

Case Report - Year 2014 - Volume 29 - Issue 2
Back-to-front flipping of an anatomical implant 31 months after augmentation mammoplasty: a case report
Rotação de trás para frente de implante anatômico após 31 meses da mamoplastia de aumento: relato de caso
ABSTRACT
INTRODUCTION: Augmentation mammoplasty is one of the most commonly performed surgical procedures by plastic surgeons. Back-to-front flipping of an implant after augmentation mammoplasty is a rare complication, occurring in 0-5% of cases.
CASE REPORT: The authors report a patient who presented with back-to-front flipping of an anatomical implant 31 months after augmentation mammoplasty.
Keywords: Breast implant; Flipping; Mammoplasty.
RESUMO
INTRODUÇÃO: A mamoplastia de aumento está entre os procedimentos mais realizados por cirurgiões plásticos. A rotação de trás para frente de implante após mamoplastia de aumento é uma complicação rara, que acontece entre 0 e 5% dos casos.
RELATO DE CASO: Os autores relatam um caso de uma paciente que apresentou rotação de trás para frente de implante anatômico após 31 meses da mamoplastia de aumento.
Palavras-chave: Implante Mamário; Rotação; Mamoplastia.
Augmentation mammoplasty was one of the most commonly performed surgical procedures by Brazilian plastic surgeons between September 2007 and August 20081. The American Society of Plastic Surgery reports an increase of 476% in mammoplasty augmentation cases between 1992 and 20002.
A prosthesis (breast implant silicone) can flip in three axes as follows, at a prevalence of up to 14%: flip as a pancake (x), bend like a door (y), and flip like a wheel (z), which is not perceived in round prostheses3.
Back-to-front flipping (as a pancake) is rare, reportedly accounting for 0-5%4-15 of cases. Diagnosis is clinically performed through physical examination of the patient and observation of possible changes in breast shape, without the need for diagnostic examinations16.
CASE REPORT
L.M. was a 29-year-old Brazilian who was employed in the area of human resources in London. She underwent augmentation mammoplasty with a retroglandular implant via the axillary approach on May 29, 2007. Anatomical silicone implants were used (high profile with microtexture; REF AX260, Perthese), which had the following measurements: volume, 260mL; width, 11.9cm; height, 12.5cm; and depth, 4.8cm.
The patient underwent the surgical procedure, performed in a day-hospital regime, without complications. A mold was used for the production of the implant.
The patient got married, had a son, and breastfed for 9 months. After 31 postoperative months without complications, on April 12, 2010, the patient contacted our service to report changes in the shape of the implant.
The implant was returned to its proper position through external manipulation. The patient was provided with guidance about the increased possibility of a second flipping, and she opted to not undergo a second surgical procedure.

Figure 1. Frontal: preoperative.

Figure 2. Frontal: at 31 postoperative months (after breastfeeding).

Figure 3. At 31 postoperative months, changes were observed in the shape of breast D, with nipple height asymmetries and anterior face alteration.

Figure 4. Details of breast D, with the patient leaning forward; a flattened aspect can be observed.

Figure 5. Profile with the anterior face alteration of breast D.
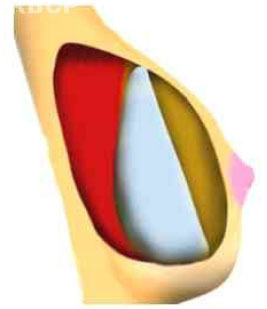
Figure 6. Schematic diagram of the back-to-front flipping of the anatomical implant, in a profile view.

Figure 7. Capsule with more than one layer surrounding the implant.

Figure 8. Example of a prosthesis with two capsules. The image depicts a capsule surrounding the implant and smoothening of the microtexture.
DISCUSSION
Although augmentation mammoplasty has been the most commonly performed surgical procedure by Brazilian plastic surgeons between September 2007 and August 20081, in our service, the cases of primary augmentation mammoplasty with implants accounted for only 5.53% of all surgical cases (n = 300). This bias may be justified by the surgical concept acquired in our service in the 1970s, when the need for surgical revision due to the poor quality of implants reached 20%. Since then, augmentation mammoplasty with breast implant began to be considered a surgery that can be performed again.
The advancements in implant design over the last 40 years focused on silicone implants with the property to not leak even if the cover of the prosthesis is perforated. When previous implant designs were used, the implant covers were observed to be not completely waterproof, thus leading to the formation of a calcified capsule. However, even today, manufacturers claim that the prosthetic cover has 5 or more layers. However, our observational experience from January 1970 to December 2010 showed that prosthetic covers are not entirely waterproof. When performing a test by pinching and twisting the prosthetic membrane, air microbubble formation was observed, which disappeared when the prosthesis was undisturbed. Moreover, all the prostheses used underwent a change in color after withdrawal and contact with air.
For such prostheses, fasteners proved to be inefficient. Rendering a wrinkled surface with pores (texture) was also ineffective, as the body recovered the texture, smoothening it. In these cases, two capsules or a capsule with several layers, instead of a single capsule, surrounded the implant. In these capsules, fluid can accumulate (in the laminar liquid layer) and possibly trigger the implant rotation3,4.
The prevalence of back- to-front flipping of an implant after augmentation mammoplasty between January 1970 and December 2010 was 0.33% per patient and 0.16% per implant in our service, indexes consistent with data already reported in the literature3-17.
Several factors such as infection, hematoma, capsular contracture, dissection, inexperience of the surgeon, physical activity, and external manipulation of the implant may contribute to the flipping of the prosthesis3,16,17. Moreover, as the rotation in the z-axis could not be observed in round prostheses, the prevalence of flipping may be higher than reported.
In our case, the implant was repositioned through external manipulation only. According to Schots et al., in 25% of cases, the implants could be returned to the normal position without manipulation; in 17% of the cases, external manipulation was necessary; and in 12% of cases, a new surgical procedure was required17. Although advised on the increased chance of a second flipping, the patient opted not to undergo a new surgical procedure. Another interesting fact is the absence of reports referring to low- or moderate-profile breast implant flipping, regardless of the texture, although the dimensions of these implants are similar to those with high and super-high profiles16.
CONCLUSION
Despite the advances in breast implant technology, we believe that breast implant designs are evolving. Therefore, research will continue.
The prevalence of back-to-front flipping of an implant after augmentation mammoplasty in our service is consistent with data reported in the literature.
Although several potential factors might have affected the mobility of the implant in the present case, the clear cause of the problem was not determined. Therefore, further studies should be performed.
Not all cases of implant flipping need surgical revision. Agreement with the patient is necessary.
REFERENCES
1. Sociedade Brasileira de Cirurgia Plástica. Pesquisa data folha SBCP. Sociedade Brasileira de Cirurgia Plástica, 2008.
2. American Society of Plastic Surgeons. The National Clearinghouse of Plastic Surgery Statistics. Arlingtom Heights, III: American Society of Plastic Surgeons, 2000.
3. Baeke JL. Breast deformity caused by anatomical or teardrop implant rotation. Plast Reconstr Surg. 2002;109:2555.
4. Panettiere P, Marchetti L, Accorsi D. Rotation of anatomic protheses: a possible cause of breast deformity. Aesthetic Plast Surg. 2004;28:348-353.
5. Tebbets JB. Warning about anatomical breast implants. Plast Reconstr Surg. 2001;107:1912-1917.
6. Hedén P, Boné B, Murphy DK, SLicton A, Walker PS. Style 410 cohesive silicone breast implants: safety and effectiveness at 5 to 9 years after implantation. Plast Reconstr Surg. 2006;118:1281-1287.
7. Brar M. Teardrop implants (Letter). Plast Reconstr Surg. 2003;111:2112.
8. Brown MH, Shenker R, Silver SA. Cohesive silicone gel breast implants in aesthetic an reconstructive breast surgery. Plast Reconstr Surg. 2005;116:768-779; discussion 780-1.
9. Heitmann C, Schreckenberger S, Olbrisch RR. A silicone implant filled with cohesive gel: advantages and disadvantages. Eur J Plat Surg. 1998;21:329-332.
10. Niechajev I. Mammary augmentation by cohesive silicone gel implants with anatomical shape: technical considerations. Aesthetic Plast Surg. 2001;25:397-403.
11. Niechajev I, Jurell G, Lohjelm L. Prospective study comparing two brands of cohesive gel breast implants with anatomic shape: 5-year follow-up evaluation. Aesthetic Plast Surg. 2007;31;697-710.
12. Bengston BP, Van Natta BW, Murphy DK, Slicton A, Maxwell GP. Style 410 highly cohesive silicone breast implant core study results at 3 years. Plast Reconstr Surg. 2007;120(1):40S-48S.
13. Cunningham B. The Mentor Core Study on Silicone MemoryGel Breast Implants. Plast Reconstr Surg. 2007:120(1):19S-29S; discussion 30S-32S.
14. Cunningham B.The Mentor Core Study on Contour Profile Gel Silicone MemoruGel Breast Implants. Plast Resconstr Surg. 2007;120(1):33S-39S.
15. Spear SL, Murphy DK, Slicton A, Walker PS. Inamed Silicone Breast Implant U.S. Study Group. Inamed silicone breast implant core study results at 6 years. Plast Reconstr Surg. 2007;120(1):8S-16S; discussion 17S-18S.
16. Khan UD. Back-to-front flipping of implants following augmentation mammoplasty and the role of physical characteristics in a round cohesive gel silicone breast Implant: retrospective analysis of 3458 breast implants by a single surgeon. Aesth Plast Surg. 2011;35:125-128.
17. Schots JM, Fechner MR, Hoogbergen MM, Van Tits HW. Malrotation of the McGhan Style 510 prothesis. Plast Reconstr Surg. 2010;126:261-265.
1 - Specialist member of BJPS and plastic surgeon at CLINCER
2 - Member of BJPS and director and plastic surgeon at CLINCER
3 - Specialist member of BJPS and plastic surgeon at CLINCER
4 - Master in Plastic Surgery by the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo and former plastic surgeon at CLINCER
5 - Former assistant at the Plastic and Reconstructive Surgery Clinic
Institutional affiliation: CLINCER (Plastic and Reconstructive Surgery Clinic S C Ltd).
Correspondent author:
André Toshiaki Toda Nishimura
Alameda Lorena, 2015 - Cerqueira César
São Paulo, SP, Brazil - CEP: 01424-002
Phone: +55-11-3062-6122
E-mail: andre_nishi@me.com
Article submitted: May 4, 2011
Article accepted : August 22, 2011


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter