

Original Article - Year 2014 - Volume 29 -
Microbiological surveillance of burn unit of EPM/UNIFESP in São Paulo, Brazil
Perfil microbiológico da unidade de queimaduras da EPM/UNIFESP, São Paulo, Brasil
ABSTRACT
INTRODUCTION: Despite great advances in treatment, burned skin infection remains a major challenge. The aim of this study is to evaluate the microbiological aspects of the first year's operation of a Burn Unit in a University Hospital.
METHODS: Retrospective study. Microbiological data were collected and analyzed from patients admitted to the Burn Unit of São Paulo Hospital, a University Hospital of the Paulista Medical School (EPM) of the Federal University of São Paulo (UNIFESP) from June 2009 to July 2010.
RESULTS: The average length of stay was 13.8 days with a mortality rate of 5.9%, and median of TBSA was 10.3%. Evaluated 159 cultures from 101 patients. Blood cultures were the most requested (41%). It was also accessed 245 surveillance cultures collected from 75 patients. The microbiological analysis revealed a total positivity rate of 34,5%. The most prevalent agents were Coagulase-negative Staphylococcus - CoNS - (33%), Pseudomonas aeruginosa (24%), Acinetobacter spp. (22%) and Klebsiella pneumoniae (5%).
CONCLUSION: The microbiological evaluation of the first year's activity of EPM/UNIFESP Burn Care Unit revealed that, although the most prevalent agent was CoNS, Gram negative bacilli are still very prevalent, such as Pseudomonas aeruginosa and Acinetobacter baumannii. Despite the short time of operation, was observed large number of multiresistant microorganisms which can be explained by long exposure to antimicrobials and high transfer rate from other hospitals.
Keywords: Burn Units; Epidemiology; Staphylococcus; Pseudomonas aeruginosa; Acinetobacter baumannii.
RESUMO
INTRODUÇÃO: Apesar dos grandes avanços em seu tratamento, infecção de pele com queimadura continua a ser um grande desafio. O objetivo deste estudo é avaliar os aspectos microbiológicos do primeiro ano de funcionamento de uma unidade de queimadura em um Hospital Universitário.
MÉTODOS: Estudo retrospectivo. Dados microbiológicos foram coletados e analisados a partir de pacientes internados na Unidade de Queimadura (UTQ) do Hospital São Paulo, Hospital Universitário da Escola Paulista de Medicina (EPM) da Universidade Federal de São Paulo (UNIFESP), entre junho de 2009 e julho de 2010.
RESULTADOS: O tempo médio de permanência hospitalar foi de 13,8 dias, com uma taxa de mortalidade de 5,9%. A média da superfície corpórea queimada foi de 10,3%. Avaliou-se 159 culturas de 101 pacientes. Culturas de sangue foram as mais solicitadas (41%). Também foram acessadas 245 culturas de vigilância, coletadas de 75 pacientes. A análise microbiológica revelou um índice de positividade total de 34,5%. Os agentes mais prevalentes foram Staphylococcus coagulase-negativo - CoNS - (33%), Pseudomonas aeruginosa (24%), Acinetobacter spp. (22%) e Klebsiella pneumoniae (5%).
CONCLUSÃO: A avaliação microbiológica do primeiro ano de funcionamento da UTQ da EPM/UNIFESP revelou que, embora o agente mais prevalente tenha sido a CoNS, bacilos Gram negativos ainda são muito prevalentes, como a Pseudomonas aeruginosa e a Acinetobacter baumannii. Apesar de pouco tempo de operação, observou-se um grande número de microrganismos multirresistentes, que pode ser explicado por longa exposição a agentes antimicrobianos e alta taxa de transferência de outros hospitais.
Palavras-chave: Unidades de Queimados; Epidemiologia; Staphylococcus; Pseudomonas aeruginosa; Acinetobacter baumannii.
Infections are major causes of mortality in severely burned patients. The United States has the highest mortality rates in patient's victims of burns among industrialized countries1. In Brazil, burns are responsible for over than 100.000 hospital admissions and 2.500 deaths per year2.Burn treatment is funded by the government and needs of epidemiological data for the correct management and publishing for prevention3.
This patients are most susceptible to developing infection, as changes occur in the immune system due to dysfunction of granulocytes, reduced numbers of circulating lymphocytes and reduction of substances such as IL-2 and IgG. The largest burn extension, the higher probability of the patient developing infection.
Studies evaluating the frequency of infections in these patients show that bloodstream infections, respiratory tract infections, urinary tract infections and skin infections are most prevalent4.
Despite great advances in treatment, burned skin infection remains a major challenge. The disruption in skin barrier, vascular changes in the tissue and immune system dysfunction contribute to infection. In addition, the wound environment is propitious to microorganism's development4.
The aim of this study is to evaluate the microbiological aspects of the first year's operation of a burn unit in a University Hospital.
METHODS
This is are trospective epidemiological study where we evaluated the microbiological data from patients admitted to the burn unit of SãoPaulo Hospital, a University Hospital of the Paulista Medical School (EPM) of the Federal University of São Paulo (UNIFESP) from June2009 to July 2010.
Thisstudy was approved by the Research Ethics Committee of EPM/UNIFESP under number 1272/10.
Opened in June 2009, the Burn Unit of São Paulo Hospital is a high complexity center with four intensive care and six ward beds and operative room in the Burn Unit. São Paulo Hospital is a University Hospital that belongs to the Paulista Medical School of the Federal University of São Paulo.
Evaluated 159 cultures from 101 patients admitted to the Burn Unit from July 2009 to June 2010.
The microbiological protocol of patient care in the burn unit is started by collecting samples from the wound, oropharyns and rectum at the patient's arrival in the burn unit. During the clinical outcome when the patient has systemic symptoms such as fever, abnormal white blood cell count, increase of PCR and other inflammatory markers, or local changes, such as discoloration of the wound, the presence of cellulitis or vasculitis, is collected culture of the wound and blood culture. When there are specific signs such as changes in the urinary, digestive, pulmonary systems, most common sources of infection, among several, specific cultures are required for diagnosis.
Microbiological data were analyzed considering the culture requested, prevalent agents and antimicrobial susceptibility. All cultures were processed at Microbiology Central Laboratory from São Paulo Hospital. The microorganism identification and susceptibility tests for antimicrobial drugs were processed by automated system (Phoenix - BD®). The interpretative criteria's for break points definition to the susceptibility followed the CLSI standards (Clinical Laboratory Standards Institute) document M100-S19.
Patient and burn's characteristics such sex, age, total body surface area (TBSA), surgical procedures, injury severity were also evaluated by epidemiologic form filled out during patient's hospitalization.
Clinical features assessed considered average hospital stay between admission and surgery, burn infection and graft lost.
Burn infection is defined by the invasion of microorganisms in the area of the burn injury with the presence of signs such as discoloration, from points of vasculitis, points or plaques blackened in the subcutaneous tissue, presence of cellulitis around the lesion, secretion on the lesions and systemic repercussions with abnormal laboratory tests. Graft skin loss is when the skin does not take by the presence of exudate or other serous solution between the graft and the recipient site. This can occur by local conditions of the recipient site or the systemic conditions of the patient, more often as a septic shock.
Statistical analysisof results was obtainedby SPSS software.
RESULTS
From June 2009 to July 2010, 101 patients were admitted at the Burn Unit. During this period an epidemiological study was performed and revealed that the average age of patients admitted was 33.7 years and they were male in 66.7% of admissions3.
The average length of stay was 13.8 days with a mortality rate of 5.9%. The median of TBSA was 10.3% and 64.3% were regarded as small burns (Table 1). The mean time to surgery (debridement or grafting) was 4.4 days.
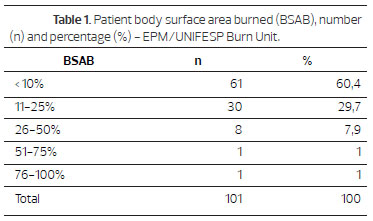
During the studied period, the average of surgeries per month was 9.1. Debridement and skin grafting, in distinct surgical moments, were the most common procedures, respectively 39 (35.4%) and 37 (33.6%) (Table 2).
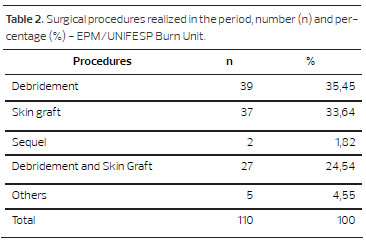
From June 2009 to July 2010, 159 cultures were requested when infection was suspected. Blood cultures were the most requested (41%), followed by urine culture (18%), quantitative skin biopsy (14%w) and catheter tip (11%), as shown in Figure 1.
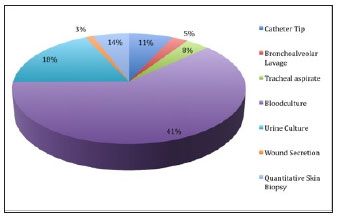
Figure 1. Type of cultures requested when infection was suspected at EPM/UNIFESP Burn Unit
It was also accessed 245 surveillance cultures collected from 75 patients with distribution of site collection and isolated microorganisms (Figures 2 and 3).
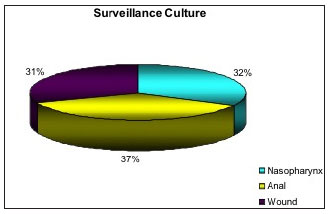
Figure 2. Distribution of site collection in surveillance cultures at EPM/UNIFESP Burn Unit.
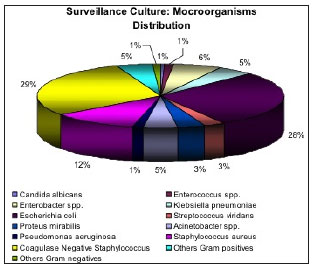
Figure 3. Distribution of microorganisms isolated in surveillance cultures at EPM/UNIFESP Burn Unit.
When it was evaluated the surveillance cultures, it was found a prevalence of Coagulase Negative Staphylococcus, Escherichia coli and Staphylococcus aureus.
Only one (0,45%) E. coli isolate presented extended-lactamase production (ESBL) with resistance to cephalosporins and one (0,45%) isolate of Pseudomonas aeruginosa presented multi-resistant susceptibility profile.
Among Gram positives, was founded 26% and 5% of resistance to oxacilin in CoNS and S. aureus respectively.
The microbiological analysis revealed a total positivity rate of 34,5%. figure 4 shows the positivity rate according the culture requested.
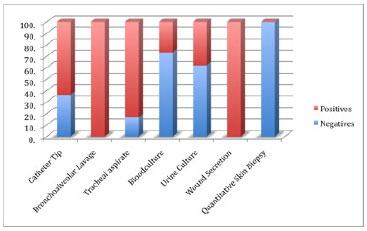
Figure 4. Positivity rate according the culture requested at EPM/UNIFESP Burn Unit.
The most prevalent agents were Coagulase-negative Staphylococcus - CoNS -(33%), Pseudomonas aeruginosa (24%), Acinetobacter spp. (22%) and Klebsiella pneumoniae (5%), according figure 5.
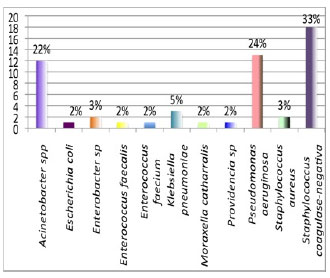
Figure 5. Microorganism's distribution in positive cultures at EPM/UNIFESP Burn Unit.
The analysis of antimicrobial susceptibility tests demonstrated that 83% of CoNS were resistant to oxacilin. Regarding Pseudomonas aeruginosa and Acinetobacter spp., 85% and 50% respectively were multi-resistant. It was found one Klebisiella pneumoniae isolate resistant to carbapenems and positive to Modified Hodge Test (possible carbapenemase producing strain).
DISCUSSION
Our epidemiological data revealed a male prevalence (66,7%) and median age of 33.7 years. Similar results were found in several studies in different countries5-9.
Studies show thatmales are exposed to work activities with higherrisk for accidents such ashandling equipments or chemicals, fuel, laborandelectricitynetworks3,10.
Regarding total body surface area (TBSA), the average percentage was 11.3%, a value close to the study conducted in Lithuania from 1991 to 2004, which averaged found was 9.6%11.Most of the burn extension was considered small, between 0 and 10% of BSA in 62 (61.4%) patients, coinciding with other studies with rates of 60.0% and 57.0% respectively6,10.
Inhalation injury was associated with six deaths, and the one-year mortality rate was 5.9%, higher than the study conducted by Onarheim et al. (2,1%), and Brusselaers et al.(14%)7,8.However, similar result was found at Macedo and Rosa's Brazilian study, with 6.2% mortality rate5.
In severely burned patients, the diagnostic of infection is extremely difficult, once inflammatory response can either cause symptoms like fever and hypotension, with increase in white blood cell account and in C-Reactive Protein (CRP). Therefore, cultures are important tools for the diagnosis of infection.
The most request culture in our service was blood culture (41%) with a posivity rate of 26.5%, followed by urine culture (18%) with positivity rate of 38% and quantitative skin biopsy (14%) with a posivity rate of 0%. Catheter tip was the fourth culture most requested, positive in 63,6%. In one study conducted in Turkey, among 169 burned patients, 127 acquired and 166 nosocomial infection (15.7% pneumonia, 56.0% BWI, 8.4% UTI and 19.9% BSI for an overall NI rate of 18.2 per 1000 patient-days)12.
A total of 55 microorganisms were isolated from 159 cultures. The most prevalent agents were Coagulase-negative Staphylococcus - CoNS -(33%), Pseudomonas aeruginosa (24%), Acinetobacter spp. (22%) and Klebsiella pneumoniae (5%). Except for the CoNS, a similar result was found at ONCUL's study12. GUGGENHEIM et al. (2009) conclude dinamicrobiological study with burned patients, from 1986 to 2005, that Staphylococcusaureus was isolated mostoften, 20.8%, followed by Escherichiacoliwith3.9%, 11.8% with Pseudomonasaeruginosa, coagulase-negative (SCN) with 10.9%, Enterococcussp. with 9.7%, 5.6% Enterobacter cloacae, Klebsiella pneumoniae 5%, Acinetobactersp. 3.2%, Proteusmirabiliswith 2% and Stenotrophomonasmaltophiliaat 1.4%13.
Our analysis showed that CoNS was the most prevalent agent, mainly from blood cultures. However, it is difficult to assess the clinical importance of these pathogens as responsible for causing infection once they are also associated to skin colonization.
Although the low prevalence of Acinetobacter baumannii in burned patients according some authors, at São Paulo Hospital it was the most isolated. The Brazilian Scope Project evaluated the blood stream infection agent's prevalence and revealed a high incidence by this agent.
Pseudomonas aeruginosa is an important causative agent of infection in burns, especially skin infections. The presence of this agent is associated with high mortality rates. In this study, it was the second most prevalent agent although it has not been associated with skin infection in the sample assessed.
MEN'SHIKOV et al. (2009) in a specialized center for burn treatment, studied 3,179 samples of exudates from wounds and 6,501 strains of microorganisms that affect the wounds and noted that the most prevalent was Staphylococcus aureus14.
At EPM/UNIFESP Burn Unit, wound secretion culture's is not recommended for routine diagnosis of infection, since it may represent colonization. The quantitative culture of a skin biopsy is the better choice to evaluate the suspecting infection.
Among 101 patients, 9 quantitative burn skin biopsy was request. None had growth of microorganisms in a significant account (> 105 UFC) and none of patients evaluated with burn skin infections. Maybe this could be attributed for the early debridement and skin graft (mean time to surgery 4.4 days).
Studies show thatearly surgical treatment of burned patients with debridementand application of skin grafts, prevents biofilm formation, colonization, skin infectionand sepsis. It has been demonstrated, effective essin reducing complications, reducing mortality rates, length of stayand number ofsurgeries15-17.
AtEPM/UNIFESP Burn Care Unit, stringent measures area doptedin the care of burn swith daily dressing changes, wound cleaning, disinfection and use oftopical antimicrobials. GRAGNANI et al. (2005) have reported that adoption of these measure sencourages a moist environment conduciting to wound healing, mainlysuperficial18.
The susceptibility tests to antimicrobials showed a high frequency of multidrug-resistant microorganisms in our unit, represented mainly by Acinetobacter baumannii and Pseudomonas aeruginos are sistants to carbapenems(85% and50% respectively).From the analysed samples only one isolate of Klebsiella pneumoniae was resistant to carbapenem swith-Hodge test positive suggesting a possible carbapenemase production.
Despite the short time drive activity of the EPM/UNIFESP Burn Care Unit, the patients studied are exposed to long periods of antibiotic therapy, which increases the selective pressure for resistant organisms(average length of stay of 13.8 days). Moreover, it is are ferral service tha treceives patients from other services(30.6%).
There ate of wound infection in burns was 0%, disagreeing with the literature. The surgical procedures(early debridementand grafting) associated with wound care such as daily dressings and topical antimicrobials, may explain the results founded.
CONCLUSIONS
The most prevalent agent was Coagulase-negative Staphylococcus in the microbiological evaluation of the firsty ear's activity of EPM/UNIFESP Burn Care Unit. Although this agent was responsable for a third of the analised cases, Gram negative bacilli, such as Pseudomonas aeruginosa and Acinetobacter baumannii, are still very prevalent, being identified in approximately half of the cultures. The long exposure to antimicrobials and high transferrate from other hospitals can explain the large number of multi resistant microorganisms in the sudy.
ACKNOWLEDGEMENTS
We would like to thank the people responsible for the inauguration of the Burn Unit, especially the efforts of our full professor, Profa. Dra. Lydia Masako Ferreira; and the NGO Pró-Queimados Institute, in particular Ms. Mira Falchi; and the Paulista Medical School/Federal University of São Paulo (EPM/UNIFESP) and the Paulista Association for the Development of Medicine (SPDM). We would like to thank also the people from the Central Laboratory of São Paulo Hospital and all professionals working in the Burn Unit of EPM/UNIFESP. And a special thank to the patients.
Author Disclosure Statement
None of the authors has competing financial interests to disclose.
REFERENCES
1. Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn Wound Infections. Clin Microbiol Rev. 2006;19(2):403-34.
2. Souza AA, Mattar CA, Almeida PC, et al. Epidemiological profile of patients admitted at Burn Unit Servidor Público Estadual de São Paulo Hospital. Rev Bras Queimaduras. 2009;8(3):87-90.
3. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Epidemiological Study of the Federal University of São Paulo Burn Unit. Rev Bras Queimaduras. 2010:82-8.
4. Rafla K, Tredget EE. Infection control in the burn unit. Burns. 2011;37:5-15.
5. Macedo JLS, Rosa SC. Estudo epidemiológico dos pacientes internados na Unidade de Queimados: Hospital Regional da Asa Norte, 1992-1997. Brasília Med. 2000;37:87-92.
6. Cavalcanti AL, Martins VM, Lucena RN, Granville-Garcia AF, Menezes VA. Morbidade por causas externas em crianças e adolescentes em Campina Grande, Paraíba. Arq Catarin Med. 2008;37:27-33.
7. Onarheim H, Jensen SA, Rosenberg BE, Guttormsen AB. The epidemiology of patients with burn injuries admitted to Norwegian hospitals in 2007. Burns. 2009;35:1142-6.
8. Brusselares N, Juhasz I, Erdei I, Monstrey S, Blot S. Evaluation of mortality following severe burns injury in Hungary: external validation of a prediction model developed on Belgian burn data. Burns. 2009;35(7):1009-14.
9. Taghavi M, Rasoouli MR, Boddouhi N, Zarei MR, Khaji A, Abdollahi M. Epidemiology of outpatient burns in Tehran: An analysis of 4813 cases. Burns. 2009;36:109-13.
10. Miranda RE, Pacannaro RC, Pinheiro LF, Calil JA, Gragnani A, Ferreira LM. Trauma elétrico: análise de 5 anos. Rev Bras Queimaduras. 2009;8:65-9.
11. Rimdeika R, Kazanavicius M, Kubilius D. Epidemiology of burns in Lithuania during 1991-2004. Medicina (Kaunas). 2008;44(7):541-7.
12. Oncul O, Ulkur E, Acar A, et al. Prospective analysis of nosocomial infections in a Burn Care Unit, Turkey. Indian J Med Res. 2009;130:758-64.
13. Guggenheim M, Zbiden R, Handschin AE, Gohritz A, Altintas MA, Giovanoli P. Changes in bacterial isolates from burn wounds and their antibiograms: a 20-year study (1986-2005). Burns. 2009;35(4):553-60.
14. Men'shikov DD, Godkov MA, Chernen'kaia TV, et al. Mono- and associated microflora during wound infection in patients with burns. Zh Mikrobiol Epidemiol Immunobiol. 2009;(6):3-7.
15. Ramzy PI, Barret JP, Herndon DN. Thermal injury. Crit Care Clin. 1999;15(2):333-52.
16. Alvarez-Díaz C, Cuenca-Pardo J, Sosa-Serrano A, Juárez-Aguilar E, Marsch-Moreno M, Kuri-Harcuch W. Controlled clinical study of deep partial-thickness burns treated with frozen cultured human allogeneic epidermal sheets. J Burn Care Rehabil. 2000;21(4):291-9.
17. Kennedy P, Brammah S, Wills E. Burns, biofilm and a new appraisal of burn wound sepsis. Burns. 2010;36(1):49-56.
18. Gragnani A, Gonçalves ML, Ferreira LM. Microbiological analyses in burns. Rev Bras Cir Plást. 2005;20(4):237-40.
1 - MD, Phd - Professor Of Plastic Surgery Division Of EPM/UNIFESP
2 - MD, Phd - Assistant Of Infectology Division Of EPM/UNIFESP
3 - MD, Fellow Master Degree - Infectology Post Graduate Program, EPM/UNIFESP
4 - Medical Student Of EPM/UNIFESP - Medical Student Of EPM/UNIFESP
5 - Nurse, Fellow Master Degree - Plastic Surgery Post Graduate Program, EPM/UNIFESP
6 - MD, Phd - Head Of Central Laboratory Of São Paulo Hospital
7 - MD, Phd - Chairwoman, Full Professor Of Plastic Surgery Division Of EPM/UNIFESP, São Paulo/São Paulo/Brazil
Institution: Disciplina de Cirurgia Plástica da Escola Paulista de Medicina- Unifesp - SP, UNIFESP/EPM.
Corresponding author:
Alfredo Gragnani
Division of Plastic Surgery of EPM/UNIFESP
Rua Napoleão de Barros, 737- 4º andar Vila Clementino
São Paulo/SP - Brazil 04024-000
E-mail: alfredogf@ig.com.br
Article received: October 7, 2013
Article accepted: December 8, 2013


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter