

Original Article - Year 2014 - Volume 29 - Issue 1
Secondary omphaloplasty: description of a new proposal
Onfaloplastia secundária: descrição de uma nova proposição
ABSTRACT
INTRODUCTION: The navel is an essential component of abdominal aesthetics. Omphaloplasty sequelae can compromise the result of an abdominal abdominoplasty. The purpose of this article was to propose an alternative procedure that is simple to perform and well accepted by patients, with favorable cosmetic results.
METHODS: We surveyed cases of abdominal dermolipectomy in teaching hospitals and in private practice in the last 5 years (433 cases).
RESULTS: We found 30 cases (6.9%) of sequelae distributed as follows: 14 cases (3.2%) in the hypogastric scar and 16 cases in the umbilicus (3.8%). They are characterized as follows: 7 cases (1.6%) of constriction of the navel and 9 cases (2.07%) of scar hypertrophy.
CONCLUSION: We analyzed the results of the proposed technique of secondary omphaloplasty in the immediate (up to 30 days) and late (1-year) postoperative periods.
Keywords: navel; reconstruction; scar; surgery; treatment; omphaloplasty.
RESUMO
INTRODUÇÃO: O umbigo é um componente essencial à estética do abdome. Sequelas de onfaloplastia podem comprometer o resultado final de uma dermolipectomia abdominal. Objetivo do trabalho é propor um procedimento alternativo, de fácil execução, com resultado estético favorável e bem aceito pelas pacientes.
MÉTODOS: Fizemos o levantamento dos casos de dermolipectomia abdominal operados no serviço de ensino e na clínica privada nos últimos cinco anos (433 casos)
RESULTADOS: Encontramos 30 casos (6,9%) com sequelas, assim distribuídos: 14 casos (3,2%) na cicatriz hipogástrica, e 16 casos de sequelas de umbigo (3,8%), assim caracterizados: sete casos (1,6%) constrição de umbigo e nove casos (2,07%) hipertrofia cicatricial.
CONCLUSÃO: Analisamos os resultados da técnica de onfaloplastia secundária proposta quanto ao pós-operatório imediato (até 30dias) e tardio (um ano).
Palavras-chave: umbigo; reconstrução; cicatriz; cirurgia; tratamento; onfaloplastia.
In our study of cases of abdominal dermolipectomy surgery in the last 5 years (in teaching hospitals and private clinics), we found 433 surgery cases distributed as follows: classic technique, 228 cases (52.6%); lipoabdominoplasty (Saldanha technique), 94 cases (21.7%); anchor technique (post-bariatric), 56 cases (12.9%); secondary technique, 16 cases (3.8%); and mini-lipoabdominoplasty (lip shape technique), 39 cases (9.0%; total, 100%; Figure 1).
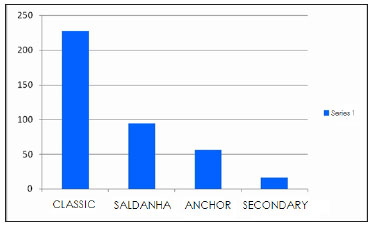
Figure 1. Distribution chart of the techniques used in the 433 cases
Within the secondary surgeries, from our own statistics and those of other services, we found cases of vicious periumbilical scars and navel constriction. As the navel is an essential component of the abdomen, such sequelae affect the result of proper abdominal surgery 1.
A number of different techniques have been used for cosmetic reconstruction to improve the appearance of a cicatrix of the navel 2,6. The subject is still under discussion, as an ideal solution is yet to be found. This paper proposed a new procedure that is simple to perform and offers acceptable cosmetic results.
Among the 433 cases studied, we found 30 cases (6.9%) with sequelae distributed as follows: 14 cases (3.2%) in hypogastric cicatrix and 16 cases of sequelae in the navel (3.8%) characterized by 7 cases (1.6%) of constriction of the navel and 9 cases (2.07%) of navel scar hypertrophy (Figure 2).
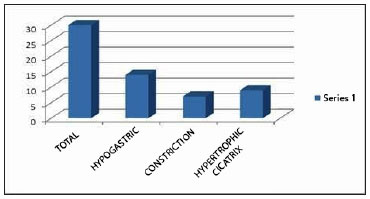
Figure 2. Chart of the sequelae found
The immediate postoperative results (up to 30 days) were the following:
Constriction of the navel: improvement of 90% compared with that in the preoperative period.
Navel scar hypertrophy: improvement of 80% compared with that in the preoperative period.
Late postoperative results (1 year) showed the following:
Constriction of the navel: persistence of 70% of the immediate result compared with that in the preoperative period.
Navel scar hypertrophy: greater than 50% improvement compared with that in the preoperative period (Figure 3).
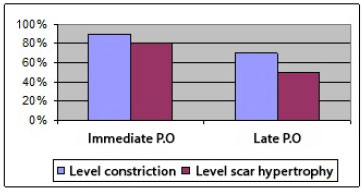
Figure 3. Evolution of results in 1 year
For these reasons, this paper aims to propose an alternative procedure, easily performed and well accepted by patients, with favorable cosmetic results.
METHODS
Surgical Technique
In the classic abdominoplasty or lipo-abdominoplasty, scars result in the upper pubic and periumbilical regions 5. If an unfavorable evolution of the navel scarring occurs (stenosis, keloids, and hypertrophic scars), the intention is to improve its appearance for better abdominal harmony3,4,5.
With the goal of minimizing the problem of circular scars, we sought to distribute the centrifugal force of the scar, widening the area of contact of the skin on the abdomen with the umbilical stump, delimiting two semicircles (variant 1) or making a triangle with a larger base (variant 2 as shown in Figure 4A and B).
Figure 4 (A): Variant 1

Figure 4 (B): Variant 2
Based on variant 2, the delimited area is decorticated with the isolation of the navel and slimming of the periumbilical fat to achieve the cosmetic sinking of that region (Figure 5A and B).

Figure 5(A): Decortication of the abdominal skin

Figure 5(B): Retro-umbilical defatting
With retro-umbilical defatting, postoperative aesthetic sinking of that region can be achieved, which enhances the result.
In variants 1 and 2, fixation of the decorticated area follows. The internal part of the semicircle is attached in the abdominal aponeurosis, with simple cardinal stitches by using a mononylon 3.0 suture. The umbilical stump skin is then enmeshed with the skin of the abdominal wall, with Perseu Lemos stitches by using a mononylon 4.0 suture (Figure 6A and B).

Figure 6(A): Deep fixation of the internal edge. Overlapping of the proximal pole.

Figure 6(B): Deep fixation of the internal edge. Overlapping of the distal pole.
In this way, all the tension of the umbilical scar will be distributed between the aponeurosis fascia and the navel skin plane in the abdominal wall. This fixation is performed with simple, separated stiches of nylon 3.0. Through this procedure, the tension on the superior skin fascia is minimized to achieve a final aesthetic result in the late postoperative period (Figure 4A and B).
This type of overlapping in the dermis of the umbilical stump brings a wider area of cicatrix contact to minimize umbilical stenosis, which occurs in traditional omphaloplasty techniques with circular scars (Figure 8).
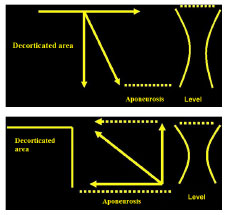
Figure 7(A) and (B): Distribution of tension in the resulting scar.
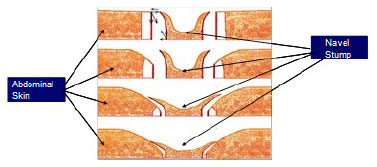
Figure 8. Distribution of forces of the umbilical stump in the surrounding skin.
RESULTS
The results were evaluated and compared between the immediate (up to 30 days) and late postoperative periods (after 1 year) in patients who had undergone classic techniques of dermolipectomy and lipoabdominoplasty. The evaluations considered the percentiles of improvement and relapses.
We illustrate the results of this study in Figure 1, comparing the preoperative aspects with the immediate and late results in two patients (scar hypertrophy and umbilical constriction).
Patient 1: Umbilical cicatrix hypertrophy Figure 9: A, B, and C

Figure 9(A): Preoperative picture of a patient with umbilical scar hypertrophy.

Figure 9(B): Postoperative appearance after 30 days.

Figure 9(C): Postoperative appearance after 1 year.
Patient 2: Umbilical constriction. Figure 10: A, B, and C.

Figure 10(A): Preoperative picture of a patient with umbilical constriction.

Figure 10(B): Postoperative appearance after 2 weeks.

Figure 10(C): Postoperative appearance after 1 year.
DISCUSSION
Although abdominoplasty is a technique that aims to produce a great degree of acceptability, an unsightly umbilical scar can compromise the result of the surgery1. The idea of broken incisions, which was proposed by Avelar (incision in the umbilical skin in the shape of a "Y"), reduced the incidence of stenosis that resulted from the circular incisions1,3
The application of other techniques that avoid that unpleasant aspect is still a challenge for most plastic surgeons. That assumption, far from offering a final solution to that problem, is based on the principle of the distribution of forces in two directions, one horizontal and one vertical, minimizing the risk of relapses and complications.
The distal result of the suture of the decorticated area in the abdominal aponeurosis will tend to unite the medial edge of the decorticated tissue to the abdominal aponeurosis, whereas the proximal result will tend to push the abdominal skin against the umbilical stump skin (Figure 8). Those resulting from the liberated umbilical stump will also undergo the action of this distribution, where its vertical component pushes the same up, allowing for a looser stump, with no tension and with its horizontal component bringing even closer the abdominal skin, which is already almost completely overlapped (dotted arrow; Figure 7 A and B).
Thus, tension distribution of the scar to the aponeurosis fascia of the umbilical stump can be achieved, allowing a more favorable aesthetic result.
CONCLUSION
Our evaluation compared immediate (up to 30 days) and late postoperative results (after 1 year; Figure 3).
Even today, achieving excellent results in abdominal abdominoplasty continues to be a challenge for plastic surgeons. This led us to the current proposition based on the principle of force distribution. We selected 16 cases, among a universe of 433 surgery cases, for this comparative study.
REFERÊNCIAS
1. Avelar J. Cicatriz umbilical da sua importância e da técnica de confecção nas abdominoplastias. Rev Bras Cir. 1979;69(1-2)41-52.
2. Franco T, Franco D. Neo-omphaloplasty- an old and new technique. Aesthetic Plast Surg.1999;23(2)-151-4.
3. Baroudi R, Carvalho C. Neoumbilicoplastias. Um procedimiento ecletico em el transcurso de las abdominoplastias. Cir Plast Iberolatinoam. 1981;7(4)-391-401.
4. Hakme F. Abdominoplasty-peri and supra-umbilical lipectomy. Aesthetic Plast Surg.1983;7(4)-213-20.
5. Franco T, Bognossian LC, Silva ALB.- Neo-onfaloplastia. Rev Bras Cir.1985;75(4)-257-60.
6. Borges AF. Recontruction of the umbilicus. BR J Plast Surg. 1975;28-75.
1- Member of the SBCP - Regent of integrated services Plastic Surgery Hospital Ipiranga
2- Member of the SBCP - Medical
3- Resident - Medical
Institution: Serviços integrados de Cirurgia Plástica - Ipiranga Hospital - São Paulo.
Corresponding Author:
Aymar Edison Sperli
Avenida Açocê 174
CEP: 04075-020
Tel: (11) 5051-4533
e_mail: aymar.sperli@uol.com.br
Article received: November 11, 2011
Article accepted: December 8, 2011


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter