

Original Article - Year 2013 - Volume 28 -
Breast reconstruction: an analysis of the new trends and major complications
Reconstrução mamária: análise de novas tendências e suas complicações maiores
ABSTRACT
INTRODUCTION: Because of its high incidence, breast cancer becomes a major concern, justified by psychological and social impacts. The purpose of the study is to analyze the current trends for breast reconstruction and evaluate its major complications.
METHOD: A retrospective study was performed in a consecutive series of breast reconstructions in the period February 2011 to February 2012, through analysis of medical records.
RESULTS: A total of 127 breast reconstructions were performed. The immediate reconstructions represent 73% of the total. The following techniques were used: permanent silicone implant, 54% (n = 69), Becker adjustable implant, 14% (n = 17), transverse rectus abdominis myocutaneous flap (TRAM), 13% (n=17), latissimus dorsi flap and implant 13% (n=16) and single expander 6% of cases (n=8). Major complications occurred in 16.5% (n = 21) and most (63% n=12) had a history of radiation therapy, neoadjuvant chemotherapy and / or smoking history. The complications resulted from hematoma reoperation (0.72% n=1), extensive necrosis of the flap requiring debridement and / or positioning of the implant to recover the lost volume (4% n=5), infections (3 % n=4), extrusion and removal of the implant (7% n=9) and thromboembolic events (1.5% n=2).
CONCLUSION: The choice of technique for breast reconstruction must be individualized and based on the characteristics and desires of each patient, the familiarity of the technique by the surgical team, the hospital resources available and costs generated by the techniques to optimize the results, reduce costs and complication rates.
Keywords: Mastectomy. Mammaplasty. Reconstructive Surgical Procedures/Methods. Mammaplasty/Trends.
RESUMO
INTRODUÇÃO: Em razão da sua elevada incidência, o câncer de mama torna-se uma das grandes preocupações, sobretudo pelos impactos psicológicos e sociais. Os objetivos do presente trabalho são analisar as tendências atuais para a reconstrução mamária e avaliar suas complicações maiores.
MÉTODO: O estudo retrospectivo foi realizado numa série consecutiva de reconstruções mamárias, no período de fevereiro de 2011 a fevereiro de 2012, pela análise de prontuários médicos.
RESULTADOS: Um total de 127 reconstruções mamárias foram realizadas. As reconstruções imediatas representam 73% do total. As seguintes técnicas foram utilizadas: implante de silicone permanente, 54% (n=69), implante ajustável de Becker, 14% (n=17), retalho transverso do músculo reto abdominal (TRAM), 13% (n=17), retalho do músculo latíssimo do dorso com implante, 13% (n=16), e expansor simples, 6% dos casos (n=8). Complicações maiores ocorreram em 16,5 % (n=21) sendo que na maioria (63% n=12) possuíam passado de radioterapia, QT neoadjuvante e/ou história de tabagismo. As complicações foram decorrentes de hematoma com reintervenção / reinternação (0,72% n=1), necrose extensa do retalho com necessidade de desbridamentos e/ou posicionamento de implante para recuperação do volume perdido (4% n=5), infecções (3% n=4), extrusão e retirada do implante (7% n=9), e eventos tromboembólicos (1,5% n=2).
CONCLUSÃO: A escolha da técnica para a reconstrução mamária deve ser individualizada e baseada nas características e anseios de cada paciente, na familiaridade da técnica pela equipe cirúrgica, nos recursos hospitalares disponíveis e nos custos gerados pelas técnicas, a fim de otimizar os resultados, reduzir custos e os índices de complicações.
Palavras-chave: Mastectomia. Mamoplastia. Procedimentos Cirúrgicos Reconstrutivos/Métodos. Mamoplastia/Tendências.
Breast aesthetics impact all spheres of the society, including science, religion, and art. Breast cancer is the most prevalent cancer among Brazilian women. The National Cancer Institute reported that in 2012, an estimated 52,680 women developed breast cancer1. Because of its high incidence, breast cancer is a major concern, especially considering its psychological and social impacts on women's health; suffering from prejudice as well as living with a stigmatized illness and the continuous uncertainties and possibility of recurrence are undesirable.
Mastectomy is one of the most common treatments for breast cancer. However, mastectomy and adjuvant therapies contribute to the development of physical complications and psychological disorders, which may negatively influence quality of life2,3. Breast removal changes a woman's body image, provokes feelings of being mutilated, and results in a loss of femininity and sensuality.
In order to reduce the negative feelings triggered by this disease and its treatment, improve self-esteem, overcome the absence of the breasts, and facilitate wearing clothes, many women opt for breast reconstruction surgery. This is a safe procedure and does not increase the risk of disease recurrence, interfere with disease detection, or delay adjuvant therapies2,3. Breast reconstruction surgery is becoming a common procedure in society; it is requested by a significant proportion of the female population. Many women who are young and employed opt for reconstruction. Plastic surgeons play an essential role by helping these patients to return to normal lives, restoring their self-esteem and appearance2,3.
Although 35-40% of the women annually diagnosed with breast cancer undergo total mastectomy, less than 25% are submitted to immediate reconstruction4-6. Albornoz et al.4 report 2 interesting findings: (1) the immediate reconstruction rate is 37.8%; (2) there are more reconstructions using implants than autologous tissue (61% vs. 41%, respectively). These findings differ from those in the literature. New reconstruction procedures using alloplastic implants (i.e., expanders, adjustable, and permanent implants) and autologous or conventional free flaps have expanded the surgeon's toolkit. Nevertheless, it is essential is to select a technique according to the patient's characteristics and needs in order to achieve satisfactory outcomes.
Accordingly, this study analyzed the current trends of breast reconstructions performed in a reference plastic surgery service and assessed the major complications of these treatments.
METHOD
This retrospective study analyzed the medical records of a consecutive series of breast reconstructions performed by the plastic surgery team of Felício Rocho Hospital, Belo Horizonte, MG, Brazil between February 2011 and February 2012.
The patients included in this study underwent extended or total mastectomy, or areola-papilla complex (APC)-sparing mastectomy followed by immediate or late breast reconstruction.
Information including age, tumor type, time of reconstruction (i.e., immediate vs. late), the reconstruction procedures used, and major complications were collected.
Major complications were defined as those requiring re-hospitalization or re-intervention within 3 months after reconstruction owing to surgery-related complications.
RESULTS
A total of 127 breast reconstructions were performed in 118 patients between February 2011 and February 2012.
The average age of the patients was 51.4 years (range: 25-81 years); 49% were younger than 50 years.
The indications for mastectomy followed by immediate reconstruction (n = 93) were as follows: unifocal invasive ductal carcinoma (40%), in situ ductal carcinoma (20%), multifocal/multicentric ductal carcinoma (17%), invasive lobular carcinoma (16%), mixed carcinoma (4%), and mucinous carcinoma (3%).
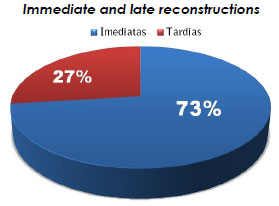
Graph 1 - Immediate and late reconstructions accounted for 73% (n = 93) and 27% (n = 34) of all cases, respectively .
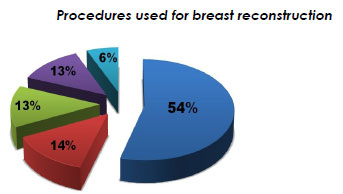
Graph 2 - Procedures used for breast reconstruction and respective percentages .
Immediate and late reconstructions accounted for 73% (n = 93) and 27% (n = 34) of the total cases, respectively. The average time elapsed between mastectomy and late reconstructions was 27 months.
Among all reconstructions, 66% were primary, i.e., there were no prior reconstruction attempts; meanwhile, 34% were secondary, i.e., they followed a previous reconstruction attempt. When immediate reconstructions performed with implants were evaluated separately, 64% were primary surgeries and 36% were conservative reconstructions. Among only autologous flaps, 51% were primary reconstructions.
Breast reconstructions were performed using permanent silicone implants, Becker adjustable implants, transverse rectus abdominis muscle (TRAM) flap, latissimus dorsi muscle flap with implants, and simple expanders in 54% (n = 69), 14% (n = 17), 13% (n = 17), 13% (n = 16), and 6% (n = 8) of cases, respectively. Among autologous reconstructions, 64%, 24%, and 12% of TRAM flaps were contralateral unipedicle, ipsilateral unipedicle, and bipedicle, respectively. Latissimus dorsi muscle flaps were used in combination with permanent and adjustable implants, and simple skin expanders in 62% (n = 10), 31% (n = 5), and 6.25% (n = 1) of cases, respectively.
Among mastectomies followed by immediate reconstructions with permanent or adjustable implants (n = 86), the APC was preserved in 34% (n = 29) of cases. Among patients who underwent adenomastectomy with APC preservation, 2 (6.8%) were submitted to APC amputation, including 1 during surgery, because the frozen cut was positive for malignancy, and the other after reconstruction, because the APC was positive for malignancy according to the final pathological examination (Figs. 1-4).

Figure 1 - Left adenomastectomy with areola-papilla complex (APC) preservation and immediate reconstruction with a permanent implant. A and B: immediate post-operative period. C: late postoperative period.

Figure 2 - Immediate reconstruction with a permanent implant without areola-papilla complex (APC) preservation. Immediate preoperative and postoperative periods, respectively.

Figure 3 - Reconstruction with a latissimus dorsi muscle flap. Immediate preoperative and postoperative periods, respectively.

Figura 4 - Right breast reconstruction with a contralateral unipedicle myocutaneous transverse rectus abdominis muscle (TRAM) flap.
Among immediate breast reconstructions, 10% (n = 9) were bilateral and 5% (n = 5) were followed by immediate symmetrization.
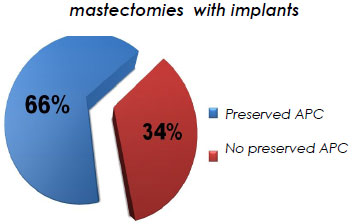
Graph 3 - Percentage of followed by immediate reconstruction with permanent or adjustable implants (n = 86). The areola-papilla complex (APC) was preserved in 34% (n = 29) of cases.
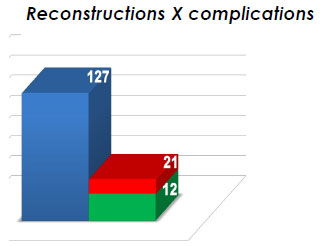
Graph 4 - Major complications occurred in 16.5% (n = 21) of the total ; most patients (63%, n = 12) had a history of radiotherapy, neoadjuvant chemotherapy (CT), and/or smoking.
The average implant volumes in reconstructions with latissimus dorsi muscle flap, and immediate reconstructions with permanent and adjustable implants were 333, 429, and 579 cm3, respectively. The average hospitalization duration was 2.6 days in cases with no complications (n = 106). In cases with major complications, i.e., cases requiring reintervention or re-admission, the average hospitalization duration was 12 days, with an average of 2.1 and 1.4 re-admissions and re-interventions per patient, respectively (n = 21).
Major complications occurred in 16.5% (n = 21) of all reconstructions; most patients (63%, n = 12) had a history of radiotherapy, neoadjuvant chemotherapy and/or smoking. Complications were due to the formation of a hematoma requiring re-intervention/re-hospitalization (0.72%, n = 1), extended flap necrosis requiring debridement and/or implant positioning to recover the loss of volume (4%, n = 5), infections (3%, n = 4), and extrusion and implant removal (7%, n = 9). In addition, there were 2 thromboembolic episodes (1.5%) including 1 case of unilateral deep venous thrombosis of the lower limb and 1 case of arterial thrombosis occurring at the bilateral bifurcation of the iliac arteries caused by tamoxifen administration; the latter case was treated by unclogging with a Fogarty catheter, and no further complications occurred.
DISCUSSION
Immediate breast reconstruction with implants was developed in the 1980s, with the reduction of aggressive breast cancer therapy. The resultant improvements in cancer surgery procedures allowed the preservation of more skin and pectoral muscle, thus facilitating the indications for breast reconstruction. Improving patients' quality of life and reducing feelings of mutilation caused by cancer treatment were also emphasized in order to facilitate their return to normal activities. In the last 11 years in the US, the rate of immediate breast reconstructions has increased 5%4-6. In this study, immediate reconstructions were predominant (73%), thus corroborating current the trend, which is affected by multiple factors. Existing legislation in the US (i.e., The Women's Health and Cancer Rights Act) and Brazil ensure women have the right to undergo breast reconstruction in both public (Law number 9.797/99) and private/contracted practice (regulated by Law number 9.656/98, amended in Law number 10.223/01). Although the direct cause of the increasing rate of reconstruction after the adoption of these laws is difficult to establish, the continuous increase in the performance of the procedure is suggested to be a major factor4.
The distribution of reconstructions among different age groups has changed3,6. Women younger than 49 years make up the majority of patients undergoing breast reconstruction. Older women often opt to not undergo reconstructive surgery4,7. Concordant with the recent literature3, nearly half (49%) of the patients in this study were younger than 50 years. Early diagnosis and less-aggressive cancer treatments have enabled more patients to benefit from immediate reconstruction. Although APC-sparing mastectomy accounts only for 2% of ablative procedures, these techniques are remarkable in terms of the immediate breast reconstruction rate, which exceeds 88%.
Awareness of breast cancer treatment has also increased dramatically in recent years. Through television, the internet, charity events, and publications, women are improving their knowledge about treatments for this disease, which include breast reconstruction. Furthermore, the city of New York enacted a new law requiring all professionals dealing with this disease to inform their patients about breast reconstruction possibilities8.
The increasing rate of immediate breast reconstructions corresponds to the growing use of implants. Although the reconstruction rate with autologous tissue was maintained between 1998 and 2008, the use of implants increased by 208%4. The use of implants surpassed autologous reconstructions in 2002 and began to be considered the leading reconstruction procedure4. The present study shows a similar predominance of breast reconstructions with implants over autologous tissues (74% vs. 26%, respectively). In contrast, older population-based studies consistently reported a ratio of 2:1 for reconstructions with autologous tissues and implants, respectively9.
Surprisingly, the rate of autologous reconstructions has not changed. There are many possible reasons for this. First, investigations on the outcomes of breast reconstructions suggest patients undergoing breast reconstruction with autologous tissues have better long-term satisfaction, longer-lasting aesthetics, and more stable results than those receiving implants10. Second, refinements in microsurgical procedures led to the advent of perforator flaps such as deep inferior epigastric artery perforator (DIEP) flaps and superficial inferior epigastric artery perforator (SIEP) microsurgical flaps, which are currently the state-of-the-art/gold standard techniques for autologous reconstructions. Perforator flaps minimize donor-site morbidity compared to conventional TRAM flaps as a result of muscle preservation, the maintenance of abdominal strength, and fewer hernias11.
The availability of operating rooms is the limiting factor for autologous reconstructions. One autologous reconstruction takes several times longer than one reconstruction with implants. For instance, unilateral implant reconstruction can be performed in 1 hour, whereas unipedicle TRAM requires approximately 3.5 hours. Furthermore, micro-surgical reconstructions with DIEP or SIEP can require 6 hours or more. Finally, the lack of surgeons trained to perform microsurgical reconstructions may contribute to increased prevalence of reconstructions with implants compared to autologous tissues4.
There are several possible reasons why women increasingly prefer implant reconstructions.
First, in 2006, the FDA reported the safety of silicone implants in reconstructive and aesthetic surgeries12 .
Second, younger women have less adipose tissue for autologous reconstruction or prefer/request faster restoration with less morbidity4.
Third, there are cultural aspects related to breast cosmetic surgery with implants. Women currently prefer non-ptotic breasts that have a more artificial than natural appearance4.
Finally, in the past, women who received adjuvant irradiation tended to be advised to avoid implant reconstruction and opt for autologous tissue reconstruction because of an increased risk of complications. Nowadays, increased experience with implants after radiation therapy has enabled satisfactory outcomes13.
Nevertheless, these are merely hypotheses and as such require more in-depth investigation.
It should also be mentioned that recent concerns related to anaplastic giant-cell lymphoma and silicone implants may result in reconstructions with autologous tissues becoming predominant again14,15 .
Although reimbursement aspects were not assessed in this study, they may be inferred by analyzing Unified Health System (UHS) and agreement remuneration tables. In the Brazilian Hierarchical Classification of Medical Procedures 2012 table, the reimbursement for autologous reconstruction is only 7% more than that for implant reconstruction16. Reimbursements covering longer hospital stay and increased surgical complexity are not considered by covenants or the public health system, which contribute to the higher rates of implant reconstructions.
The re-intervention rate after breast-conserving surgery varies widely. Some international centers report rates ranging from 17-68%. A Dutch study compiling data from 16 hospitals including 961 patients reports a re-intervention rate of 28.9%. Independent prognostic factors considered for re-intervention include histological type, tumor sublocation and size, lymph node involvement, and multifocal disease. About half of these reinterventions are mastectomies17. In this study, when evaluating immediate reconstructions with implants separately, 36% of the cases submitted to conservative breast reconstructions were submitted to subsequent mastectomy.
At present, improved detection of smaller and/or multicenter tumors has increased the tendency to perform surgeries that allow greater skin preservation. Therefore, the development of new techniques for mastectomy has resulted in remarkable progress in the achievement of aesthetic results.
Skin-sparing mastectomies are as safe as classical mastectomies. The rate of local recurrence ranges from 3-7%. They are indicated in virtually all mastectomies as they do not compromise the skin or APC18-20.
Nowadays, the main challenge for mastologists and plastic surgeons when performing either breast reconstruction or adenomastectomy is to spare the APC to achieve the most favorable aesthetic results possible.
APC preservation is based on oncologic safety, aesthetic improvement, and sensory function preservation. Most attention is focused on the first parameter compared to the potential risk of developing cancer in the main ducts and residual breast tissues, for which the rate of local recurrence is 5.4-11%. Although 97% of women report being satisfied with APC preservation, they report satisfactory aesthetic results in almost 68% of cases. The sensitivity of the APC partially and completely returns in 33% and 16% of cases, respectively21.
In general, several studies suggest the following safety criteria for APC preservervation22-24:
A survey conducted at the Faculty of Medicine of ABC shows that in addition to these factors, the most important variable for the presence of the disease in the APC is an extensive in situ component. Patient selection should always take into account the histological type of the tumor. Intraoperative study of retroareolar tissue should always be performed. It should also be noted that the risk of developing the disease is related to the papilla and not the areola. The average risk of a false-negative result in intraoperative examination is 10%25.age <75 years, absence of cutaneous involvement, absence of APC involvement (i.e., Paget's disease), absence of a central tumor, distance between tumor and APC >3 cm, distance between tumor and skin >2 cm, tumors <3-4 cm, and negative retroareolar tissue freezing.
At present, positive signals for malignancy in frozen sub-areolar tissue sections are detected in 6-16% of cases26,27. In this study, we investigated positivity for malignancies in 6.8% of cases with APC preservation.
Studies referring to major procedures, such as the work published by Cordeiro et al.28, report extensive series of immediate reconstructions with expanders/implants in which the rate of success and patient satisfaction with the shape of the reconstructed breasts remained high despite a higher complication rate due to radiotherapy. Most patients claim they would repeat this procedure, which is faster and simpler than more complex reconstructions with autologous flaps.
In the review by Platt et al.29, the average rate of major complications in all cases was approximately 15.5%. In the present study, the major complication rate was 16.5%.
CONCLUSION
Although immediate breast reconstruction with implants is a global reality in most major reference centers, the possibility of performing immediate and/or late reconstruction with autologous tissue should always be considered, discussed, and prioritized when necessary.
Plastic surgeons have many technical options at their disposal. Nevertheless, treatments should be individualized and based on the characteristics and necessities of each patient, the surgical team's familiarity with the procedure, and availability of hospital resources and funding; the ultimate aims should be optimizing results and reducing costs and complication rates.
REFERENCES
1. Brasil. Ministério da Saúde. Estimativa 2012: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2011. 118p.
2. Oliveira RR, Morais SS, Sarian LO. Efeitos da reconstrução mamária imediata sobre a qualidade de vida de mulheres mastectomizadas. Rev Bras Ginecol Obstet. 2010;32(12):602-8.
3. Junior FCO, Mélega JM, Pinheiro AS, Pereira RF. Reconstrução mamária total: técnicas e complicações. Rev Bras Cir Plást. 2010;25(supl.1):62.
4. Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131(1):15-23.
5. Nano MT, Gill PG, Kollias J, Bochner MA, Malycha P, Winefield HR. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg. 2005;75(11):940-7.
6. Atisha D, Alderman AK, Lowery JC, Kuhn LE, Davis J, Wilkins EG. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg. 2008;247(6):1019-28.
7. Crippa CG, Hallal ALC, Dellagiustina AR, Traebert EE, Gondin G, Pereira C. Perfil clínico e epidemiológico do câncer de mama em mulheres Jovens. Arq Catarin Med. 2003;32(3):50-8.
8. Lentol J. Information and access to breast reconstructive surgery law. Committee on codes. 2010. Chapter 354; Health. A. 10094-B/S. 6993-B [Accessed 2011 Jul]. Available from:http://assembly.state.ny.us/comm/Codes/2010Annual/index.pdf.
9. Polednak AP. Type of breast reconstructive surgery among breast cancer patients: a population-based study. Plast Reconstr Surg. 2001;108(6):1600-3.
10. Yueh JH, Slavin SA, Adesiyun T, Nyame TT, Gautam S, Morris DJ, et al. Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Plast Reconstr Surg. 2010;125(6):1585-95.
11. Bottero L, Lefaucheur JP, Fadhul S, Raulo Y, Collins ED, Lantieri L. Electromyographic assessment of rectus abdominis muscle function after deep inferior epigastric perforator flap surgery. Plast Reconstr Surg. Plast Reconstr Surg. 2004;113(1):156-61.
12. U.S. Food and Drug Administration. Regulatory history of breast implants in the U.S. [Accessed 2011 Nov 1]. Available from:http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/BreastImplants/ucm064461.htm.
13. Ho A, Cordeiro P, Disa J, Mehrara B, Wright J, Van Zee KJ, et al. Long-term outcomes in breast cancer patients undergoing immediate 2-stage expander/implant reconstruction and postmastectomy radiation. Cancer. 2012;118(9):2552-9.
14. Jewell M, Spear SL, Largent J, Oefelein MG, Adams WP Jr. Anaplastic large T-cell lymphoma and breast implants: a review of the literature. Plast Reconstr Surg. 2011;128(3):651-61.
15. Smith TJ, Ramsaroop R. Breast implant related anaplastic large cell lymphoma presenting as late onset peri-implant effusion. Breast. 2012;21(1):102-4.
16. Associação Médica Brasileira. Classificação Brasileira Hierarquizada de Procedimentos Médicos [Accessed 2013 Jan 20]. Available from: http://www.amb.org.br/Site/Home/PUBLICA%C3%87%C3%95ES%20AMB/CBHPM/
17. Talsma AK, Reedijk AM, Damhuis RA, Westenend PJ, Vles WJ. Re-resection rates after breast-conserving surgery as a performance indicator: introduction of a case-mix model to allow comparison between Dutch hospitals. Eur J Surg Oncol. 2011;37(4):357-63.
18. Singletary SE, Robb GL. Oncologic safety of skin-sparing mastectomy. Ann Surg Oncol. 2003;10(2):95-7.
19. Cunnick GH, Mokbel K. Oncological considerations of skin-sparing mastectomy. Int Semin Surg Oncol. 2006;3:14.
20. Torresan RZ, dos Santos CC, Okamura H, Alvarenga M. Evaluation of residual glandular tissue after skin-sparing mastectomies. Ann Surg Oncol. 2005;12(12):1037-44.
21. Petit JY, Veronesi U, Orecchia R, Luini A, Rey P, Intra M, et al. Nipple-sparing mastectomy in association with intra operative radiotherapy (ELIOT): A new type of mastectomy for breast cancer treatment. Breast Cancer Res Treat. 2006;96(1):47-51.
22. Vlajcic Z, Zic R, Stanec S, Lambasa S, Petrovecki M, Stanec Z. Nipple-areola complex preservation: predictive factors of neoplastic nipple-areola complex invasion. Ann Plast Surg. 2005;55(3):240-4.
23. Simmons RM, Hollenbeck ST, Latrenta GS. Two-year follow-up of areola-sparing mastectomy with immediate reconstruction. Am J Surg. 2004;188(4):403-6.
24. Rusby JE, Brachtel EF, Taghian A, Michaelson JS, Koerner FC, Smith BL. George Peters Award. Microscopic anatomy within the nipple: implications for nipple-sparing mastectomy. Am J Surg. 2007;194(4):433-7.
25. Pirozzi PR. Relação entre características clínicas, morfológicas e biomoleculares do carcinoma ductal infiltrativo de mama e o estado da papila [Tese de Doutorado]. São Paulo: Faculdade de Ciências Médicas da Santa Casa de São Paulo; 2008.
26. Crowe JP Jr, Kim JA, Yetman R, Banbury J, Patrick RJ, Baynes D. Nipple-sparing mastectomy: technique and results of 54 procedures. Arch Surg. 2004;139(2):148-50.
27. Simmons RM, Brennan M, Christos P, King V, Osborne M. Analysis of nipple/areolar involvement with mastectomy: can the areola be preserved? Ann Surg Oncol. 2002;9(2):165-8.
28. Cordeiro PG, Pusic AL, Disa JJ, McCormick B, VanZee K. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg. 2004;113(3):877-81.
29. Platt J, Baxter N, Zhong T. Breast reconstruction after mastectomy for breast cancer. CMAJ. 2011;183(18):2109-16.
1. Aspiring member of the BSPS in training. Physician, general surgeon, resident at the Plastic Surgery Service of Felício Rocho Hospital, Belo Horizonte, MG, Brazil
2. Plastic surgeon, member of the BSPS, member of the clinical staff of the Plastic Surgery Service of Felício Rocho Hospital and Institute of Advanced Plastic Surgery, Belo Horizonte, MG, Brazil
3. PhD in Surgery from the Federal University of Minas Gerais, member of the BSPS, professor of Surgical and Anesthetic Techniques at the Faculty of Medicine of the University of Itaúna, member of the clinical staff of the Plastic Surgery Service of Felício Rocho Hospital and Institute of Advanced Plastic Surgery, Belo Horizonte, MG, Brazil
4. Plastic surgeon, member of the BSPS, coordinator of the Plastic Surgery Service of the Life Center Hospital, assistant at the Plastic Surgery Service of Felício Rocho Hospital, Belo Horizonte, MG, Brazil
5. Plastic surgeon, member of the BSPS, regent of the Plastic Surgery Service of Felício Rocho Hospital, founder member of the Brazilian Society of Craniomaxillofacial Surgery (BSCS), Belo Horizonte, Minas Gerais, Brazil
6. Aspiring member of the BSPS in training. Physician, general surgeon, resident at the Plastic Surgery Service of Felício Rocho Hospital, Belo Horizonte, MG, Brazil
Gustavo Augusto Matos Saliba
Rua Esmeralda, nº 559/603, Bairro Prado
Belo Horizonte, MG, Brazil
Article received:01/07/2013
Article accepted:01/09/2013
This study was performed at the Felício Rocho Hospital, Belo Horizonte, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter