

Original Article - Year 2013 - Volume 28 -
Treatment of contractures in retroglandular mammary augmentation using retropectoral implants and capsular flaps
Tratamento das contraturas nas mamoplastias de aumento retroglandulares: implante retropeitoral com retalho capsular
ABSTRACT
INTRODUÇÃO: Capsular contracture is one of the most common causes of surgical revision in the mammary augmentation procedure. This phenomenon can happen with any kind of implant, or layer of the pocket. The literature shows that there is an increased prevalence in the implant in the retro mammary position, and for this reason the majority of patients whom operate for treating contracture are in this situation. In these patients we observe a significant thinning of the gland and the subcutaneous tissue, then, we create a rectropectoralis pocket to insert the new implant making use of a capsular flap, to involve it completely. This allows larger implants house with great security, nice cosmetic results and high satisfaction.
Keywords: Implant Capsular Contracture. Mammaplasty. Breast Implants. Surgical Flaps.
RESUMO
INTRODUÇÃO: Este trabalho propõe, nos casos de contratura capsular em mamoplastias de aumento retroglandulares, a inclusão de novos implantes no plano retropeitoral, empregando retalhos de cápsula para sua fixação.
MÉTODO: Foram avaliadas, retrospectivamente, 27 pacientes portadoras de contratura capsular tratadas desta forma entre maio de 2007 e junho de 2012.
RESULTADOS: A técnica utilizada permitiu abrigar implantes maiores com bom aspecto de contorno mamário, assegurados pela cobertura muscular, estabilizada pelo retalho capsular.
CONCLUSÕES: A técnica apresentada é um método seguro, reprodutível, tecnicamente simples, de resultados satisfatórios e baixa prevalência de intercorrências.
Palavras-chave: Contratura capsular em Implantes. Mamoplastia. Implantes de Mama. Retalhos Cirúrgicos.
The presence of an implant behind the mammary gland leads to a thinning of the overlying planes, subcutaneous fat, and mammary gland. Furthermore, events such as pregnancy, weight loss, or the aging process can accentuate this phenomenon.
In agreement with this aspect and given that most patients opt for larger breast volumes when undergoing secondary augmentation mammoplasty to treat contractures, we consider it important to construct a new pocket in the retromuscular plane to provide better coverage and a more natural result.
We performed sectioning of the inferior medial portion of the origin of the pectoralis major muscle to better accommodate the implants and eliminate their tendency to rise. This maneuver, in turn, enhances communication between the previous and new surgical pockets.
We used a technique of covering the lower portion of the prosthesis with a flap made from part of the old retroglandular capsule to stabilize the pectoral muscle and prevent the implant from migrating to the original plane.
These measures ensure adequate coverage with the necessary camouflage of the margins of the new implants and a highly satisfactory aesthetic result.
Regardless of all the current developments and knowledge about breast implant procedures, a recent study series1 in which implants with current designs were used reported a risk for revision surgery of 12%. Most of these reoperations were performed purely because of aesthetic dissatisfaction related to size and shape. However, approximately 10% to 20% of these revisions are due to capsular contracture, motivated by pain or dysmorphia2-4. In our more than 20 years' experience with patients consult with us, the prevalence of contracture can reach 50%5.
METHODS
Between May 2007 and June 2012, 27 patients with signs of capsular contracture underwent implant replacement using the technique described earlier. Among them, nine had associated mastopexy.
While the patient was standing, we marked the implant placement site according to the dimensions of the implants that would be used.
The surgical approach was submammary, except in the patients whose areolas had at least 4 cm in diameter, those with previous scar on the location, or those in which one pexy was indicated in the same procedure.
We incised the breast parenchyma until we identified the capsule to be dissected from the breast in its entire anterior surface, with or without an implant inside. (figs 1 e 2)
After explantation, we performed partial capsulectomy. Only the upper half of the capsule was removed. The preserved lower half then only maintained its medial and lateral sectioned segments, allowing the anterior lamella of the capsule to be folded inferiorly to later complement the coverage of the implants. The posterior lamella attached to the pectoral muscle ensured adequate blood supply to the flap.
We dissected the retromuscular space following the previous marking and resected the origin of the pectoralis major muscle in its lower medial portion, just enough to cause a relaxation in this segment and cancel the tendency of the implants to rise due to pressure by muscle action.
This segmental section of the pectoralis major, as a rule, causes a significant cranial retraction of the muscle because of the absence of attachment to other tissue planes.
The implant was then placed in the retropectoral plane, and the capsular flap was folded inferiorly, caudally carrying the adhered belly of the pectoralis major muscle. After excision of any excess, the implant was sutured to the superficial fascia, at the level of the inframammary fold, with a 3-0 nylon suture (Figs. 1-4).
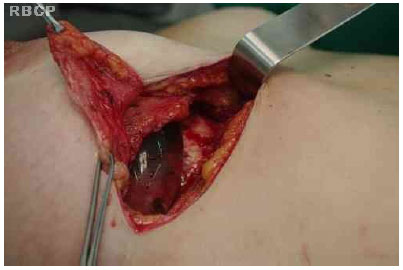
Figure 1 - Incision of the breast parenchyma to identify the capsule.
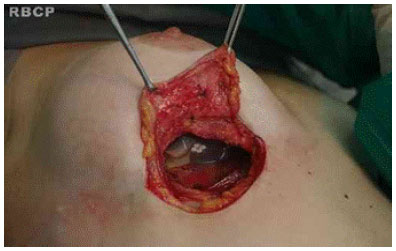
Figure 2 - Incision of the breast parenchyma to identify the capsule .

Figure 3 - Implant positioning in the retropectoral plane.
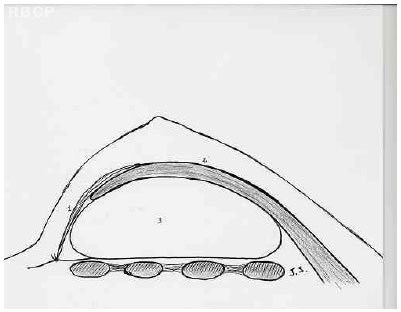
Figure 4 - Illustration showing the position of the implants after surgery .
The overlying planes were sutured with absorbable sutures, and no drains were used.
RESULTS
The procedure was simple to perform. All of the patients developed aesthetically pleasing breast shapes (Figs. 5-8).

Figure 5 - A patient with aesthetically pleasing breasts .

Figure 6 - A patient with aesthetically pleasing breasts .
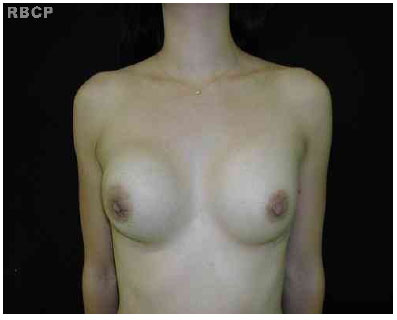
Figure 7 - A patient with aesthetically pleasing breasts.

Figure 8 - A patient with aesthetically pleasing breasts.
We observed one case of unilateral seroma that was drained on three occasions, with good evolution. Hematoma, dehiscence, or scar problems did not occur.
DISCUSSÃO
Undoubtedly, with the increase in knowledge, and improvements of surgical technique and implant quality, we have witnessed a progressive decrease in the prevalence of capsular contracture in augmentation mammoplasty. However, it is still a common complaint in our clinic, as we often attend to patients operated for 10 or more years.
Many situations have been already associated with the development of capsular contractures, such as the presence of contaminants such as glove talc, cotton compresses, and even pulp packaging of implants. Microtrauma arising from the friction of the implant texture with the capsule, bruising, and bacterial contamination originating from ruptured cysts and breast ducts were also indicated6.
In some statistical data, an occurrence of 1% to 4% can be noted. However, many of these numbers can be disputed for not taking into account the time factor.
The retroglandular plane is the choice of most surgeons during primary augmentation mammoplasty2. Studies also show that capsular contracture is more common when the implants are accommodated in this situation7,8. Some argue that continuous muscle action on the fibrous capsule would make this occurrence less frequent when the implant is retropectoral.
When referring to secondary augmentation mammoplasty, we observe a significant increase in capsular contracture as a reason for surgery. In a recent survey by Pitanguy et al.3, 9% of the revisions were due to contracture. Spears reported that 55% of patients who underwent secondary augmentation mammoplasty or augmentation mastopexy presented with capsular contracture2,3.
Augmentation mammoplasty, together with lipoplasty, is one of the most sought plastic surgeries by women worldwide, and we have seen this occur especially in the last two decades. Moreover, due to a globalization effect, we have seen a progressive increase in the volume of the implants used regularly, according to patient demand.
Most patients who face a secondary surgery opt for a further increase in breast volume, for the reasons already mentioned or because of loss by thinning induced by the implant or the natural aging process.
Replacement of the allocation plane of the implant, which is associated with its fixation in the retropectoral space, with the capsular flap combines simplicity, safety, and good aesthetic results. The capsular flap, thin but quite tough with good circulatory viability, will contain the implant in the proper position, until the formation of a new capsule and the inner healing is complete.
REFERENCES
1. Yoo G, Lee PK. Capsular flaps for the management of mal-positioned implants after augmentation mammoplasty. Aesthetic Plast Surg. 2010;34(1):111-5.
2. Spear SL, Low M, Ducic I. Revision augmentation mastopexy: indications, operations, and outcomes. Ann Plast Surg. 2003;51(6):540-6.
3. Pitanguy I, Amorim NFG, Ferreira AV, Berger R. Análise de trocas de implantes mamarios nos últimos cinco anos na Clínica Ivo Pitanguy. Rev Bras Cir Plást. 2010;25(4):668-74.
4. Pinchuk V, Tymofii O. Seroma as a late complication after breast augmentation. Aesthetic Plast Surg. 2011;35(3):303-14.
5. Ventura OD, Marino H, Marcello GA. Treatment of the fibrous capsule on mammary implants: a technical innovation for changing the implant from the subglandular to the submuscular plane. Aesthetic Plast Surg. 2008;32(2):365-7.
6. de Benito J, Sanchez K. Secondary breast augmentation: managing each case. Aesthetic Plast Surg. 2010;34(6):691-700.
7. Mahler D, Hauben DJ. Retromammary versus retropectoral breast augmentation-a comparative study. Ann Plast Surg. 1982;(5):3704.
8. Zeitoune GC. The best plane for breast implantation in patients with hipomastia: submuscular or sugglandular? Rev Bras Cir Plást. 2012;27(3):428-34.
Plastic Surgeon and full member of the Brazilian Society of Plastic Surgery
José Aurino Cavalcanti Saraiva
Al. Prof. Lucas Nogueira Garcêz, 3525 - Jd. Paulista
CEP: 12947-000 - Atibaia, SP, Brasil
E- mail: saraiva@clinicasaraiva.com.br
Article received:12/09/2013
Article accepted: 05/10/2013
Work performed at the Clinica Saraiva - Atibaia, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter