

Original Article - Year 2013 - Volume 28 - Issue 4
Evaluation of nipple-areola complex position after breast augmentation surgery
Avaliação do posicionamento do complexo aréolo-papilar na evolução pós-operatória da cirurgia de mamoplastia de aumento
ABSTRACT
INTRODUCTION: The augmentation mammoplasty commonly provokes in patients an inquiry about the possibility of breast falling. The plastic surgery usually answers yes, but don't find studies justifying this. In this research we focus to understand the position variation of papillary-areolar complex after breast implants observing principally the "ptosis tendency" and "bottoming out" phenomenon.
METHODS: Medical records selection between patients operated in Instituto Ivo Pitanguy - Infirmary 38 of Santa Casa de Misericórdia do Rio de Janeiro since 2009 January until 2010 December based on inclusion and exclusion criterions using for this research medical records revision, photographer register and literature revision.
RESULTS: Among the 20 breasts (10 patients) analyzed we observed "bottoming out" in 8 breasts (5 patients) 4 moderated and 4 mild. Occur "ptosis tendency" in 10 breasts (5 patients) 4 mild and 6 moderated. Only 1 breast didn't suffered APC variation.
CONCLUSION: The "ptosis tendency" and "bottoming out" phenomenon are a reality that has to be largely studied to better elucidation for patients.
Keywords: Mammary Glands, Human. Mammaplasty. Breast implants.
RESUMO
INTRODUÇÃO: A mastoplastia de aumento, muito comumente, gera na paciente indagações acerca da possibilidade de queda das mamas. A resposta do cirurgião plástico é geralmente afirmativa, porém, este não encontra respaldo na literatura. Neste trabalho, objetivamos justamente entender a variação de posição do Complexo aréolo-papilar pós-inclusão de implantes mamários observando, principalmente, os fenômenos de "tendência à ptose" e "bottoming out".
MÉTODOS: Seleção de prontuários dentre as pacientes operadas no Instituto Ivo Pitanguy - Enfermaria 38 da Santa Casa de Misericórdia do Rio de Janeiro de jan/2009 a dez/2010, com base em critérios de inclusão e exclusão, utilizando-se para esta pesquisa de revisão dos prontuários, registro fotográfico e revisão da literatura.
RESULTADOS: : Dentre as 20 mamas ( 10 pacientes ) analisadas observamos "bottoming out" em 8 mamas ( 5 pacientes ) das quais 4 de graus moderados e 4 leves. Houve "tendência à ptose" em 10 mamas (5 pacientes) sendo 4 leves e 6 moderadas. .
CONCLUSÃO: Os fenômenos "bottoming out" e tendência à ptose" são uma realidade que precisa ser amplamente estudada para melhor esclarecimento das pacientes.
Palavras-chave: Glândulas Mamárias Humanas. Mamoplastia. Implantes de mama.
Breast augmentation surgery with implants is one of the most commonly performed surgical procedures today in Brazil and worldwide. The significant increase in the number of procedures is likely because the breasts play an important role in female sexuality and psychosocial well-being 1.
Surgery is mainly indicated for breast asymmetry, hypomastia, congenital abnormalities of the chest wall, breast ptosis, deformity secondary to breast surgery, and the simple desire to increase breast volume 2,,3.
In daily clinical practice, patients frequently ask surgeons if their breasts may sag after breast implantation. Although surgeons usually respond that this is unlikely, there is insufficient published evidence supporting this statement.
"Tendency to ptosis" is the negative vertical change of the nipple-areola complex (NAC). Meanwhile, "bottoming out" is the increase in the distance between the NAC and the mammary crease due to the caudal migration of the implant, distorting the lower pole of the breast 4.
In addition, many patients may report discomfort, heaviness, and even pain in the breasts after surgery. The observation of rippling due to the thin tissue at the inferior pole of the breast is also not unusual in such cases 5.
Accordingly, the present study analyzed changes in the position of the NAC as well as the presence bottoming out and tendency to ptosis after breast augmentation surgery.
METHODS
The information contained in this study was obtained from medical records, interviews with patients, photographs, and literature review.
We retrospectively evaluated the medical records of all patients undergoing surgical breast implantation at the Ivo Pitanguy Institute - 38th Infirmary of the Santa Casa de Misericordia of Rio de Janeiro from January 2009 to December 2010. From a total of 368 patients, we selected those that met the following inclusion and exclusion criteria:
Inclusion and exclusion criteria
The inclusion criteria were breast augmentation with breast implants and aesthetic indications for the retro-glandular or retro-muscular plane through lower peri-areolar, trans-areolar, or mammary fold incisions; polyurethane-coated or textured breast silicone implants; and patient able to be located using data from medical records and photographs taken 1 month postoperatively.
The inclusion criteria
Were breast augmentation with breast implants for breast reconstruction or in association with mastopexy; no photographs taken 1 month postoperatively; or unable to be located.
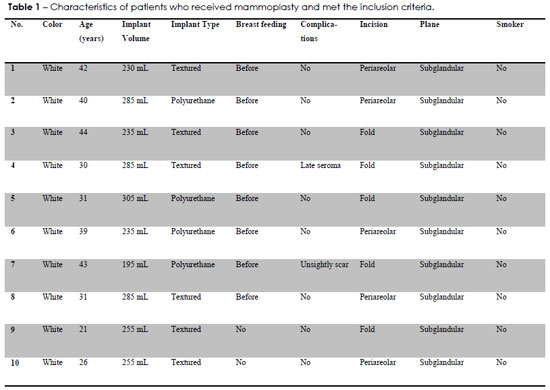
Ten patients met the inclusion criteria and were subjected to a physical examination, photography, and an interview; their characteristics are shown in Table 1.
Photographic analysis
Photographic analysis was performed by comparing the photographs of patients in the early postoperative period (within 1 month postoperatively) and late postoperative period (1-3 years); follow-up ranged from 18-33 months. An automatic 10-megapixel digital camera with a focal range of 35-105 mm equivalent and 1× optical zoom was used. A comparative photographic method was then performed by a single medical professional with surgical training by direct visualization with the naked eye. Fixed variables were defined on the chest of the patient, and ratios of measures were established for analysis (Figures 1 and 2). Measurements were made manually using a ruler and protractor. Computer graphics were also used as an auxiliary tool.
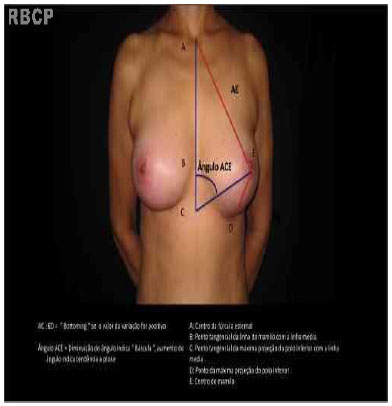
Figure 1 - Photographic analysis method, showing the fixed points used as references, front view
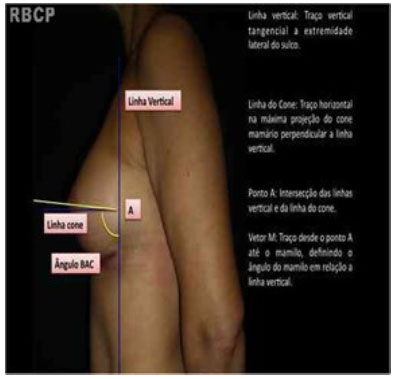
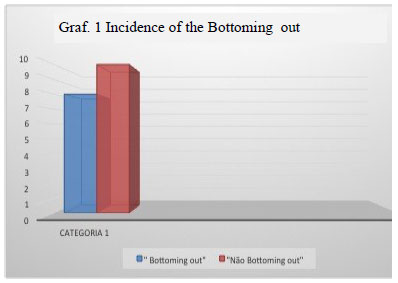
Figure 2 - Photographic analysis, profile view
Definitions of variables
Fixed points of reference on the patient's chest were assessed with the patient in an upright posture with arms back. Some of these points and measures are cited in the work of Westreich 6the others were made on the basis of observations in the present study. The measurement points were a folows:
- POINT A: Center of the sternal notch.
- POINT B: Tangential point of the line from the nipple to the midline
- POINT C: Tangential point of the maximum projection of the lower pole of the breast to the midline
- POINT D: Point of maximum projection of the lower pole of the breast 6.
- POINT E: , center of the nipple 6.
Comparative measurements (Figure 1)
The AC:ED ratio was defined as the distance between the center of the sternal notch and the tangential point of maximum projection of the lower pole of the breast to the middle line divided by the distance between the center of the nipple and the point of maximum projection of the lower pole of the breast 6.
An increase in this ratio from the early to late postoperative period indicated the presence of bottoming out.
· The ACE angle was defined as the angle whose vertex is point C formed by straight lines that intersect points A and E.
When comparing early and late postoperative photographs, an increase in this angle indicated tendency to ptosis, while a decrease indicated sliding of the NAC.
Fixed points of reference on the chest in profile view (Figure 2)
· The vertical line was defined as a straight vertical line tangential to the lateral edge of the mammary crease .
· The cone line was defined as the straight horizontal line passing through the maximum projection of the breast cone, perpendicularly intersecting the vertical line.
· Point A was defined as the intersection point of the vertical line with the cone line.
· Vector M was defined as the straight line that intersects point A and the center of the nipple.
Comparative measurements (Figure 2)
The BAC angle was defined as the angle whose vertex is point A, being formed by vector M and the vertical line below point A. When comparing early and late postoperative photographs, an increase in this angle indicated sliding, while a decrease indicated tendency to ptosis.
In this analytical method, the AC:ED ratio and ACE angle best detected bottoming out and tendency to ptosis, respectively. Therefore, through clinical perception and comparison of these parameters between the early and late postoperative periods, we classified changes <5%, 5-30%, and >30% as mild, moderate, and severe, respectively
RESULTS
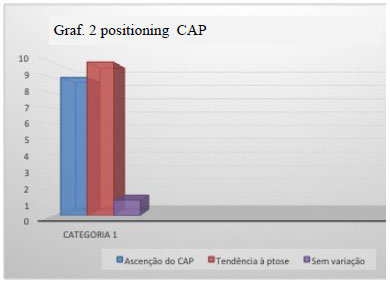
Among 20 breasts in 10 patients, bottoming out was observed in 9 breasts in 6 patients (Figure 6), including 5 moderate and 4 mild (Table 2, Figure 1). This analysis was performed by comparison of the AC:ED ratio (Figure 3).
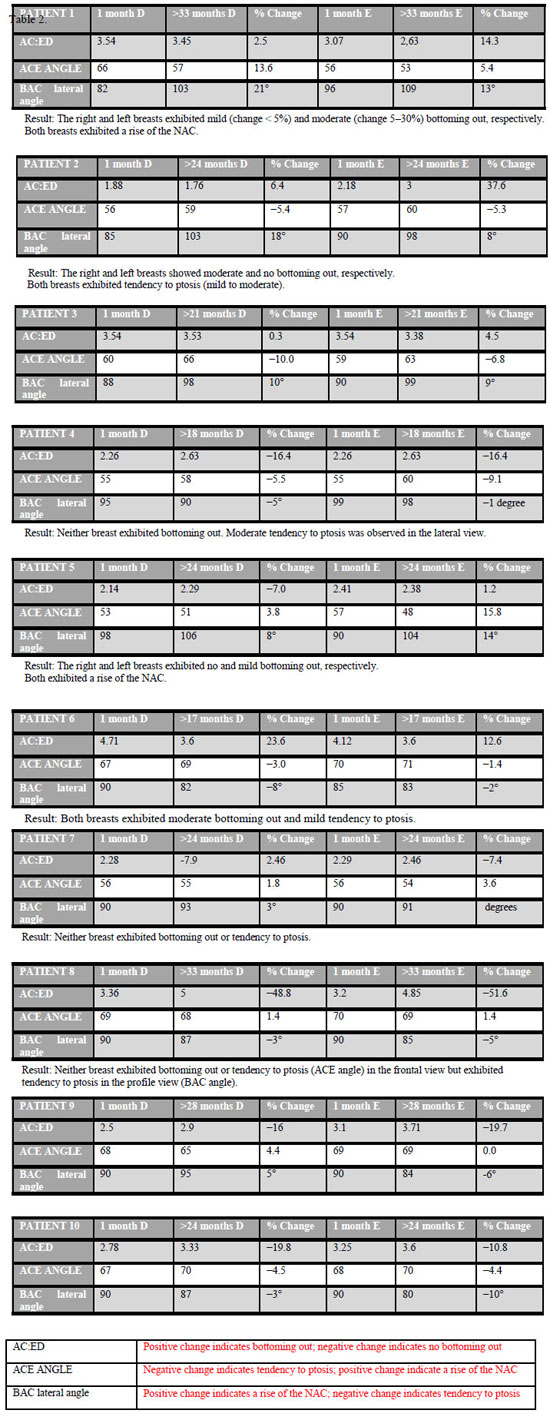
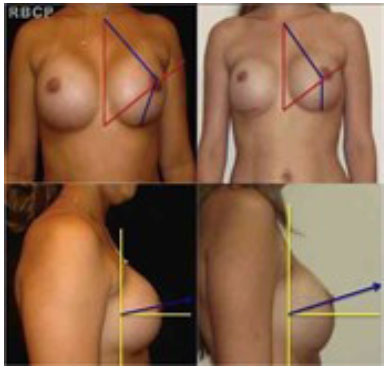
Figure 3 - PATIENT 5: photographs 1 month (left) and 24 months (right) postoperatively demonstrating the phenomenon of bottoming out on the left breast (front view) and rise of the NAC in the right breast (profile view).
Considering the NAC as a parameter, in the front view, 9 breasts in 5 patients exhibited tendency to ptosis, including 3 mild and 6 moderate. Meanwhile, 11 breasts in 6 patients exhibited a rise of the NAC; ; only 1 breast exhibited no change in NAC positioning (Tables 2 and 3, Figure 2). This analysis was performed by comparison of the ACE angle (Figure 3).
In the profile view, in 11 breasts in 6 patients, the NAC exhibited tendency to ptosis; meanwhile, in 9 breasts in 5 patients, the NAC exhibited a tendency to rise (Figure 5, Table 2). This analysis was performed by comparison of the BAC lateral angle (Figure 4).
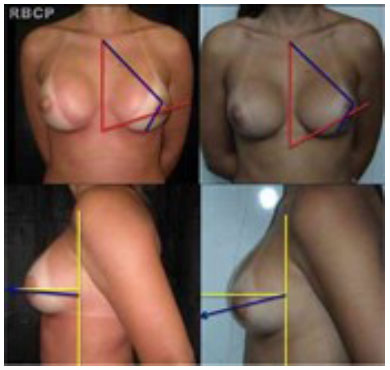
Figure 4 - PATIENT 10: photograph showing the fall of the NAC in the left breast (profile view) 24 month postoperatively (bottom left).
There were no associations of the general characteristics of the patients, including age, implant type or volume, smoking, or prior breastfeeding (Table 1), with the phenomena mentioned above.
Furthermore, 7 breasts in 4 patients exhibited neither bottoming out nor tendency to ptosis. Meanwhile, 12 breasts in 7 patients exhibited either bottoming out or tendency to ptosis.
DISCUSSION
When breast augmentation surgeries were first performed, there was little control over the results. The surgeon could only guarantee breast augmentation itself. Assumptions and generalizations were employed to circumvent ignorance of tissue dynamics and their relation to the implants. Surgeons now have some tools to quantify simple parameters previously treated subjectively 7. In 2001, Dr. Tebbetts published "TEPID," which is a selection algorithm for breast implants based on tissue characteristics and the dynamic relationship of the implant with breast tissue 8. TEPID aims to reduce complications such as skin stretching, ptosis, parenchymal atrophy, implant visibility and palpability, rippling phenomenon, and bottoming out among others.
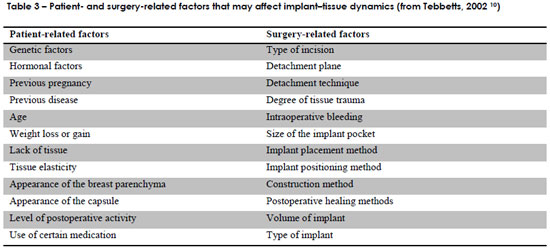
Numerous factors related to breast tissue and the surgeon (Table 3) can affect the outcome of augmentation mammoplasty 8-11. Therefore, it is difficult to explain why these phenomena occur over time after implant placement, including the changes demonstrated herein. However, objectively and quantitatively, statistical evidence demonstrating the incidence of such phenomena as well as related implant and patient characteristics may contribute to better preoperative guidance.
Breast ptosis is an aesthetic complication characterized by sagging of the breast due to the relaxation of their support. The following 6 classifications of breast ptosis were found through an electronic search in LILACS and MEDLINE from 1951 to 2008: Binet (1951), Robutti & Lupo (1970), Regnault (1976), Bozola (1990 ) Chekkour et al. (1991), and Oliveira Jr et al. 12. However, none of them mention breast implants The existence of multiple grades shows that none of these classifications is fully satisfactory; all apply to restricted situations according to case history and the experience or convenience of the classifier. However, it is notable that the most valid parameter is ptosis of the nipple 12. Consequently, at no point did we aim to classify the operated breasts according to the degree of ptosis. Instead, we used the nipple as a parameter to try to clarify if the breast was sagging or not. Therefore, we cautiously used the term "tendency to ptosis" and graded it as mild, moderate, or severe. We also proposed an objective classification for the phenomenon of bottoming out.
Both the tendency to ptosis and phenomenon of bottoming out were clearly evident in this study. One explanation is that the framework of the breast is designed to support up to a certain weight. Therefore, negative effects may occur when genetic or hormonal influence, weight gain, pregnancy, or breast implants exceeds this capacity 8,13,14. Nevertheless, no effect by itself significantly influenced these phenomena.
The prediction of the postoperative positions of the nipple and NAC remains difficult. Several variables are involved, including the degree and type of previous ptosis, quality of the skin envelope, gland/fat ratio of the breast tissue, and breast behavior in the postoperative course 15. However, the present study demonstrates the postoperative assessment of such changes is easy.
It is very clear how dynamic changes occur in breasts. The behavior of the breasts can vary considerably within a patient, as demonstrated in patient 10; in this patient, one of the breasts exhibited bottoming out with a rise in the NAC, while the other did not bottom out but with tendency to ptosis (Table 2).
Bottoming out is one way by which breasts sag and occurs as a result of the migration of the implant to the inferior pole of the breast .
The nipple-papillary complex is arguably the best parameter for assessing breast ptosis; its fall is associated with the perception of sagging breasts. In this study, 12 breasts in 7 patients exhibited some degree of breast sagging; this is a very significant number that justifies the concerns and questions of patients before surgery.
CONCLUSION
The tendency to ptosis after the placement of breast implants and the phenomenon of bottoming out must be reported and responded to in preoperative consultation.In short, there is a high probability of sagging breasts after the placement of implants.
In the present study, the degree of ptosis was mild to moderate.
Several factors may contribute to ptosis but none of them alone are strongly associated with ptosis except for placement of the breast implant. The rise or fall of the NAC was also very common in the present study.
Even following the principle of matching the center of the implant with the nipple during surgery, the postoperative positioning of the NAC was uninfluenced by the direction of the implant or rest of the breast framework.
Thus, the present results were unexpected, making these complications even more challenging to the surgeon. Further studies involving histological analysis of breast tissue are required to further improve predictability and surgical approaches, and thus improve results.
REFERENCES
1. Verbicário JPM, Ferreira AV, Holanda TA, Amorim NFC, Pitanguy I. Incisão transareolopapilar para mamoplastia de aumento: experiência dos últimos 10 anos do Instituto Ivo Pitanguy. Rev Bras Cir Plást. 2011;26(4):670-4.
2. Pitanguy I. Análise das trocas de implantes mamários nos últimos cinco anos na Clínica Ivo Pitanguy. Rev Bras Cir Plást. 2010;25(4):668-74.
3. Pitanguy I. Aesthetic plastic surgery of head and body. Berlin Heidelberg: Springer-Verlag; 1981. p.412.
4. Hammond DC, Hidalgo D, Slavin S, Spear S, Tebbetts J. Revising the unsatisfactory breast augmentation. Plast Reconstr Surg. 1999;104(1):277-83.
5. Tebbetts JB. The greatest myths in breast augmentation. Plast Reconstr Surg. 2001;107(7):1895-903.
6. Westreich M. Anthropomorphic breast measurement: protocol and results in 50 women with aesthetically perfect breasts and clinical application. Plast Reconstr Surg. 1997;100(2):468-79.
7. Dowden RV. Brody's article on "the perfect breast". Plast Reconstr Surg. 2005;115(4):1202-3.
8. Tebbetts JB. "Out points" criteria for breast implant removal without replacement and criteria to minimize reoperations following breast augmentation. Plast Reconstr Surg. 2004;114(5):1258-62.
9. Tebbetts JB, Teitelbaum S. High- and extra-high-projection breast implants: potential consequences for patients. Plast Reconstr Surg. 2010;126(6):2150-9.
10. Tebbetts JB. A system for breast implant selection based on patient tissue characteristics and implant-soft tissue dynamics. Plast Reconstr Surg. 2002;109(4):1396-409.
11. Tebbetts JB. Achieving a zero percent reoperation rate at 3 years in a 50-consecutive-case augmentation mammaplasty premarket approval study. Plast Reconstr Surg. 2006;118(6):1453-7.
12. Souza SC. Graduações de ptose mamária. Arq Catarin Med. 2008;37(3):66-71.
13. Pitanguy I, Carreirão S, Mazzarone F, Fróes LB, Cló TT. Mastopexia associada à inclusão de prótese. Rev Bras Cir Plást. 1991;81(2):101-11.
14. Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2006;118(7 Suppl):35S-45S.
15. Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117(3):757-67.
1. Specialist Member of the Brazilian Society of Plastic Surgery (SBCP) - Assistant Instructor, Post-Graduate Medical Course, Pontifical Catholic University of Rio de Janeiro and Carlos Chagas Postgraduate Medical Institute, Rio de Janeiro, RJ, Brazil. Scientific advisor to the Ivo Pitanguy Institute, Rio de Janeiro, RJ, Brazil
2. General Surgeon - Postgraduate in Plastic Surgery, Ivo Pitanguy Institute, Rio de Janeiro, RJ, Brazil
3. General Surgeon - Postgraduate in Plastic Surgery, Ivo Pitanguy Institute, Rio de Janeiro, RJ, Brazil
4. Full Member of the SBCP, Assistant Professor, Postgraduate Medical Course, Pontifical Catholic University of Rio de Janeiro and Carlos Chagas Postgraduate Medical Institute, Rio de Janeiro, RJ, Brazil
5. Patron of the SBCP, member of the National Academy of Medicine and the Brazilian Academy of Arts. Professor of Medical Postgraduate course in Plastic Surgery, Pontifical Catholic University of Rio de Janeiro and of the Carlos Chagas Postgraduate Medical Institute, Rio de Janeiro, RJ, Brazil
João Paulo Verbicario
Rua Visconde de Pirajá, 351 salas 1104/1105 - Ipanema
CEP: 22410-003 - Rio de Janeiro, RJ, Brasil
Article received: 30/09/2013
Article accepted: 30/10/2013
Work performed at the Ivo Pitanguy Institute - 38th Infirmary of the Santa Casa de Misericordia of Rio de Janeiro


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter