

Original Article - Year 2013 - Volume 28 -
Scrotal reconstruction using a superomedial thigh flap after Fournier's syndrome
Reconstrução escrotal com retalho súpero-medial da coxa após síndrome de fournier
ABSTRACT
INTRODUCTION: Necrotizing fasciitis is a severe infection that consumes the perineal-scrotal skin quickly. Overcome the infection, it is necessary to cover the compromised structures. We present a series of patients suffering from necrotizing fasciitis who underwent scrotal reconstruction using the superior medial thigh flap.
METHODS: Seven male patients underwent unilateral or bilateral scrotal reconstruction with superior medial thigh flap.
RESULTS: The patients showed satisfactory results as regards coverage testicular and appearance of the donor area.
CONCLUSION: The superior medial thigh flap is presented as an excellent choice for scrotal reconstruction by testicular produce good coverage, is easy to perform and improve local aesthetics.
Keywords: Fournier Disease. Scrotum/Surgery. Surgical flaps.
RESUMO
INTRODUÇÃO: Fasceíte necrotizante é uma grave infecção que consome a pele períneo-escrotal rapidamente. Superada a infecção, faz-se necessária a cobertura das estruturas comprometidas. Apresentamos uma série de pacientes acometidos por fasceíte necrotizante que foram submetidos à reconstrução escrotal com a utilização do retalho súpero-medial da coxa.
MÉTODO: Sete pacientes do sexo masculino foram submetidos à reconstrução escrotal, uni ou bilateralmente, com o retalho súpero-medial da coxa.
RESULTADOS: Os pacientes apresentaram resultados satisfatórios quanto à cobertura testicular e ao aspecto da área doadora.
CONCLUSÃO: O retalho súpero-medial da coxa se apresentou como excelente opção para reconstrução escrotal por produzir boa cobertura testicular, ser de fácil execução e melhorar a estética local.
Palavras-chave: Doença de Fournier. Escroto/Cirurgia. Retalhos cirúrgicos.
Fournier's syndrome is known as a necrotizing fasciitis of the genitalia, perineum, and perianal region. It is a rare, aggressive, and mutilating infectious disease with associated high morbidity and mortality1.
Rapid progression to necrosis occurs in the structures involved in the infectious process, which extends to the fascial plane, resulting in a significant quantity of devitalized tissue.
For local control of the aggressive infection, appropriate clinical support is necessary, including antibiotic therapy of a wide spectrum and hydroelectrolytic control, in addition to successive surgical debridements until reaching the margin of healthy tissue2, culminating with major tissue loss1 and exposure of the regional muscles in the penis and testicles. The deviation of the intestinal transit through a colostomy may be necessary in cases where there is perianal impairment3. Likewise, performing cystostomy is also possible to prevent urinary contamination4.
To surpass the critical stage of infection, covering the resulting wound5 is necessary for functional and aesthetic recovery of the exposed structures, with emphasis on testicular coverage, particularly in those individuals with reproduction capability.
Reconstruction of large perineal-scrotal areas affected by the disease is a challenge for plastic surgeons6. The superomedial thigh flap is the most advantageous among the various options available to adequately cover the testicles and surrounding areas owing to its technical simplicity, presence of excess skin in the donor area, and vascular reliability. It is a fasciocutaneous flap obliquely conceived and based on the long abductor muscle of the thigh3, which is unilaterally or bilaterally transposed for construction of the new scrotal sac with efficient testicular coverage.
In this study, we present the cases of patients with necrotizing fasciitis that resulted in scrotal damage, which was successfully reconstructed using a superomedial thigh flap with satisfactory results.
METHODS
Seven male patients who had necrotizing fasciitis with exposure of the testes were surgically treated and monitored between August 2008 and June 2012 at the Hospital São Francisco de Assis,
Crato, Ceará, Brazil. Patients' age ranged from 42 to 76 years, with a mean of 53.2 years. One patient had diabetes and hypertension, another had Alzheimer's disease, and another had paraplegia. Two patients required diversion of the intestinal transit, and another three underwent cystostomy. Of the seven patients who underwent the surgical procedure, six required bilateral flaps and one required only a unilateral right flap. All patients were hospitalized in the same hospital, from the acute phase of infection to the time of scrotal reconstruction, with a mean hospital stay of 32.6 days.
The general surgery team performed debridement until the infection was controlled, and a specialized nurse administered the curatives until the appearance of good granulation tissue.
Surgical technique
The patients were placed in the lithotomy position. Spinal anesthesia was induced in sensitive patients, and sedation, in paraplegic patients. Delimitation of the flap was based on the size of the defect to be covered, the base being at the root of the thigh and its end being in an oblique direction, assuming an approximately triangular shape (Figure 1).

Figure 1 - Exposure of the testes and perineum after necrotizing fasciitis. Delimitation of the surgical flaps .
The edges of the granular tissue were revived through the removal of fibrotic tissue. The flap was incised and detached in the distal to proximal direction, including the muscle fascia (Figure 2). Transposition and fixation were performed according to the marking of the healthy margin to cover the defect. Primary closure of the donor area was performed. No. 2 Penrose drains were used and removed after 24 or 48 h.
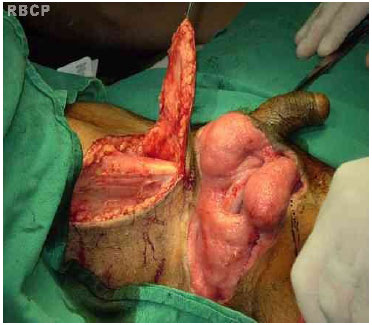
Figure 2 - Rise of the fasciocutaneous flap to the right
RESULTS
All the patients had good testicular coverage and were satisfied with the results. In the paraplegic patient, scar expansion was observed on one side of the thigh. In the patient with bilateral reconstruction, mild necrosis of the tip of the flap was observed but was conservatively resolved. Another patient had prolonged edema in the flaps, which regressed around the third month after surgery. A patient with retraction of the spermatic cord (Figure 3) complained of testicular pain, which improved with medication. (Figure 4-6)

Figure 3 - Large retraction of the spermatic cord with testicular dislocation. Delimitation of the fasciocutaneous flap unilaterally.

Figure 4 - Appearance immediately after right unilateral scrotal reconstruction

Figure 5 - Appearance 18 months after unilateral scrotal reconstruction

Figure 6 - Appearance before scrotal reconstruction.

Figure 7 - Appearance immediately after bilateral scrotal reconstruction

Figure 8 - Appearance 3 months after bilateral scrotal reconstruction.
Ambulatory monitoring of the patients was performed for 6-18 months.
DISCUSSION
Fournier's syndrome is an acute necrotizing fasciitis that rapid progresses and is potentially fatal, and mainly affects the genital, perineal, and perianal regions1,5. The syndrome is characterized by rapid and fulminating evolution to sepsis, with high morbidity and mortality2. It is a polymicrobial infection with an identifiable cause in 95% of cases, originating in the genital or perineal region. Endarteritis obliterans occurs histologically, followed by ischemia and thrombosis of the subcutaneous vessels, resulting in necroses of the skin and adjacent subcutaneous cell tissue.
Predisposing factors include diabetes mellitus, local trauma, urine leakage, perirectal or perineal surgical intervention, extent of periurethral infection, anorectal abscess, genitourinary tract infection, alcoholism1,7,8, immunosuppression, human immunodeficiency virus carriers, and kidney or liver disease, among which diabetes mellitus is the most common7. It is more prevalent in men than in women (10:1). The incidence rate is approximately 1 case in 7500 individuals. Up to 45% of the patients have diabetes mellitus, and 25% have alcohol addiction9. The disease rarely affects children1. It has a predilection for elderly, diabetic5, alcoholic, malnourished, immune depressed, obese, cirrhotic9, longtime hospitalized10, and socioeconomically disadvantaged individuals.
Owing to the severity and rapidity of the advancement of infection, extensive and repeated surgical debridement is necessary for local control of the infectious process. This results in large wounds and exposure of the testes, which become unprotected and suspended only by spermatic cords, subsequently requiring adequate tissue coverage through a restorative procedure11. The testes do not develop necrosis because their vascularization and lymphatic drainage are different from those of the penis and scrotum4,12.
In the treatment of wounds resulting from necrotizing fasciitis of the scrotum, the following three aspects should be considered: wound healing, maintenance of organ function, and aesthetic recovery13. In case of delayed testicular coverage process, contraction following granulation formation incarcerates the testicles, which may lead to twists or compressions that alter spermatogenesis, which may have previously been impaired by the disease itself13 (Figure 3). Multiple surgical debridements for the removal of necrotic debris is required, performed 3.5 times per patient on average.
The superomedial thigh flap was first described by Hirshowitz13,14 in the reconstruction of the scrotum and vulva. It has rich vascularity, mainly from the branches of the femoral artery (internal and circumflex pudenda), making it a safe option even for individuals with diabetes and vasculopathies. It provides good replacement of extensive scrotal skin loss, allows easy technical execution, and produces excellent aesthetic results, both in the donor and receptor areas5,8.
Ferreira et al.14 indicated that in addition to these advantages, the superomedial thigh flap is made in a single procedure, leaves no sequelae in the donor area, and restores the psychological balance of the patient regarding coverage of the exposed genital structures.
The flap has similar tissue as the scrotum, and even contains hair. It allows for preservation of local sensitivity through the inclusion of ilioinguinal nerves and the genital branch of the genitofemoral nerve3,8,13, simple implementation in a single surgical operation12, and primary synthesis of the donor area. However, the availability of the donor thigh area is a limiting factor, which may be limited in young patients owing to low laxity of the region.
Mordjikian1 reports that fasciocutaneous flaps provide lesser protection, volume, and vascularity than myocutaneous flaps, although they have the advantage of not causing functional impairment of the donor area.
In a retrospective study by Ferreira et al.14, medical records of 43 patients with necrotizing fasciitis between 1985 and 2003 were analyzed. The researchers used superomedial thigh flaps in 26 of the patients, of whom 17 underwent bilateral and 9 underwent unilateral reconstruction. They observed partial dehiscence in five patients.
El-Mageed12 prefers the anterior flap of the medial surface of the thigh over the superomedial flap, stating that the former has the following advantages: easier dissection and access, less acute arc of rotation with lower risk for pedicle torsion, smaller dog-ears at the top due to the transposition and scar in the donor area, and distant from the area of friction between the thighs.
Meanwhile, Ayad6 used the medial thigh flap to reconstruct the scrotal sac after Fournier's gangrene in a series of seven patients. This flap is similar to that used in our series, except for the height of the upward dissection and the absence of a wound that requires skin grafting. Scrotal sac reconstruction after Fournier's gangrene remains a major challenge for plastic surgeons. The reconstruction is important for organ function, aesthetics, and psychological reasons6.
Whaib8 suggested that minor complications such as dehiscence, localized seroma, extended flap edema, distal necrosis, paresthesias, and scar expansion in the donor area might occur. However, they do not compromise the good aesthetic results achieved through reconstruction.
In our series, we found a small area of distal necrosis in a flap that healed by secondary intention in a case of bilateral reconstruction. In addition, persistent edema of the flaps, which subsided after 3 months, and scar expansion in the donor area were observed in a patient who underwent bilateral reconstruction and in a paraplegic patient, respectively. The patient with retraction of the spermatic cord (Figure 3) persistently complained of pain in the testicular topography for approximately 1 year after reconstruction.
Rest and the use of scrotal suspensory for at least 3 postoperative weeks were prescribed to all our patients. These precautionary measures were intended to reduce edema and tension on the wound from the weight of the structures and thus promote good healing13. However, the patient with persistent edema did not follow these precautions, which prolonged his recovery time.
Ideal scrotal reconstruction should present the following characteristics: completion of surgery in a single procedure, use of a flap with maintained sensitivity, minimal morbidity at the donor area, simplicity of execution, and reliability of the flap used6,12.
CONCLUSION
The use of a superomedial thigh flap is an excellent option for scrotal reconstruction, as it requires procedures with easy technical execution, promotes good testicular coverage, and does not produce sequelae in the donor area, in addition to providing functionally and aesthetically lasting results.
REFERENCES
1. Mordjikian E, Oliveira MA, Merolo Jr J. Métodos de reconstrução cirúrgica utilizados no tratamento das deformidades teciduais decorrentes da gangrena de Fournier: análise de 10 casos. An Bras Dermatol. 2001;76(6):701-9.
2. Mehl AA, Nogueira Filho DC, Mantovani LM, Grippa MM, Berger R, Krauss D, et al. Manejo da gangrena de Fournier: experiência de um hospital universitário de Curitiba. Rev Col Bras Cir 2010;37(6):435-41.
3. Horta R, Cerqueira M, Marques M, Ferreira P, Reis J, Amarante J. Fournier's gangrene: from urological emergency to plastic surgery. Actas Urol Esp. 2009;33(8):925-9.
4. Silva Filho AF, Pereira NA, Siqueira IMG, Saraiva PS, Magalhães GM, Alves JCRR. Fasceite necrosante da genitália masculina: síndrome de Fournier. An Bras Dermatol. 1998;73(2):97-103.
5. Mauro V. Retalho fasciocutâneo de região interna de coxa para reconstrução escrotal na síndrome de Fournier. Rev Bras Cir Plást. 2011;26(4):707-9.
6. Ayad WM, Al-Shahat OA, Zaied E, Albanooby T, Taman E. The versatility of the medial thigh flap for reconstruction of post-Fournier's gangrene complex perineoscrotal defects. J Plast Reconstr Surg. 2011;35(1):129-32.
7. Bhatnagar AM, Mohite PN, Suthar M. Fournier's gangrene: a review of 110 cases for aetiology, predisposing conditions, microorganisms, and modalities for coverage of necrosed scrotum with bare testes. N Z Med J. 2008;121(1275):46-56.
8. Whaib ARA. Evaluation of superomedial fasciocutaneous thigh flap in replacement of scrotal and penile skin. Iraq Postgrade Med J. 2011;10(3):374-80.
9. Naji SH. Reconstruction of scrotum in Fournier's gangrene. Kufa Med J. 2011;14(2):219-24.
10. Judice PLP, Christofoli MOJM, Oliveira PCR, Teles IG, Najjar YSJ. Gangrena de Fournier: relato de três casos, achados tomográficos e revisão de literatura. Rev Imagem (Online). 2010;32(1/2):21-3.
11. Park KR, Kim TG, Lee J, Ha JH, Kim YH. Single-stage reconstruction of extensive defects after Fournier's gangrene with an exposed iliac crest and testes. Arch Plast Surg. 2013;40(1):74-6.
12. El-Mageed MA. Evaluation of the anteromedial thigh fasciocutaneous flap for scrotal reconstruction. J Plast Reconstr Surg. 2007;31(2):149-55.
13. Franco D, Rodrigues C, Tavares JM, Imoto F, Franco T. Reconstrução do escroto após fascite necrosante. Rev Bras Cir Plást. 2010;25(2):349-54.
14. Ferreira PC, Reis JC, Amarante JM, Silva AC, Pinho CJ, Oliveira IC, et al. Fournier's gangrene: a review of 43 reconstructive cases. Plast Reconstr Surg. 2007;119(1):175-84.
1. Specialist member and Assistant Professor II
2. Undergraduate student of Medicine, Faculty of Medicine of Juazeiro do Norte, Ceará, Brazil
Paulo José Alves
Rua Pedro Cardoso sobreira 10 apto 201 Lagoa Seca
Juazeiro do Norte ,Ceara, Brasil
Article received : 05/09/2013
Article accepted : 05/10/2013
work performed at the Hospital São Francisco de Assis, Crato, Ceará, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter