

Original Article - Year 2013 - Volume 28 -
Assessment of the degree of correction of prominent ears using a standardized treatment algorithm
Medida do grau de correção das orelhas proeminentes utilizando algoritmo de tratamento padronizado
ABSTRACT
BACKGROUND: The goal of aesthetic otoplasty is the correction of ear deformities by creating harmonious and symmetrical external ears, without visible scars. Otoplasty techniques based on the excision of postauricular skin are associated with high recurrence rates. Modern otoplasty is based on cartilage-cutting and cartilage-sparing techniques, alone or in combination, which lead to lower recurrence rates.
OBJECTIVE: We evaluated the efficacy of otoplasty combined with other techniques in the correction of ear deformities, based on a modified version of the "algorithm for otoplasty at the Craniofacial Center at Texas Children's Hospital".
METHODS: Forty patients, who underwent otoplasty for prominent ears in our institution between March and September of 2009, were prospectively assessed. The mastoid-helix distance was measured preoperatively (baseline) and at 1, 3, and 6 months postoperatively.
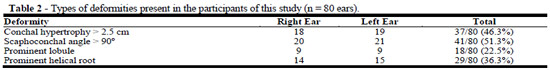
RESULTS: The most common deformities were scaphoconchal angle greater than 90º (51.3%, 41/80 ears) and conchal hypertrophy > 2.5 cm (46.3%, 37/80 ears). Recurrence occurred in 2 (5%) patients and partial stenosis of the ear canal in 1 (2.5%). Significant reductions in the mastoid-helix distance were observed at the three time points compared with baseline (P<0.001); a significant reduction was present in the immediate postoperative period (P<0.001), followed by a small increase 3 months postoperatively (P<0.005), which appeared to stabilize between 3-6 months postoperatively (P=0.520).
CONCLUSION: Otoplasty performed according to the modified algorithm resulted in a significant reduction of the mastoid-helix distance, which slightly increased in the early postoperative period, and re-mained unchanged 6 months postoperatively.
Keywords: Otologic surgical procedures. Ear, External. Deformities.
RESUMO
INTRODUÇÃO: O objetivo da otoplastia estética é a correção de deformidades da orelha, criando orelhas externas harmoniosas e simétricas. As técnicas de otoplastia, baseadas na excisão da pele pós-auricular, estão associados com a recorrência elevada. A otoplastia moderna é baseada nas técnicas de ressecção e/ou modelagem da cartilagem, que levam a menores taxas de recorrência.
OBJETIVO Foi avaliada a eficácia da otoplastia com técnica combinada na correção de deformidades da orelha, baseado numa versão modificada do "algoritmo para otoplastia", no Centro Craniofacial do Hospital Infantil do Texas".
MÉTODO: Quarenta pacientes submetidos à otoplastia por orelhas proeminentes, entre março e setembro de 2009, foram avaliados prospectivamente. A distância mastoide-hélice foi medida no pré-operatório e após 1, 3 e 6 meses após a cirurgia.
RESULTADOS: As deformidades mais comuns foram ângulo escafo-conchal maior que 90º (51,3%, 41/80 orelhas) e hipertrofia de concha> 2,5 cm (46,3%, 37/80 orelhas). Reduções significativas na distância mastoide-hélice foram observadas nos três períodos em comparação com os valores basais (P<0,001). Houve uma redução desta medida no período pós-operatório imediato (P<0,001), seguido por um pequeno aumento após três meses da cirurgia (P<0,005) e subsequente tendência de estabilização entre 3-6 meses após a cirurgia (P=0,520).
CONCLUSÃO: Otoplastia, realizada de acordo com o algoritmo citado, resultou em redução significativa da distância mastoide-hélice, com ligeira perda desta redução no início do período pós-operatório, e com tendência a manter-se inalterado após 6 meses de pós-operatório.
Palavras-chave: Orelha externa. Otoplastia. Deformidades.
Ear deformities are relatively common, occurring with an incidence of 5% in Caucasians. The deformity is diagnosed at birth in 60% of cases and becomes obvious during early childhood1. The most common defects in patients with prominent ears are an absent or reduced antihelical fold, conchal hypertrophy or deep conchal bowl, inadequate definition of the helical rim, and abnormalities of the lobule. Patients with prominent ears may have one or more of these defects2,3. The goal of otoplasty is the correction of ear deformities by creating harmonious and symmetrical external ears, without visible signs of the surgical procedure4. Techniques to correct prominent ears based on the excision of postauricular skin are associated with high recurrence rates. Modern otoplasty is based on cartilage-cutting2 and cartilage-sparing techniques, alone or in combination, with recurrence rates ranging from 2.1% to 6.6%1,5.
The purpose of this study was to evaluate the efficacy of otoplasty combined with other techniques in the correction of ear deformities, based on a modified version of the "algorithm for otoplasty at the Craniofacial Center at Texas Children's Hospital".
METHODS
The study was approved by the Research Ethics Committee of the Hospital do Servidor Público Municipal de São Paulo (HSPM), Brazil, and performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its succeeding revisions. Written informed consent was obtained from all patients or their representatives prior to their inclusion in the study, and anonymity was assured.
A prospective assessment was performed in 40 consecutive patients who underwent otoplasty for prominent ears at the Plastic Surgery Unit of the HSPM between March and September 2009. The exclusion criteria were patient younger than 6 years-old, previous otoplasty surgeries, another malformations of the external ear. The participants were mostly female (60%) and the mean age was 20 years (range 8-55 years). Data were collected through a standardized questionnaire and mastoid-helix distances were measured preoperatively (baseline) and at 1, 3, and 6 months after surgery (Fig. 4).
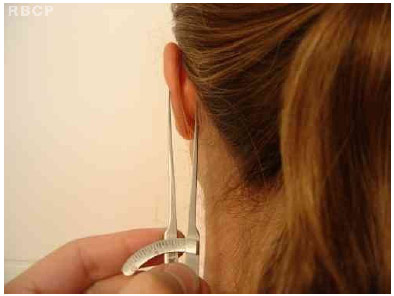
(Fig 4 ) Picture of the measure of the mastoid-helix distance with precision compass/caliper
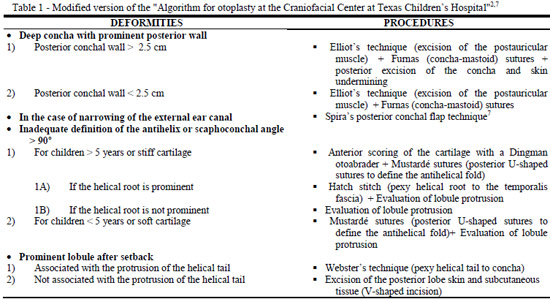
The otoplasty techniques used in each case were determined based on a modified version of the "algorithm for otoplasty at the Craniofacial Center at Texas Children's Hospital" (Table 1)6, which combines cartilage cutting, rasping and scoring, and suture techniques (Fig. 5-8)

(Fig 5.) Preoperative marking - marking of the points for conchal-helix sutures and for conchal resection

(Fig. 6) Preoperative marking - marking of the retroauricular incision

(Fig.7) Posterior resection of the conchal excess followed by simple suture

(Fig.8) Rasp is passed through the antitragohelicine fissure to the anteroauricular surface and perichondrium and cartilage are scored on the anterior surface
Statistical analysis was carried out using the Statistical Packa ge for the Social Sciences (SPSS) version 15.0 for Windows (SPSS Inc., Chicago, IL) and the Statistical Analysis System (SAS, SAS Institute Inc., Cary, NC) for repeated-measures analysis of variance. All statistical tests were performed at a significance level of 0.05 (P<0.05).
RESULTS
Among the participants, 75% reported that they were ridiculed in the study/work environment because of their deformity and 40% reported low self-esteem. First-degree relatives of participants also had the same deformity in 42.5% of cases.
Common auricular deformities included scaphoconchal angle greater than 90º (51.3%, 41/80 ears) and conchal hypertrophy > 2.5 cm (46.3%, 37/80 ears) (Table 2). Note that some patients had more than one type of deformity.
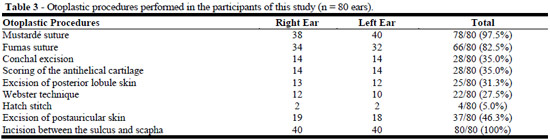
The most frequently used procedures were the placement of Mustardé sutures to create the antihelical fold and Furnas (concha-mastoid) sutures (Table 3).
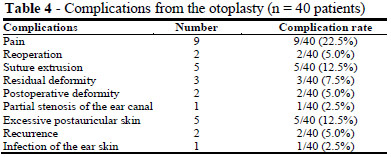
The most common postoperative complications were pain (22.5%), suture extrusion (12.5%), and excessive postauricular skin (12.5%). However, the most problematic complications were recurrence (5%), partial stenosis of the ear canal (2.5%), and residual deformities detected in the immediate, early and late postoperative periods (Table 4).
Significant reductions in the mastoid-helix distance were observed at the three time points compared with baseline (P < 0.001).
Otoplasty procedures performed based on the modified algorithm for management of prominent ears resulted in a significant reduction of the mastoid-helix distance within the first postoperative month (P<0.001) and a small increase in this distance 3 months postoperatively (P<0.005), with no significante differences between 3 and 6 months after the procedure (P>0.520) (Tables 5 and 6, Figs. 1-3).
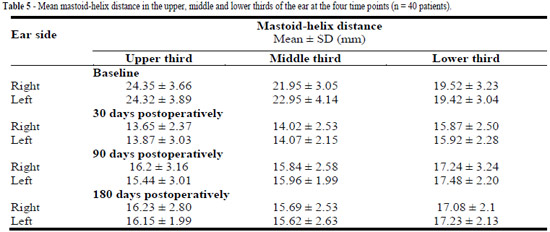
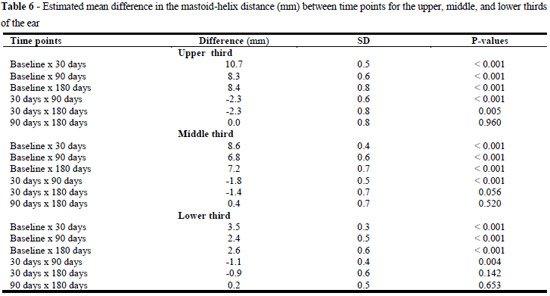
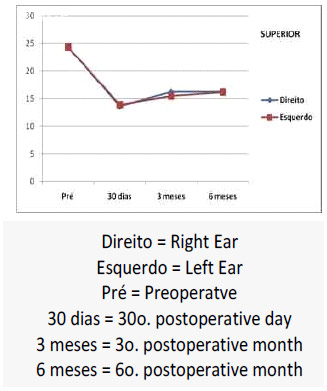
Fig 1. Variation of the mastoidhelix distance in the upper third of the right and left external ears in otoplasty patients.
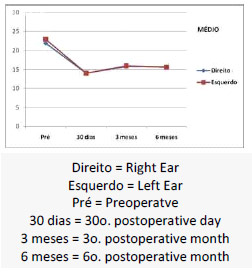
Fig 2. Variation of the mastoidhelix distance in the medial third of the right and left external ears in otoplasty patients.
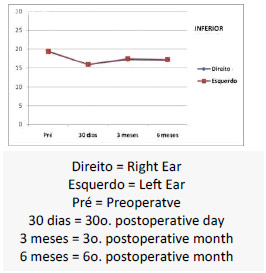
Fig 3. Variation of the mastoidhelix distance in the lower third of the right and left external ears in otoplasty patients.
DISCUSSION
The prominet ear is a deformity with a relatively high prevalence in the general population, occurring in up to 5% of Caucasians1. This indicates that otoplasty is an important part of routine practice in plastic surgery. Thus, the identification of clinical parameters that may contribute to the assemment of anatomic features pre- and post-operatively and evaluation of experiemental and well-established techniques and protocols is of fundamental importance.
Previous studies have used the mastoid-helix distance as an assessment parameter, with normal ranges of 10 to 12 mm at the superior helix, 16 to 18 mm at the level of the external ear canal, and 20 to 22 mm at the tail of the helix2,6. The measurement of the scaphoconchal angle may lead to inaccurate results because the precision measuring instrument have to be in contact with the cartilage in a relatively small space.
A grading system for prominent ears has been suggested based on the assessment of the mastoid-helix distance, conchal hypertrophy, and scaphoconchal angle. According to this system, external ear deformities are graded as: 1) mild, for mastoid-helix distances between 15 and 20 mm; 2) moderate, for mastoid-helix distances between 20 and 24 mm; 3) severe, for mastoid-helix distances between 24 and 28 mm; and 4) totally upfront ear, for mastoid-helix distances > 28 mm. The antihelical fold is determined to be present or absent by visual inspection8.
Other authors have considered aesthetic aspects, such as the need to correct any protrusion in the upper third of the ear; the helix should be seen beyond the antihelix and have a smooth and regular line; the postauricular sulcus should not be reduced or distorted, ears should be symmentricaly positioned and with similar shapes4, and the auriculomastoid angle should be between 20º and 30º9.
Conventional treatments involve the weakening of the antihelical cartilage (through rasping, scoring or incisions), suture techniques, reduction of the conchal hypertrophy, and excision of the postauricular skin3. In the present study, combined techniques were used in the treatment of each case, according to a modified version of the "algorithm for otoplasty at the Craniofacial Center at Texas Children's Hospital" (Table 1)3,5.
The mastoid-helix distance was used as an assessment parameter to evaluate the otoplasty results in this study. This distance is a continuous reproducible measure that can be objectively assessed using a precision compass and a millimeter ruler. Other authors10 reported a significant increase in the mastoid-helix distance (range, 1-7.7 mm; < 3 mm in 71.7% of cases) in the immediate postoperative period, but no significant increase in this distance was observed 12 months after surgery. Overcorrection was considered unnecessary because it would have little effect on otoplasty results9.
There were significant reductions in the mastoid-helix distance at the three time points compared with baseline (P < 0.001). Otoplasty resulted in a marked reduction of the mastoid-helix distance in the immediated postoperative period, followed by a small increase in this distance 3 months after surgery, and a tendancy to stabilize between 3-6 months postoperatively (Figs. 1-3). For example, the mastoid-helix distance in the upper third of the ear had a mean reduction of 10.7 mm one month after the procedure (P<0.001), followed by an mean increase of 2.3 mm at 3 months postoperatively, with no significant differences between 3 and 6 months postoperatively. The reduction in the mastoid-helix distance observed in the immediate postoperative period and maintained over the period of this study can be attributed to the use of the algorithm for otoplasty, which indicates the proper techniques to correct the prominent ear and residual deformities.
There were 2 cases of recurrence and 1 case of partial stenosis of the ear canal during the immediate postoperative period. Two surgical corrections yielded acceptable results. Spira's posterior conchal flap technique was performed in the case of partial stenosis of the ear canal. Mustardé sutures were used in case of recurrence due to the lack of definition of the antihelical fold.
CONCLUSION
Otoplasty performed according to a modified version of the "algorithm for otoplasty at the Craniofacial Center at Texas Children's Hospital" resulted in a significant marked reduction in the mastoid-helix distance in the immediate postoperative period, followed by a slight increase in this distance 3 months after surgery, which remained stable thereafter. The sequencing of procedures, as indicated by the algorithm for management of the prominent ear, takes into account the type of deformity, ensuring that the most effective technique to reduce the mastoid-helix distance is used.
REFERENCES
1. Aki F, Sakae E, Cruz DP, Kamakura L, Ferreira MC. Complicações em otoplastia: revisão de 508 casos. Rev Soc Bras Cir Plást. 2006;21(3):140-4.
2. Stal S, Klebuc M, Spira M. An algorithm for otoplasty. Oper Tec Plast Reconstr Surg. 1997;4(3):88-103.
3. Sperli AE. Oto-pericondrioplastia: atualização de técnica. Rev Soc Bras Cir Plást. 1998;13(3):7-18.
4. Schlegel-Wagner C, Pabst G, Müller W, Linder T. Otoplasty using a modified anterior scoring technique: standardized measurements of long-term results. Arch Facial Plast Surg. 2010;12(3):143-8.
5. Lee KH, Pereira Filho OJ, Grangeiro LS, Neves CRZD, Bins-Ely J. Endotoplastia por incisão superior. Rev Bras Cir Plást. 2012;27(supl):42.
6. Kelley P, Hollier L, Stal S. Otoplasty: evaluation, technique, and review. J Craniofac Surg. 2003;14(5):643-53.
7. Janis JE, Rohrich RJ, Gutowski KA. Otoplasty. Plast Reconstr Surg. 2005;115(4):60e-72e.
8. Bhatti AZ, Adeniran A. Grading and scoring of prominent ears. Plast Reconstr Surg. 2006;118(2):582-3.
9. Naumann A. Otoplasty - techniques, characteristics and risks. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2007;6:Doc04.
10. Braun T, Hainzinger T, Stelter K, Krause E, Berghaus A, Hempel JM. Health-related quality of life, patient benefit, and clinical outcome after otoplasty using suture tecniques in 62 children and adults. Plast Reconstr Surg. 2010;126(6):2115-24.
1. Doctorate. Assistant Physician, Department of Plastic and Burns Hospital for State Civil Servants Surgery - Francisco Morato de Oliveira / SP - HSPE FMO. Former Resident of the Hospital do Servidor Publico Municipal de São Paulo Plastic Surgery
2. Doctor. Plastic surgeon. Former Resident of the Hospital do Servidor Publico Municipal de São Paulo Plastic Surgery
3. Doctor. Resident of the Hospital do Servidor Publico Municipal de São Paulo Plastic Surgery
4. Assistant Professor of the Public Service of the Municipal Hospital of São Paulo Plastic Surgery
5. Doctorate. Associate Professor, Discipline of C. Plastic Advisor Professor of Post-Graduate Assistant Professor of Plastic Surgery, Hospital for City Public Service of São Paulo Plastic Surgery
6. Master's degree. Assistant Professor of Hospital Municipal Public Servant of São Paulo Plastic Surgery
7. Doctorate. Head of the Hospital Municipal Public Servant of St. Paul Plastic Surgery service
Leonardo Gabeira Secco
Rua Dr. Veiga Filho, 350 cjs. 106 a 109 ; Higienopolis
CEP 01229-001 São Paulo, SP, Brazil
Tel.: +55 (11) 3822-0328; Fax: +55 (11) 3661-9502
E-mail: leonardosecco@uol.com.br
Article received:18/10/2012
Article accepted: 25/11/2012
Work performed at the no Serviço de Cirurgia Plástica do Hospital do Servidor Público Municipal de São Paulo - Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter