

Original Article - Year 2013 - Volume 28 -
Evaluation of depression levels in individuals with chronic wounds
Avaliação do nível de depressão em indivíduos com feridas crônicas
ABSTRACT
BACKGROUND: The Hyperbaric Oxygen Therapy-HOT, is a non-invasive therapeutic method in which patient breaths 100% oxygen (pure oxygen) through masks, while remain in a pressurized chamber to a pressure higher than atmospheric. Its act as an accelerator of recovery process, by increasing the oxygen saturation in the body that allows to speed up cicatrization and engagement to infection. The aim of this study was to determine the epidemiological profile of hyperbaric oxygen therapy patient of Mato Grosso do Sul state.
OBJECTIVE: To demonstrate the Epidemiological Profile of patients treated with the aid of hyperbaric oxygen in the State of Mato Grosso do Sul May 2007 to October 2012.
METHODS: We conducted a restrospective study of HOT patients admitted to Santa Casa de Campo Grande Hospital from May 2007 to October 2012.
RESULTS: Among 600 patients who underwent HOT, there was a predominance for males (71% - 425 patients); Plastic surgery is the medical speciality which most request HOT associated with conventional treatment for their patients (71% of the total patients), and most of these are due to burn injury (82%). Most of the patients were aged between 31 and 60 years old. (the range with highest prevalence were 31 to 60 years). The mean number of hyperbaric sessions among the burn patients was between 6 and 10 sessions (66.19% of burn patients).
CONCLUSIONS: The majority of our service to patients requiring hyperbaric oxygen therapy was male because of moderate to severe burns, and the Plastic Surgery specialty that most used this tool as adjuvant treatment.
Keywords: Hyperbaric Oxigenation. Therapeutics. Wound Healing.
RESUMO
INTRODUÇÃO: Avaliar a intensidade e osníveis de sintomas de depressão nos pacientes com feridas crônicas.
MÉTODO: Estudo exploratório e analítico. Participaram do estudo 25 pacientes com úlceras venosas, 30 com úlceras por pressão e 18 diabéticos com pé ulcerado. Para mensurar a intensidade de sintomas e o nível de depressão foi utilizado o Inventário de Avaliação de Depressão de Beck.
RESULTADOS: Dentre os pacientes com úlcera venosa, sete (28%) apresentaram depressão leve a moderada e três (12%) depressão moderada a grave. Dezesseis (53,3%) pacientes com úlceras por pressão manifestaram depressão leve a moderada, e cinco (16,7%), depressão de moderada a grave. Dez (55,6%) pacientes diabéticos com pé ulcerado apresentaram depressão leve a moderada e, quatro (22,20%)sem depressão ou depressão mínima.
CONCLUSÃO: Os autores concluíram que os pacientes do estudo apresentaram entre depressão leve a moderada e grave.
Palavras-chave: Diabetes Mellitus. Qualidade de vida. Depressão. Pé diabético. Úlcera Por Pressão. Úlcera Venosa.
The current state of demographic transition in Brazil and the increases in life expectancy and the number of individuals with chronic conditions has created the need for a broader search for interventions that are focused not only on prevention but also on the treatment of continuous problems that affect human beings, including skin lesions1.
Chronic wounds are characterized by a diversion in the physiological sequence of wound healing phases and are frequently associated with systemic involvement or disease. In these wounds, the body response is more proliferative (fibroblastic) than exudative and the chronic inflammation process negatively affects cellular repair2.
The recurrence rate of chronic wounds is high, ranging from 80 to 90%. Their persistence is debilitating, as they can cause functional disability and dependence. Taking economic and social costs into account, chronic wounds can be considered an important health problem3.
In the United States, more than three billion dollars are spent annually on treatment of chronic wounds; however, this does not include the cost associated with the treatment of emotional issues resulting from the presence of the lesion2.
The negative impact on the quality of life of patients with ulcers is due to several interrelated factors, including odor, presence of exudate, pain, reduced mobility, lack of sleep, and increased frequency of dressing changes4,5. For patients with hard-to-heal chronic wounds, these complications can lead to loss of independence, mood swings, a negative impact on self-esteem and self-image, and isolation from social and family life, potentially leading to anxiety and depression6.
Depression is a disease that concerns specialists all over the world. Current statistics indicate that more than 400 million people suffer from depression worldwide. The World Health Organization estimates that, in the next 20 years, depression will move from fourth to second place in the list of expensive and fatal diseases, ranking behind heart disease alone7.
Despite these statistics, depression is not a disease of the 21st century. The term "depression" was initially used in 1860 to describe sadness and became commonly used in the mid-19th century6-8. Once depression is treated, there is an improvement in the patient's quality of life, an increase in self-esteem, and a positive impact on social and family life. However, the scientific literature lacks studies into depression involving patients with chronic wounds, even though studies on the wider subject have been conducted in several countries.
Given the relevance of these issues, this study could contribute to current knowledge of depression in patients with chronic wounds and assist healthcare professionals, particularly those who deal with this condition. Thus, the objective of this study was to evaluate the symptom severity and levels of depression in patients with chronic wounds.
METHODS
This was an exploratory, descriptive, and analytical study.
The sample comprised 73 patients with chronic wounds, recruited from the general population, including 25 patients with venous ulcers, 30 with pressure ulcers, and 18 diabetic patients with foot ulcers. They were all seen at the outpatient wound clinic of a hospital located in the interior of São Paulo state.
There were 97 patients registered at the outpatient clinic, including 30 with venous ulcers, 42 with pressure ulcers, and 25 diabetic patients with foot ulcers.
The inclusion criteria used were as follows: 18 years or older and suffering from venous, pressure, or diabetic foot ulcers. Patients who could not answer the questionnaire during the investigator's evaluation due to physical or mental conditions were excluded from the study.
The data were collected between December 2008 and January 2010. Ethical approval was obtained from the research ethics committee of the Federal University of São Paulo (Protocolo-1611/08). Data collection was performed by the researchers themselves once patients had signed informed consent forms.
The first instrument used was of a sociodemographic nature, containing information regarding gender, age, race, and marital status.
The Beck Depression Inventory was the second instrument used. This inventory, which was developed in the sixties and translated into Portuguese and validated in Brazil9, includes 21 categories of symptoms and behaviors typical of depression, including vegetative, social, and cognitive symptoms in addition to measures of humor and irritability9,10.
The following score ranges were used to represent depression severity in this study: no or minimal depression (0-10), mild to moderate depression (11-18), moderate to severe depression (19-29), and severe depression (30-63) 9,10.
A non-parametric Kruskal-Wallis test and Chi-square independence test were used for statistical analysis. The significance level was set at 5% (p < 0.05) in all statistical analyses.
RESULTS
Results presented in Table 1 show that 11 (44.0%) patients with venous ulcers were aged between 60 and 75 years, 11 (36.7%) patients with pressure ulcers, and 7 (38.9%) with diabetic foot ulcers were aged between 50 and 59 years. With respect to gender, there was predominance of women, 15 (60.0%) with venous ulcers, 18 (60.0%) with pressure ulcers, and 10 (55.6%) with diabetic with foot ulcers. Among patients with venous ulcers, 21 (87.5%) were white, as were 23 (76.7%) with pressure ulcers, and 16 (88.8%) with diabetic foot ulcers. There were no significant differences between groups with respect to age, race, gender, and marital status.
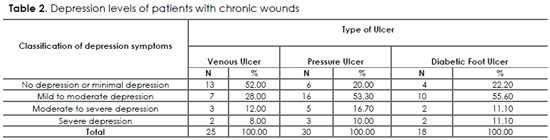
Results presented in Table 2 show that 13 (52%) patients with venous ulcers exhibited no or minimal depression; 7 (28%) exhibited mild to moderate depression, and 3 (12%) exhibited moderate to severe depression. Sixteen (53.3%) patients with pressure ulcers exhibited mild to moderate depression and five (16.7%) exhibited moderate to severe depression. Ten (55.6%) patients with diabetic foot ulcers exhibited mild to moderate depression and four (22.20%) exhibited no or minimal depression.
According to results shown in Table 3, 25 (100%) patients with venous ulcers reported the following symptoms: lack of satisfaction, pessimism, sense of failure, irritability, indecision, and sleep disorder, while 24 (96%) presented with body image distortion, self-deprecation, and social withdrawal. Thirty (100%) patients with pressure ulcers experienced body image distortion, pessimism, and sense of failure; while 29 (96.66%) reported self-deprecation, social withdrawal, irritability, indecision, sleep disorder, feelings of guilt, and suicidal thoughts. Among the patients with diabetic foot ulcers, 18 (100%) reported body image distortion, self-deprecation, lack of satisfaction, pessimism, work inhibition, irritability, decreased libido, and feelings of guilt, while 17 (94.44%) experienced social withdrawal, sense of failure, indecision, somatic concern, sleep disorder, and suicidal thoughts.
DISCUSSION
The epidemiological profile has changed due to the aging of the population, resulting in the prevalence of nontransmissible chronic diseases, which can potentially limit and compromise quality of life in older adults11.
According to a census conducted in 2000, older adults accounted for 8.6% of the Brazilian population, representing a 1.02% increase relative to the previous census, conducted in 1999. The study refers to individuals aged 50 years and older. The authors stated that patients in this age group who have chronic diseases show higher evidence of depression12.
In this study, most of the participants were women, aged 60 years and older, and divorced.
In older adults, foot ulcers are associated with physiological alterations that usually affect their ability to perform daily activities. The intensity and frequency of this effect vary and depend on socioeconomic, historical, and cultural conditions pertaining to the affected individual. It is often hard, or even impossible, for these individuals to participate in social, leisure, or family activities due to work absenteeism and an inability to perform daily tasks13, 14.
Several studies15-17 have indicated that these types of ulcer affect work productivity, which leads to disability retirement, and restrict day-today and recreational activities. For many patients with such wounds, the ulcers involve pain, impaired mobility, worsened quality of life, anxiety, and depression.
Depression is a mental disorder that interferes with the individual's physical and psychological functions at both personal and family levels. Women are twice as likely to suffer from depression than men18,19.
During the 90s, a global comparison of several diseases placed depression as the fourth most common specific cause of disability. It has been estimated that by the year 2020, depression will be the second and first leading cause of disability in developed and developing countries, respectively20.
Patients with chronic diseases, particularly those with chronic wounds, experience changes in their lifestyles and often suffer important losses at a social, economic, or personal level. The healing process is very slow or limited, resulting in residual disabilities or frequent recurrence of disease. Thus, patients with chronic diseases face constant anxiety, as they are always concerned about the possibility of negative outcomes related to their diseases21, 22.
Once the individual acquires/develops an ulcer, he or she experiences social withdrawal, as the presence of pain, odor, and exudate associated with the wound may induce anxiety and depression.
Salomé et al.14 and Serafim & Cosa21 concluded that ulcers in lower limbs limit performance of daily activities, interfere with social and family life, cause pain, and consequently lead to mental suffering and anxiety. Pain is an unpleasant emotional and sensorial experience. Both chronic pain and depression considerably affect quality of life, in addition to considerably increasing the cost of health care22.
In an integrative review, the authors concluded that the pain from venous ulcers affects the patient's daily life, representing one of the main causes of decreased quality of life, particularly as it relates to loss of sense of humor, sleep disorders, social and family withdrawal, and impaired physical mobility23. Results of this study showed that the majority of the patients presented with moderate to severe depression.
Costa et al22 analyzed the association between depressive symptoms and anxiety, in relation to chronic pain, and investigated the impact of these symptoms on health and quality of life on participants. They concluded that 70% of the participants displayed signs of anxiety and 60% exhibited depressive symptoms.
A review of the literature indicated that approximately 20-30% of diabetics are depressed. Depression can be a risk factor during the development of diabetes, leading to worsened symptoms and affecting patient's self-care. If depression is not properly treated in these patients, it can advance with high recurrence rates24,25.
Using the Beck Depression Inventory in a study performed with 50 patients, the authors concluded that 41 patients experienced some degree of depression, while 32 (64%) exhibited moderate depression, showing symptoms of self-deprecation, sadness, body image distortion, and decreased libido26.
Other authors have concluded that these wounds cause physical and psychological alterations that lead to anatomical deformities, which often result in feelings of fear, anxiety, anguish, aggressive behavior, decreased quality of life, low self-esteem, and body image distortion and potentially result in depression27-30.
This research reinforces the need for redirecting attention to the health of patients with chronic wounds, in order to identify changes in self-esteem, self-image, anxiety, and depression as part of routine activities provided by health care services, including hospitals, outpatient clinics, and family health programs. Patients who live with such wounds in their daily lives should have their care needs addressed and their caretakers should be aware of these patients' disabilities.
As researchers, we believe that it is important to develop future studies to compare the results of the Beck Depression Inventory with the following variables: sociodemographic factors, comorbidities and past history of psychiatric disease of the individual and his or her family. It is also necessary to evaluate correlations between the results from the Beck Depression Inventory and those from the subjective well-being assessment. We consider this a limitation of our study.
CONCLUSIONS
Based on the results obtained with use of the Beck Depression Inventory, it can be concluded that patients with ulcers (venous, pressure, and diabetic foot ulcers) exhibited mild-to-moderate to moderate-to-severe symptoms of depression. As the findings relate to symptom severity, the most important symptoms were as follows: lack of satisfaction, pessimism, sense of failure, self-deprecation, social withdrawal, and suicidal thoughts.
REFERENCES
1- Caliri MHL, Martins GP. Análise da produção científica da enfermagem brasileira na área de feridas crônicas e meios utilizados para sua disseminação. Rev Estima. 2008;6(1):14-21.
2 - Dantas SRPE. Aspectos históricos do tratamento de feridas. In:Jorge AS, Dantas SRPE. Abordagem multiprofissional do tratamento de feridas. São Paulo: Atheneu; 2003. p.3-6.
3 - Tuyama LY, Alves FE, Fragoso MPV, Watanabe HAW. Feridas crônicas de membros inferiores: proposta de sistematização de assistência de enfermagem a nível ambulatorial. Nursing Rev. Técnico-CientíficaEnferm. 2004;75(7):46-50.
4 - Chase SK, Whittemore R, Crosby N, Freney D, Howes P, Phillips TJ. Living with chronic venous leg ulcers: a descriptive study of knowledge and functional health status. J Community Health Nurs. 2000;17(1):1-13.
5 - Cavalini F, Moriya TM, Pelei NTR. Síndrome deFournier: a percepção do seu portador. Rev Esc Enferm USP. 2002;36(2):108-14.
6 - Yamada BFA, Santos VLCG.Quality of life of individuals with chronic venous ulcers. Wounds. 2005;17(7):178-89.
7 - Solomon A. O demônio do meio-dia: uma anatomia da depressão. Rio de Janeiro: Objetiva; 2000.
8 - Peluso ETP, Blay SL. Percepção da depressão pela população da cidade de São Paulo. Rev Saúde Pública. 2008;42(1):41
9 - Gorenstein C, Andrade LHSG. Inventário de depressão de Beck: propriedades psicométricas da versão em português. Rev PsiqClin. 1998;25(5):245-50.
10 - Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry.1961;4:561-71.
11- Neves VT, Feitosa MAG. Envelhecimento do processamento temporal auditivo. PsicTeor Pesq. 2002;18(3):275-82.
12 - Santos AB, Bandeira MA, Coiado CRP. Avaliação do grau de depressão em pacientes com insuficiência renal crônica submetidos à hemodiálise.Nursing(São Paulo).2008;11(124):411-8.
13 - Trentini M, Silva DGV, Leimann AH. Mudanças no estilo de vida enfrentadas por pacientes em condições crônicas de saúde. Rev Gaúcha Enferm. 1990;11(1):18-28.
14 - Salomé GM, Blanes L, Ferreira LM. Capacidade funcional dos pacientes com diabetes mellitus e pé ulcerado. Rev Acta Paul Enferm. 2009;22(4):412-6.
15 - França LHG, Tavares V. Insuficiência venosa crônica: uma atualização. J Vasc Bras. 2003;2(4):318-28.
16 - Salomé GM, Blanes L, Ferreira LM. Avaliação de sintomas depressivos em pessoascom úlcera venosa.RevBrasCirPlást.2012;27(1):124-9.
17 - Salomé GM, Ferreira LM.Qualidade de vida em pacientes com úlcera venosa em terapia compressiva por bota de Unna.RevBrasCirPlást. 2012;27(3):466-71.
18 - Botega NJ, Bio MC, Zomignani MA, Garcia CJr, Pereira WAB. Transtornos do humor em enfermaria de clínica médica e validação de escala de medida (HAD) de ansiedade e depressão. Rev Saúde Publica. 1995;29(5):355-63.
19 - Lima AFBS, Fleck, MPA. Qualidade de vida e depressão: uma revisão da literatura. RevPsiquiatr Rio Gd Sul. 2009;31(3 Suppl).
20 - Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349(9063):1436-42.
21 - Serafim TS, Cosa ALS. Sintomas somáticos de depressão em pacientes portadores de retocolite ulcerativa idiopática. Rev Acta Paul Enferm. 2009;22(3):295-300.
22 - Costa EC, Nakatani AYK, Bacchion MM. Capacidade de idosos da comunidade para desenvolver atividades de vida diária e atividades instrumentais de vida diária. Acta Paul Enferm. 2006;19(1):43-8.
23 - Jones JE, Robinson J, Barr W, Carlisle C. Impact of exudate and odour from chronic venous leg ulceration. NursStand. 2008;22(45):53-4.
24 - Castro MMC, Quarantini LC, Daltro C, Pires-Calda M, Koenen KC, Kraychete DC,et al.Comorbidade de sintomas ansiosos e depressivos em pacientes com dor crônica e o impacto sobre a qualidade de vida.RevPsiquiatrClín.2011;38(4):126-9.
25 - Costa IKF, Melo GSM, Farias TYA, Tourinho FSV, Enders BC, Torres GV, et al. Influence of pain on daily life of people with venous ulcers: evidence:based practice. Rev Enferm UFPE on line. 2011;5(spe):514-21.
26. Fráguas R, Soares SMSR, Bronstein MD. Depressão e diabetes mellitus. RevPsiquiatr Clín. 2009;36(3):93-9.
27. Monami M, Longo R, Desideri CM, Masotti G, Marchionni N, Mannucci E. The diabetic person beyond a foot ulcer: healing, recurrence, and depressive symptoms. J AmPodiatrMed Assoc. 2008;98(2):130-6.
28. Salomé GM, Blanes L, Ferreira LM. Avaliação de sintomas depressivos em pessoas com diabetes mellitus e pé ulcerado. RevColBras Cir. 2011;38(5):327-33.
29. Salomé GM, Maria de Souza Pellegrino D, Blanes L, Ferreira LM. Self-esteem in patients with diabetes mellitus and foot ulcers. J TissueVia
1. Medical Student at the Universidade do Vale do Sapucaí (University of Vale do Sapucai - UNIVÁS). Pouso Alegre, MG, Brazil
2. Nurse
3. Master of Science
4. Associate Professor of the Professional Master's Degree in Applied Health Sciences at UNIVAS, Pouso Alegre, MG, Brazil
Geraldo Magela Salomé
Av. Francisco de Paula Quintaninha Ribeiro, 280/134
CEP: 04330-020. São Paulo, SP, Brazil
Article received: 05/09/2013
Article accepted: 05/10/2013
This study was performed at the: Santa Casa de Campo Grande. Campo Grande, MS, Brasil.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter