

Reviw Article - Year 2013 - Volume 28 -
Positioning the scar of the region brachioplasty upper arm in ex-obese patients
Posicionamento da cicatriz da braquioplastia na região posterior do braço em pacientes ex-obesos
ABSTRACT
INTRODUCTION: Brachioplasty is the surgical treatment of severe ptosis of the arm tissues, which is located on the inside and bottom, extending from the armpit to the elbow when the arm is in abduction, having or not fat deposits.
OBJECTIVE: The objective of this work is to show the positioning of the brachioplasty scar in the lower region of the arm, viewed only afterwards, in ex-obese patients, not being visible by patient or whoever is before him or her, during the arm abduction.
METHODS: 18 patients were selected and undergone bilateral brachioplasty with lower region positioning of the scar.
RESULTS: the satisfaction degree of the patients with the scar positioning in this region was relevant, allowing it to be imperceptible during arm abduction by the patient or whoever is before him or her.
CONCLUSIONS: The surgical technique applied to brachioplasty is safe and reproducible, constituting a good alternative to disguise the scar in this region, important factor in ex-obese patients' surgery.
Keywords: Reconstructive Surgical Procedures. Arm/Surgery. Weight Loss. Surgery, Plastic/Methods.
RESUMO
INTRODUÇÃO: A braquioplastia consiste no tratamento cirúrgico da acentuada ptose dos tecidos do braço, que se localiza na região interna e inferior, estendendo-se da axila ao cotovelo, quando o braço está em abdução, contendo ou não depósito de gordura.
OBJETIVO O objetivo deste trabalho é mostrar o posicionamento da cicatriz da braquioplastia na região inferior do braço, visto somente posteriormente, em pacientes ex-obesos, não sendo visível pelo paciente ou por quem estiver à sua frente durante a abdução do braço.
MÉTODOS: Foram selecionados 18 pacientes, realizando-se a braquioplastia bilateral, com posicionamento da cicatriz na região inferior.
RESULTADOS: O grau de satisfação dos pacientes com o posicionamento da cicatriz nesta região foi elevado, permitindo que a mesma fique imperceptível durante a abdução do braço, não sendo vista pelo paciente ou por outra pessoa que se encontre em sua frente.
CONCLUSÕES: A técnica cirúrgica apresentada para braquioplastia é segura e reprodutível, constituindo uma boa opção para disfarçar a cicatriz nesta região, fator importante na cirurgia dos pacientes ex-obesos.
Palavras-chave: Procedimentos Cirúrgicos Reconstrutivos. Braço/Cirurgia. Perda de peso. Cirurgia Plástica/Métodos.
Patients who have experienced significant weight loss often exhibit marked ptosis of the lower arms during abduction, from the axilla to the elbow. This results in an exaggerated convex contour with or without a fatty deposit. Brachioplasty is the surgical treatment of this deformity; in most cases, this is performed by dermo-fat resection and flap creation by sliding. The procedure may or may not be associated with lipoaspiration.
The techniques and strategies described for brachioplasty are rarely used by plastic surgeons and are seldom accepted by patients because of the high visibility of scars and frequent complications. Several authors have greatly contributed to the development of these techniques and strategies. The first of such authors was Posse1, who described elliptical excision in the medial portion of the arm. Moreover, Correa-Iturraspe & Fernandez2 and Pitanguy3 reported an S-shaped incision. Meanwhile, over 35 years previously, Baroudi4 recommended positioning the scar in the bicep crease. Franco and Rebello5 reported an L-shaped incision. Moreover, Illouz6 reported the lipoaspiration technique. Juri et al.7 reported the quadrangular flap with a final T-shaped scar. Lockwood8 described the facial suspension system. Finally, Márquez & Abramo9 reported the joint treatment of arm, axilla, and elbow.
Accordingly, this study reports a technique for better positioning of the brachioplasty scar by placing it on the lower arm (when viewed posteriorly), thereby preventing the unsuitable position along the bicep crease, which is visible when the arm is abducted. Other authors have published reports on this topic, including Aly & Cram10 in 2006, Maciel11,12 in 2008, and Kathib13 in 2009.
Patient selection and assessment
For better surgical indications, Baroudi & Ferreira14, Aly & Cram10, and Maciel11,12 divided patients into 3 groups. Group II that includes patients with sagging and little or no lipodystrophy is the most common. Such cases exhibit large deflation, and surgery results in better esthetic results (Fig. 1). It is important to assess the surrounding areas, especially the lateral torso and dorsal breast (Fig. 2) with regard to the sagging and quality of skin, remaining fat, and presence of stretch marks, indicating combined surgeries in this area that aim to achieve good results in the entire affected area.

Figure 1 - Patient with marked sagging without lipodystrophy.

Figure 2 - Assessment of surrounding areas.
METHODS
For decades, several established techniques and several Brazilian and foreign authors have recommended that the final position of the scar should be in the brachial groove (e.g., Baroudi4,15 and Barouldi & Ferreira14) or 2 cm below the bicep groove. In the present study, 18 patients were asked to choose the position of the final scar: in the bicep groove (Fig. 3, black) or lower arm (Fig. 4, red). We explained to all patients that it is not always possible to accurately place the scar in the lower arm and showed them photographs as examples. All patients signed an informed consent form before surgery.
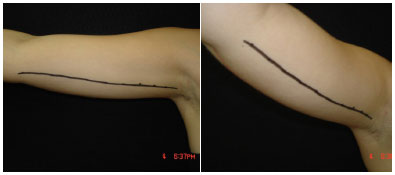
Figure 3 - Position of the scar along the biceps groove.

Figure 4 - Posterior view of the scar position scar in the lower arm, as proposed by (by Aly et al.1).
Marking
Marking was performed 1-2 days before surgery by bidigital maneuver (anterior and posterior) while the patient was sitting with arms abducted at 90 degrees (Fig. 5). An ellipse extending from the armpit to elbow was drawn, passing through the medial epicondyle of the humorous when necessary. In surgeries suited to the lateral trunk, Baroudi14 and Maciel11,12 do not recommend z- or w-plasty but only a small scar in the axillary cavity. After marking, the patient was positioned in the supine position with the arm extended 180 degrees to better visualize symmetry (Fig. 6). Finally, the points were tattooed with methylene blue by using a hypodermic insulin needle.

Figure 5 - Bidigital pinching maneuver to mark the anterior and posterior regions.

Figure 6 - Patient position with arms extended 180 degrees, allowing better assessment of symmetry.
Technique
The surgery was performed under local anesthesia and sedation. The patient was positioned with the arms abducted 90 degrees relative to the body. First, an incision was made according to the anterior marking (Fig. 7); this was followed by bipartition of the flaps for better reliability (Fig. 8), because there is a tendency to over-mark when the arm is abducted owing to tissue ptosis. After (Fig. 9) without using drains or leaving a dead resection, suturing was performed in 3 or 4 layers.

Figure 7 - Anterior incision.

Figure 8 - Flat bipartition in 3 different patients.
RESULTS
The degree of patient satisfaction with brachioplasty is more important than that with thigh surgery, because the arm is more exposed than the thigh, making it harder to hide deformities. Therefore, we recommend the final position of the brachioplasty scar should be in the lower arm. All patients in the present study were very satisfied with the scar location and final results. Complications including wound dehiscence, scar hypertrophy, and scar enlargement were observed.
(Fig. 9) without using drains or leaving a dead space to prevent strain.

Figure 9 - Suture in four layers.
During the postoperative period, we instructed patients to rest their arms for 15 days and they were not allowed to lower them; tape or elastic bands and silicon blades were used for 2 months. The patients were warned about the possibility of edema in the limbs, particularly the hands; the edema spontaneously regressed after approximately 15 days. We recommended 12-15 lymphatic drainage sessions for patients who underwent lipoaspiration.
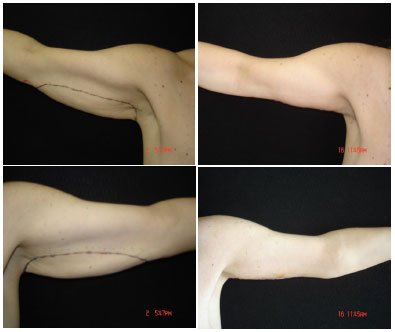
CLINICAL CASE 1- Preoperative and 24-month postoperative aspects: the final scar is not visible when viewed anteriorly.

CLINICAL CASE 2- Preoperative and 4-year postoperative aspects: good results without a scar visible when viewed anteriorly.
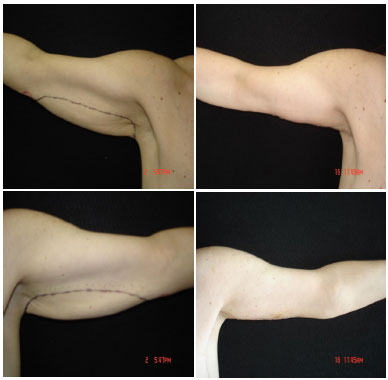
CLINICAL CASE 3- Preoperative and 2-year postoperative aspects: the scar is not visible in the photograph taken in the anterior view.

CLINICAL CASE 3.5- Day 12 postoperatively; ecchymosis and reddening of the scar. The scar is visible when viewed posteriorly.

CLINICAL CASE 4- Scar quality 2 months post-operatively from the right and left sides.
DISCUSSION
For many years, brachioplasty was rarely performed by plastic surgeons primarily because of the visible scars as well as high rates of complications. However, these techniques and strategies have reemerged with the advent of gastroplasty and better scar positioning, resulting in a high degree of satisfaction in both patients and surgeons. In order to achieve good overall results, it is important that patients are carefully selected for surgery and provided necessary information, and that preoperative marking and surgical technique are properly executed.
CONCLUSION
The final placement of the gastroplasty scar in the lower arm is a safe and easily reproducible surgical procedure that results in satisfactory outcomes in patients and surgeons. The technique described herein allows the scar to be hidden in the lower arm and ensures that the scar is not visible to the patient or whoever is in front of the patient during arm abduction.
REFERENCE
1. Posse RP. Cirurgia estética. Buenos Aires; 1946.
2. Correa-Iturraspe M, Fernandez JC. Dermolipectomia braquial. Prensa Med Argent. 1954;41(34):2432-6.
3. Pitanguy I. Correction of lipodystrophy of the lateral thoracic aspect and inner side of the arm and elbow dermosenescence. Clin Plast Surg. 1975;2(3):477-83.
4. Baroudi R. Dermatolipectomy of the upper arm. Clin Plast Surg. 1975;2(3):485-94.
5. Franco T, Rebello C. Cirurgia estética. Rio de Janeiro: Atheneu; 1977.
6. Illouz IG. Une nouvelle technique pour les lypodistrophies localisées. Rev Chir Esth Fran. 1980;6(9):4-19.
7. Juri J, Juri C, Elías JC. Arm dermolipectomy with a quadrangular flap and "T" closure. Plast Reconstr Surg. 1979;64(4):521-5.
8. Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96(4):912-20.
9. Marques B, Abramo A. Dermolipectomia braquial. Rev Soc Bras Cir Est Reconst. 1996; 11(1).
10. Aly AS, Cram AE. Brachioplasty. In: Aly AS, ed. Body Contouring after massive weight loss. 1st ed. St Louis: Quality Medical Publishing; 2006. p.303-33.
11. Maciel E. Cirugía plástica pós-bariátrica em brazos. Cirugía Plástica Estética y Reconstructiva, v-494, p.4839-46, 2008.
12. Lima Junior EM. Tratado de cirurgia plástica Após grandes perdas ponderais. São Paulo: Atheheu; 2010. p.96-116.
13. Kathib H. Clasificación de lap ptosis braquial: estratégias de tratamiento. Plast Reconst Surg (español). 2009;(13):276-81.
14. Baroudi R, Ferreira CAA. Braquioplastias. In: Mélega JM, Baroudi R, eds. Cirurgia Plástica: Fundamentos e Arte - Cirurgia Estética. São Paulo: Medsi; 2009. p.60-84.
15. Baroudi R. Braquioplastia. Cirurgia do Contorno Corporal, cap. 5; 2009. p.60-84.
1. Postgraduate in hospital administration, President of the Latin-American Federation of Burns
2. Full member of SBCP [Brazilian Society of Plastic Surgery], Plastic Surgeon of HGF and IJ
3. Medical UNIFESP and resident of General Surgery at UNIFESP
Edmar Maciel Lima Junior
Rua Visconde de Mauá, 1650 ap. 801, Aldeota
CEP: 60125-160, Fortaleza - Ceará
Article received: 27/08/2012
Article accepted: 27/09/2012


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter