

Original Article - Year 2013 - Volume 28 -
Assessing the quality of records in the dressing charts, performed by nursing
Avaliação da qualidade dos registros dos curativos em prontuários realizados pela enfermagem
ABSTRACT
OBJECTIVE: To evaluate the quality of the records of healing performed by nursing records.
METHOD: Descriptive study with retrospective documentary analysis. This study was conducted in adult Intensive Care Unit of the Hospital of Samuel Libanius.
RESULTS: 65 (65%) of annotations not present in this type of tissue lesion, 85 (85%) had no type of exudate, 100 (100%) indicated no measurement of the wound and in 80 (80%), the appearance of margin and center of the lesion were not recorded. 100 (100%) of the notes were with abbreviation, 59 (59%) had no clarity of notes and 80 (80%) had grammatical errors and language of 80 (80%) contained incorrect errata and technical terminologies. 75 (75%) of nursing prescriptions were not checked and in 54 (54%) of the notes the letter was not legible.
CONCLUSION: In this study the authors concluded that the quality of the ratings of nursing care are limited and inadequate.
Keywords: Quality of Health Care. Quality Assurance, Health Care. Nursing. Bandages.
RESUMO
OBJETIVO: Avaliar a qualidade dos registros dos curativos realizados pela enfermagem em prontuários.
MÉTODO: Estudo descritivo, com análise documental retrospectiva. Este estudo foi realizado na Unidade de Terapia Intensiva adulto do Hospital das Clínicas Samuel Libânio.
RESULTADOS: Sessenta e cinco (65%) das anotações não descreviam qual o tipo de tecido presente na lesão, 85 (85%) não apresentavam tipo de exsudato, 100 (100%) não indicavam mensuração da ferida, e em 80 (80%) o aspecto da margem e centro da lesão não foram registrados. Todas as (100%) anotações estavam com abreviatura, 59 (59%) das anotações não apresentavam clareza, 80 (80%) apresentavam erros gramaticais da linguagem e 80 (80%) continham terminologias técnicas erratas e incorretas. Setenta e cinco (75%) das prescrições de enfermagem não estavam checadas, e em 54 (54%) das anotações a letra não estava legível.
CONCLUSÃO: Por meio deste estudo, os autores concluíram que a qualidade das anotações da assistência de enfermagem são limitadas e inadequadas.
Palavras-chave: Qualidade da assistência à saúde. Garantia da qualidade dos cuidados de saúde. Enfermagem. Curativos.
An audit is defined as the systematic and formal assessment of an activity, performed by a person who is not directly involved in the execution of the activity, to determine whether the professional in charge conducted the activity according to its goals. Auditing can also be emphasized as a formal evaluation carried out by staff not directly responsible for the execution of the service being evaluated, and that contributes toward the assessment of an organization's quality1.
Auditing is a tool for controlling the quality of a nursing team's work, and is aimed at improving the quality of the service being provided2. Thus, nursing care may be evaluated by using documentation that reflects the quality of the care provided3.
Auditing is also defined as the official examination of nursing documentation with the purpose of assessing, after the patient's discharge, the quality of attendance so as to improve nursing care4,5. Recording of notes is one of the most important forms of communication in nursing; its objectives are (i) to establish an effective communication between the nursing team and all other professionals involved in human care; (ii) to serve as a basis for the drafting of a patient's care plan; (iii) to contribute to the assessment of the care that was provided; (iv) to be used in monitoring the progress of the patient; (v) to serve as a legal document, both for the patient and for the nursing team, concerning the care that was provided; and (vi) to contribute to the auditing process of nursing and assist in nursing teaching and research6.
In the study conducted by Setz and D'lnnocenzo4, the authors evaluated the quality of nursing documentation in patient medical records through an audit. The authors concluded that the study identified several nonconformities, which were analyzed in cooperation with the Nursing Directorate and with the Process Improvement Groups of the Nursing Directorate of the hospital under study, which allowed new goals and strategies to be proposed to improve the quality of nursing care and of the nursing documentation. Therefore, the aim of this study is to evaluate the quality of wound documentation, prepared by nursing professionals, in patient medical records6.
METHOD
This is a descriptive study with a retrospective documentary analysis. The study was conducted at the adult intensive care unit (ICU) of the Hospital das Clínicas Samuel Libânio, following approval by the research ethics committee of the Faculty of Health Sciences "Dr. José Antônio Garcia Coutinho."
The data were collected through the evaluation of the Nursing Care Systematization form, which comprises Nursing Documentation and Progress, as well as nursing prescription to patients, included in medical records during the months of May to August 2012.
An instrument for the evaluation of nursing notes in patient medical records was prepared, containing three items-(i) wound-related records: tissue type, exudate type, location of the wound, type of bandage used in dressing, wound measurement, wound type, appearance of the wound's edge, appearance of the wound's center; (ii) note-related records: patient identification, clarity of note, professional's stamp, professional's signature, professional's legible handwriting, time at which the dressing was performed, grammatical errors, incorrect technical terminology, and presence of abbreviations; (iii) records related to the quality of nursing prescription: professional's stamp, checking, clarity of prescription, professional's signature, professional's legible handwriting, and presence of abbreviations.
The inclusion criterion was that all nursing notes had to be recorded in the Nursing Care Systematization forms (Nursing Annotation, Progress and Prescription), included in the patient medical records available at the Medical and Statistical Archiving Service (SAME), in the months of May to December 2012. Data related to nursing diagnoses and nursing prescription were analyzed.
RESULTS
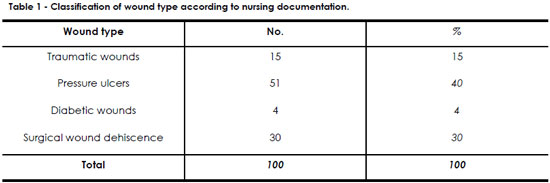
Table 1 shows that 51 (51%) of the notes involved pressure ulcers and 30 (30%) were on surgical wound dehiscence.
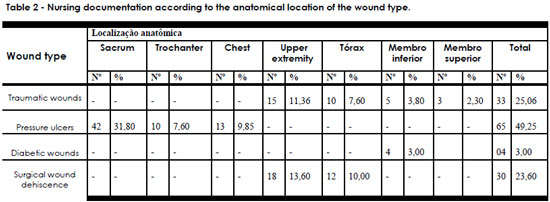
Table 2 shows that, according to the nursing documentation, 65 (49.25%) of patients had pressure ulcers and 33 (25.06%) had traumatic wounds, evidencing that patients presented with more than one wound.
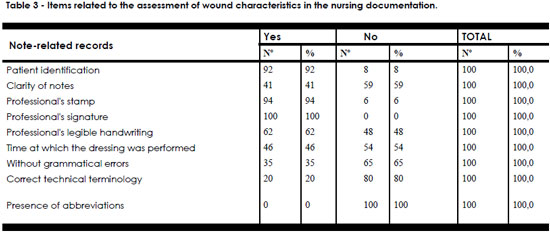
Table 3 shows that there were no records on the type of tissue in 65 (65%) of the cases, on the type of exudate in 85 (85%), on the evaluation of the wound in 100 (100%), on the appearance of the wound's edge in 80 (80%), on the appearance of the wound's center in 80 (80%), and on whether the patient complained of pain in 98 (98%).
Table 4 shows that 100 (100%) of the notes included abbreviations, 59 (59%) were unclear, 65 (65%) showed no grammatical errors, and 80 (80%) did not use the correct technical terminology.
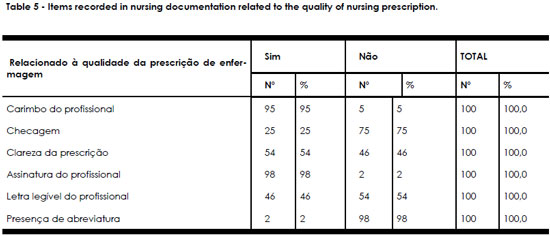
Table 5 shows that 75 (75%) of the nursing prescriptions were unchecked and 54 (54%) of the notes contained illegible handwriting.
DISCUSSION
Wound care is part of a nurse's duty, and the scope of this activity has been expanding in recent years owing to the greater knowledge about the tissue healing process and the scientific and technological advances in nursing care delivered to patients with skin lesions7. This knowledge is required so that the professional can assess the wound and, consequently, decide on the ideal dressing to promote wound healing.
When assessing wounds, the nurse needs to make instrumental decisions and, for this reason, must have a comprehensive knowledge of the anatomy of the skin and of the principles of physiology, tissue repair, and the factors affecting wound repair. Such professionals must know the types of wounds and the different forms of treatment available, while also having the ability to observe loss of tissue; the clinical characteristics of the injury, its location and dimension; presence of exudate; type of tissue; characteristics of the skin surrounding the wound; and presence of pain and signs of infection8,9.
Often, during the assessment of a chronic wound, the professional realizes whether the amount of necrosis and exudate has increased, or whether the lesion is ready to receive a skin graft or flap. The professional must then consult the plastic surgeon about the possibility of surgical debridement, skin graft, and flap application.
A study on the role of plastic surgery in complex wound treatment, performed at a tertiary care hospital, concluded that the plastic surgeon had a significant influence on the treatment of complex wounds by adopting the most recent surgical treatment, which contributed toward effectively solving the cases10,11.
General nursing care, as well as the care provided along with wound treatment, must be systematically recorded to ensure qualified nursing assistance. This requires the formulation of nursing diagnosis, prescription, progress, planning, implementation, and assessment of actions. In this regard, the recording of nursing evaluations and interventions must be performed clearly and precisely so that data are not omitted and therefore do not damage the care provided to the patient9.
Since nursing services are involved in patient care 24 hours a day, nurses become responsible for the permanent evaluation of wound progress. Unfortunately, it is apparent that this does not always mean proper attendance, because in most public sector hospitals, there is a shortage of nursing professionals (nursing assistants and nurses). Because of this shortage, the nursing team has to provide assistance beyond the volumes stipulated by the professional order (Coren) according to the size of the team. Because of the work overload, nursing professionals who are considered the most qualified to assess wounds end up delegating such duty to nurse assistants. In turn, the nurse assistant, also because of work overload, might make an incorrect assessment of the wound and, as a result, fail in using the most appropriate product for the patient. Another aggravating circumstance in most of the public sector hospitals is the lack of a dressing team, considering that such teams have already been proven to be essential for the efficiency of recovery and for decreasing the length of the hospital stay of patients.
Another problem is a medical professional who, for a lack of commitment or any other reason, does not perform an appropriate follow up of the patient for systematic anamnesis, that when he/she decides to request an assessment by a plastic surgeon, the wounds are in such an advanced state that appropriate treatment, and even the patient's full recovery, has become compromised. In addition to all of the above, the nursing team may be missing other professionals such as physical therapists and nutritionists. In contrast, private institutions have sufficient human resources to ensure proper treatment of wounds. To solve this problem, especially in public institutions, the creation of dressing teams that include nursing assistants, nurses, plastic surgeons, nutritionists, and physical therapists is required.
In 65 (65%) of the notes assessed in this study, the type of tissue was not mentioned; in 85 (85%), the type of exudate was missing; in 100 (100%), there were no records on wound measurement; and in 80 (80%), the appearance of the wound's edge and center was not recorded. Furthermore, in 98 (98%) of the notes, there was no record on whether the patient complained of pain.
Assessing a wound means describing its clinical characteristics, location, and size; the skin characteristics; the amount of exudate; the smell of the wound; the type of tissue involved in the lesion; and the presence or absence of pain. These data must be recorded as they are factors that interfere with wound healing12.
Systematic recording of the evaluation and the type of dressing used to treat the wound is a fundamental element to ensure qualified nursing assistance. Documentation about interventions must be clear and precise so that the data are not omitted and do not affect the care provided. Recording of wound evaluation and progress must be selectively performed by using instruments that facilitate the taking of notes on the characteristics and factors delaying the wound healing process; thus, it is necessary that the professionals speak the same language9. This means that the creation and implementation of protocols for wound prevention and treatment, as well as the formation of a multidisciplinary team (plastic surgeon, nurse, nutritionist, physical therapist), are crucial. In their study, Silva and Dias13 concluded that nursing professionals are not aware of the importance of reflexive writing; recording of care is often conducted mechanically, with use of repetitive sentences, catchphrases, and vague terms, which render the complete documentation of care impossible.
The recording of the evaluation, progress, and dressing of wounds not only enables follow up of care and allows computing the statistics of the different attendances, but it also acts as a source of consultation and legal documentation that enables the improvement of the quality of care9.
Concerning the quality of nursing documentation, this study found that 75 (75%) of the nursing prescriptions were unchecked and the handwriting was not legible in 54 (54%) of the notes.
Nursing records are a way to demonstrate the work conducted by the nursing team and is a relevant indicator of the quality of care. Incorrect filling of forms and, especially, a lack of periodicity and continuity are factors that irreversibly block any kind of evaluation, certification, creation of indicators, and even evidence-based inquests that may also provide legal support to the professional and the institution14.
Nursing documentation is the principal proof of the provision and the quality of care. This study investigated the documentation written by nurses and nursing assistants at a hospital school. After the ethical requirements were met, 71 notes made in the first 72 hours after patient admission to the ICU, and to the sector where the patient was later transferred, were analyzed. The contents of the notes were grouped into 15 items. The results showed that the number of notes does not correspond to the requirements of the institution. It was observed that the two categories produced records that, for the most part, include the same items and give disproportionate importance to the biological dimension. Information on the conscience level and test/evaluation results, important for the type of patients, such as the ones studied herein, appeared only a few times. The psycho-social-spiritual dimension was considered only once. Therefore, we conclude that the nursing notes/records, although widely discussed, need to be improved15.
A previous study reported on how to evaluate, through audits, the quality of nursing notes in patient medical records. In the qualitative analysis of the medical records, 26.7% were considered poor, 64.6% regular, and 8.7% good. A compromise can be observed between the safety and patient care dimensions, besides the difficulty in measuring the care results from the nursing team16. In a study where 134 patient medical records were assessed through an audit, the results revealed that only the records pertaining to postoperative nursing prescriptions, observation of signs and symptoms, and postoperative notes were considered complete. The notes on the appearance and progress of skin lesions and those concerning discharge were incomplete in 73.9% and 97% of the cases under analysis, respectively. These results indicate the need for continuous education, monitoring, and assessment of nursing records with a view to improve them as well as the care provided17.
In another study, the authors observed that nursing records were complete for most of the items: nursing history (99.9%), multidisciplinary progress (80.0%), and risk assessment (99.6%). Concerning the correctness of completion, the most relevant findings were as follows: 88.4% of all nursing prescriptions were classified as correct, whereas records on nursing diagnosis and progress were classified as incorrect in 58.7% and 64.6%, respectively. Concerning the identification of the nurse, 98.3% were complete in the nursing history section, 87.9% in progress, and 75.4% in nursing diagnosis and prescription18.
In another study, the authors found that the nursing documentation was, in most of the patient medical records, incorrect or absent. The patient identification information was incorrect in most of the records. Some notes were written by pencil (and are therefore subject to alteration), of questionable legal and support value, with incomplete analyzed data, or were incorrect or absent in half of the assessed records19.
Recording of the care provided to the patient on the respective medical record encompasses several dimensions and protects, ethically and legally, both the professional in charge for the care and the patient. When such records are limited and inadequate, the care that is given, as well as the image of the institution and of the nursing team, becomes compromised. There is a compromise between the safety and patient care dimensions, besides the difficulty in measuring the care results from the nurses' practice.
The standardization of the recording of nursing notes is necessary, as there are flaws concerning grammatical adjustments of formal language, preciseness, shortness, legibility, identification, and technical terminology16.
This study is limited by the lack of comparison against adequate recording, as well as the failure to determine the impact of incomplete notes during the hospitalization period on wound treatment and progress.
CONCLUSION
From the results of this study, it is possible to conclude that the quality of nursing notes, pertaining to patients with skin lesions, is limited and inadequate since information on the clinical condition of the patient is necessary to follow up and evaluate the care assistance that is provided.
REFERENCES
1.Faraco MM, Albuquerque GL. Auditoria do método de assistência de enfermagem. Rev Bras Enferm. 2004;57(4):421-24.
2.Pinto KA, de Melo CM. Nurses' practice in health audit. Rev Esc Enferm USP. 2010;44(3):671-8.
3.Costa MS, Forte BP, Alves MD, Viana JF, Oriá MO. Nursing audit as a professional marketing strategy. Rev Bras Enferm. 2004;57(4):497-9.
4.Setz VG, D'Innocenzo M. Evaluation of the quality of nursing documentation though the review of patient medical records. Acta Paul Enferm. 2009;22(3):313-7.
5.Phaneuf MC. A nursing audit method. Nurs Outlook. 1964;12:42-5.
6.Pereira LL, Takahashi RT. Auditoria em enfermagem. In: Kurcgant P, coord. Administração em enfermagem. São Paulo: Editora Pedagógica e Universitária; 1991. p.215-22.
7. Tayar G, Peterlini MAS, Pedreira MLG. Proposta de um algoritmo para seleção de coberturas, segundo o tipo de lesão aberta em crianças. Acta Paul Enferm. 2007;20(3):284-90.
8. Borges EL, Chianca TCM. Tratamento e cicatrização de ferida: Parte 1. Nursing. 2000;3(21):24-9
9. Bajay HM, Pedrosa MMO, Lourenço MTN, Cortez SL, Paula MAB. Registro de avaliação e evolução de feridas: subsídios para reflexão e mudanças. Rev Estima. 2003;1(2):20-9.
10.Coltro PS, Ferreira MC, Batista BP, Nakamoto HA, Milcheski DA, Tuma Júnior P. Role of plastic surgery on the treatment complex wounds. Rev Col Bras Cir. 2011;38(6):381-6.
11. erreira MC, Tuma P Jr, Carvalho VF, Kamamoto F. Complex wounds. Clinics (Sao Paulo). 2006;61(6):571-8.
12. Santos VLCG, Azevedo MAJ, Silva TS, Carvalho VMJ, Carvalho VF. Adaptação transcultural do Pressure Ulcer Scale for Healing (PUSH) para a língua portuguesa. Rev Latinoam Enferm. 2005;13(3):305-13.
13. Silva MJP, Dias DC. O registro da prática da enfermagem: da realidade do cuidado rotineiro à utopia do cuidado individualizado. Nursing (São Paulo). 1999;2(11):21-6.
14. Araújo MV, Simões C, Silva CL. Auditoria em enfermagem. Rev Bras Enferm. 1998;31(4):466-77.
15. Matsuda LM, Carvalho ARS, Évora YDM. Anotações /registros de enfermagem em um hospital-escola. Ciênc Cuid Saúde. 2007;6(Supl.2):337-46.
16. Sets VG, D'Innocenzo M. Evaluation of the quality of nursing documentation though the review of patient medical records. Acta Paul Enferm. 2009;22(3):313-7.
17. Venturini DA, Marcon SS. Nursing reports in a surgical unit at a school hospital. Rev Bras Enferm. 2008;61(5):570-7.
18. Franco MTG, Akemi EN, D'Inocento M. Evaluation of the nursing records in the medical records of patients hospitalized in an internal medicine unit. Acta Paul Enferm. 2012;25(2):163-70.
19.Draganov PB, Reichert MCF. Avaliação do padrão dos registros de Enfermagem. Rev Enferm UFPE on line. 2007;1(1):36-45.
1. Student of the Undergraduate Nursing Course, Universidade do Vale do Sapucai, Pouso Alegre-MG, Brazil
2. Student of the Undergraduate Nursing Course, Universidade do Vale do Sapucai, Pouso Alegre-MG, Brazil
3. PhD, Professor of the Professional Masters Course in Applied Health Sciences, Universidade do Vale do Sapucai-UNIVÁS, Pouso Alegre-MG, Brazil
4. MSc in Nursing, RN, PhD, MSc, Full Professor and Coordinator of the Nursing Course, Universidade do Vale do Sapucai (UNIVÁS), Pouso Alegre, MG, Brazil
Rodrigo Galvão Bueno Gardona
Av-Francisco de Paula Quintaninha Ribeiro, 280/134, Bl 01
CEP-04330-020. São Paulo, SP, Brasil
Article received: 05/09/2013
Article accepted: 05/10/2013
This study was conducted at the Hospital das Clínicas Samuel Libânio, Pouso Alegre, RS, Brazil.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter