

Original Article - Year 2013 - Volume 28 -
Use of blades of 0.7 to 1mm in diameter and coronal incisions in hair transplantation: Surgical approach to improve density and natural results
Uso de lâminas de 0,7 a 1mm de largura e incisões coronais no transplante capilar:Tática cirúrgica para melhorar a densidade e naturalidade
ABSTRACT
INTRODUCTION: The hair transplant evolved greatly in the past two decades primarily by the use of microscopes to make follicular units. The use of Micro blades is another step to reduce the surgical trauma and increase the naturalness of the result. Coronal incisions help to maintain the correct direction of hair placed. The goal of this work is to show our experience with the use of blades 0.7 to 1mm in diameter, with coronal incisions for hair transplantation.
METHOD: We evaluated 131 consecutive surgeries from June 2011 to June 2012, in which all patients operated on by the same surgeon with the use of microblades 0.7 to 1mm wide using coronal incisions.
RESULTS:The postoperative results were considered satisfactory by the patients and the surgical team.
CONCLUSION:The use of small blades with coronal incisions helps to give more density with little surgical trauma. The results were considered natural with good cosmetic density.
Keywords: Hair Follicle/Transplantation.Scalp/Surgery.SurgicalInstruments.
RESUMO
INTRODUÇÃO: O transplante capilar evoluiu muito nas últimas duas décadas, principalmente com o uso de microscópios para lapidar unidades foliculares. A utilização de microlâminas é mais um avanço para diminuir o trauma cirúrgico e aumentar a naturalidade do resultado. As incisões coronais ajudam a manter a direção correta dos cabelos colocados. O objetivo deste trabalho é mostrar nossa experiência com o uso de lâminas de 0,7 a 1 mm de diâmetro, com incisões coronais para o transplante capilar.
MÉTODO: Foram avaliadas 131 cirurgias consecutivas de junho de 2011 a junho de 2012, em que todos os pacientes foram operados pelo mesmo cirurgião, com o uso de microlâminas de 0,7 a 1 mm de largura utilizando a técnica coronal para a incisão.
RESULTADOS: Os resultados pós-operatórios foram considerados satisfatórios pelos pacientes e pela equipe cirúrgica.
CONCLUSÃO: O uso de lâminas pequenas nas incisões coronais promove maior densidade com pouco trauma cirúrgico. Os resultados foram considerados naturais e com boa densidade cosmética.
Palavras-chave: Folículo Piloso/Transplante. Couro Cabeludo/Cirurgia. Instrumentos Cirúrgicos.
Hair transplantation has undergone intensive development in the last decades since the 4-mm punches were popularized by the American surgeon Orentreich1 in 1959. Meanwhile, temporo-parieto-occipital flaps, which were first described by Juri2, had been used until the use of microscopes to cut follicular units. In 1987, the American surgeon Bobby Limmer was the first to routinely use stereoscopic microscopes in hair restoration surgery3. Thereby, dissection became possible, as well as placement of follicular units, which are the minimum units of the pilosebaceous structure4. Follicular units may emerge from one pore with one to three hair strands. Units with more than three strands are rare. When implanted in the bald area, follicular units simulate the normal hair scalp; therefore, the artificial-looking result of tufted hair, which comprises various follicular units in one orifice, that is commonly observed in conventional methods of hair transplantation is prevented.
Independent of the materials that make up the instruments used to create the required orifices, such as blades or needles, the larger the instrument, the greater the trauma to the hair scalp. Such fact may compromise the vascularization and viability of the implanted grafts. The large space between grafts due to large orifices leads to a low-density hair growth per square centimeter. For this reason, to achieve natural results, the diameter of the blades and needles used has been decreasing, minimizing trauma but increasing the technical difficulty of graft placement.
The direction of the hair implanted is of vital importance for aesthetic results. Coronal incisions, a technique originally described by Hasson and Wong5, allow for the control of the direction toward which the graft is will heal.
This article describes our experience with microblades of 0.7 to 1 mm in diameter along with the use of coronal incisions in hair transplantation.
METHODS
A total of 131 consecutive patients underwent surgery by the same surgeon between June 2011 and June 2012. The patients underwent surgery under local anesthesia and sedation, and were discharged from the hospital 2 hours after the surgery.
The patients had different levels of baldness, with a Norwood classification6 between stages III and VI.
Surgical Technique
Donor area
Xylocaine was infiltrated at 0.5% with diluted adrenaline at 1:100,000. A strip of scalp, ranging in width from 1.2 to 2 cm depending on the mobility of the hair scalp, was removed from the supragaleal plane. The resection was advanced until the anterior region of the temples particularly in patients who required a great quantity of grafts. The final suture in the supragaleal plane was performed using 4-0 monocryl and 4-0 mononylon sutures.
Recipient area
The regional anesthetic blockade was applied in the incision arc, located outside the graft recipient site, using 5-mg/mL ropivacaine. The entire recipient area was infiltrated with a physiological saline solution diluted in 1:200,000 adrenaline. Anesthetics were not applied in the recipient region because the regional blockade was sufficient.
Graft placement
Blades of various diameters were used, depending on the size of the grafts each patient required. Blades of 0.7-, 0.8- or 0.9-mm, and 0.9- or 1-mm diameters were used for follicular units with one, two, and three hair strands, respectively. The 1-mm blades are frequently used for curly and thick hair (Figures 1 and 2).

Figure 1 - Blades 0.7, 0.9, and 1 mm in diameter.

Figure 2 - 0.8-mm microblade.
Two graft placement techniques were used. For high-density hair growth in the frontal area, the grafts were implanted via the previous incisions that were used for creating the orifices. Behind the frontal line, the follicular units were implanted in the created orifices. Subsequently, we added more units to the frontal line according to the desired cosmetic density.
All the incisions were performed in the coronal direction to better control the angle of hair growth. The use of coronal incisions also allowed for a more precisely sized incision, as on the sagittal plane, the diameter of the orifice increases according to the angle of the graft placement (Figures 3A and 3B).

Figure 3A - Coronal incision using a 1-mm blade, which produced a 1-mm cut.

Figure 3B - Sagittal incision at a 45-degree angle using a 1-mm blade, which produced a 1.4-mm cut.
RESULTS
A total of 131 consecutive patients underwent surgery using microblades to create the coronal incisions. Postoperative crusts shed after a week, and the patients went back to their work routine 2 days after surgery on average.
The results were considered natural with good cosmetic density. However, two patients (1.7%) had lower hair density than expected and again underwent surgery to increase the density.
Preoperative and postoperative results:

Result on the day of surgery with long hair strands

Result after 1 year

Preoperative result

Immediate postoperative result with short hair strands
Result after 1 year
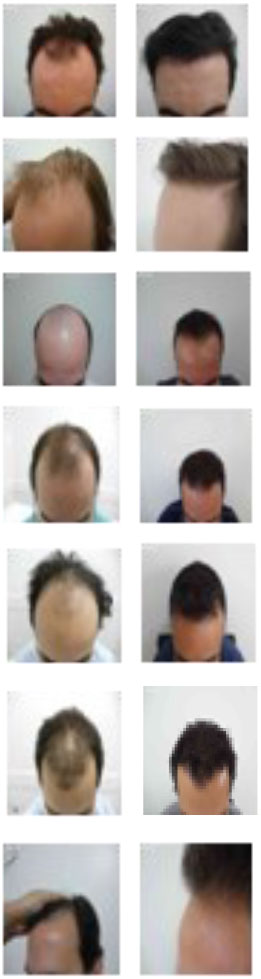
Cases 3 to 9 - Preoperative and postoperative results of the placement of 2,500 to 3,000 follicular units.

Close 1 a 4 - Detailed results of the final graft placement in the frontal line.
DISCUSSION
The use of follicular units has revolutionized hair transplantation surgery, as it provides natural-looking results, which was not possible with the previous method of placement of several units in one orifice. The use of stereoscopic microscopy is a modern surgical routine procedure in hair transplantation, with which follicular units are cut with preservation of an adequate amount of fat around the follicle to protect the follicle during graft placement. Fat grafts, that is, a large amount of fat around the follicle, should be avoided; only a small amount of fat is necessary to keep the follicular unit intact and protected. Therefore, small orifices can be used and provide higher hair density.
Seager7 was the first surgeon to describe the one pass technique, whereby a good hair density can be achieved in just one procedure by placing orifices close to each other with the aid of needles 0.8 to 1.2 mm in diameter. Many surgeons prefer the use of needles because the lumen is useful in graft placement.
One of the Brazilian surgeons who were responsible for the great advancement of modern hair transplantation was Dr. Carlos Uebel, who in the late 1980s introduced the use of micrografts and minigrafts for a more natural-looking outcome of hair transplantation8. Since that time, the instruments have become more refined and many surgeons have started to use microblades and needles smaller than 1.2 mm, instead of large blades, for creating orifices.
Depending on the instrument used, the size, depth, and width of orifices vary. To minimize trauma, the instrument should ideally mimic the shape and size of the graft. In addition, the following facts should be considered: thousands of punctures should be created, and the lesser the trauma to the tissues, the better the graft integration. Dr. Wong5, a surgeon practicing in Canada, was the first to publish the routine use of coronal incisions and obtain promising results with the use of 0.6- to 1-mm-wide blades. This demonstrates that the type of instrument varies according to the surgeon's preference and that good results can be achieved using needles or blades, as long as they are small enough and used with the appropriate graft placement technique. Efficient manipulation of grafts is essential for good hair integration, as well as keeping them always moisturized, as described by the Brazilian surgeon Marcelo Gandelman9. In addition, the anterior line outline is essential for a natural-looking result, as described by the Brazilian surgeon Fernando Basto10.
Creating orifices using blades generates a minor trauma because they produce a linear cut and do not have the sharp round circumference of needles. Moreover, blades can be adjusted to the size of the graft by customizing their lengths (Figure 4). This way, adequate cosmetic density with a minor trauma can be achieved. Hair growth densities may vary from 20 to 70 units/cm2, depending on size of the strand, color contrast of the hair against the hair scalp, type of hair (curly or straight), and recipient site. Generally, as many strands as necessary are transplanted to achieve a satisfactory cosmetic density.

Figure 4 - A blade that mimics the maximum size of the graft.
The direction of the strands is essential for a natural-looking result. The follicular units should be transplanted in the exact same direction as that of the original strands. In case of advanced baldness, the remaining fluff is used to determine the direction of the transplanted strands.
By using coronal incisions, total control over the positioning of the grafts toward the antero-posterior direction can be achieved for a more desirable aesthetic result. The elevation of the angle of the strands should not be too high, as this creates an artificial-looking result. Unlike coronal incisions, sagittal incisions usually results in a slight vertical elevation of the graft (Figure 5), usually approximately 10 degrees or more, depending on the size of the blade. Therefore, the coronal incision is ideal to achieve total control of the position of the hair, considering that the hair may change position to the right or left, but not upward or downward. This technique is especially ideal for the temples, where the elevation should be at a minimum.

Figura 5 - A strand elevated after cicatrization from a sagittal incision.
Small incisions are important to achieve good results. A coronal incision made with a 1-mm blade always produces a 1-mm cut. By contrast, a sagittal incision made with a 1-mm blade produces a 1.4mm cut when performed in a 45-degree angle. In a mega session, severe trauma may interfere in the vascularization and integration of the grafts. Nakatsui11 achieved excellent results by using 0.6- to 1.0-mm blades and making incisions at close intervals, producing good hair density. However, the technique has disadvantages, including longer surgical duration from creating more orifices and thus placing more grafts, and higher risk for trauma to the hair follicles during placement. However, it presents advantages such as higher hair density, more natural-looking result, and greater patient satisfaction.
In clinical practice, the use of various types of instruments has been demonstrated to present good results, including the use of needles first reported by Seager and the use of blades first described by Wong to produce high hair density. Aside from a less traumatic method of follicle placement, utilization of small instruments, along with the surgeon's experience and ability, seem to be one of the most important factors for achieving good results. Therefore, the instrument most compatible with the graft in terms of shape and size should be used.
Based on the experience of the present author, the learning curve for the utilization of microblades is steep, as it requires more experience and the use of more potent magnifying glasses for graft placement. However, with adequate training, surgeons can perform graft placement with less trauma as possible, and achieve good and consistent results.
CONCLUSION
By using microblades varying from 0.7 to 1 mm in diameter, better natural-looking results can be achieved in hair transplantation. Obtaining high hair density is the greatest advantage of the technique, along with minimal surgical trauma. In this study, the use of coronal incisions was useful in achieving an adequate angle of hair growth.
REFERENCES
1. Orentreich N. Autografts in alopecias and other selected dermatological conditions. Ann N Y Acad Sci. 1959;83:463-79.
2. Juri J. Use of parieto-occipital flaps in the surgical treatment of baldness. PlastReconstr Surg. 1975;55(4):456-60.
3. Limmer BL. Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation.J DermatolSurgOncol.1994;20(12):789-93.
4. Headington JT. Transverse microscopic anatomy of the human scalp.A basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120(4):449-56.
5. Nakatsui T, Wong J, Groot D. Survival of densely packed follicular unit grafts using the lateral slit technique. Dermatol Surg. 2008;34(8):1016-22.
6. Norwood O. Alopecia: classification and incidence. In: Stough DB, HaberRS, eds. Hair replacement: surgical and medical.Philadelphia: Mosby; 1996. p.13-9.
7. Seager DJ. The "one-pass hair transplant" - a six year perspective. Hair Transplant Forum Int. 2002;12(1):176-8.
8. Uebel CO. Micrografts and minigrafts: a new approach for baldness surgery. Ann PlastSurg. 1991;27(5):476-87.
9. Gandelman M, Mota AL, Abrahamsohn PA, De Oliveira SF. Light and electron microscopic analysis of controlled injury to follicular unit grafts. Dermatol Surg. 2000;26(1):25-30.
10. Basto FT, Lemos P. Irregular and sinuous anterior hairline in the capillary micrograft. Rev Soc Bras Cir PlastEstetReconstr. 1996;11(2):15-22.
11. Nakatsui TC. Doing away with incision length. Hair Transplant ForuInt. 2004;14:149-50.
Specialist member of the Brazilian Society of Plastic Surgery, member of the International Society of Hair Restoration Surgery, plastic surgeon graduated at the Faculty of Medicine, University of São Paulo, São Paulo/SP, Brazil
Alan Wells
R. Mato Grosso, 306 cj 1402
Higienopolis, São Paulo, SP CEP: 01230-040
Article received: 07/06/2013
Article accepted: 25/11/2013
Wells Clinical, SP - Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter