

Original Article - Year 2013 - Volume 28 -
Abdominoplasty: effectiveness of classification of Bozola and Psillakis - 27 years of note from the author
Abdominoplastias: efetividade da classificação de Bozola e Psillakis - 27 anos de observação do autor
ABSTRACT
INTRODUCTION: The author recalls the classification proposed by Bozola and Psillakis in 1988, and "aesthetic pathologies" abdominal divided into 5 groups identical to initial treatment in this segment body as excess skin, subcutaneous fat trunk, diastasis of the rectus muscles, external obliques, and deployment vertical position of the navel. Proposed model abdomen aesthetically beautiful like "lira" as he had done with elevations and depressions, highlights and shadows, creating relief. Define beauty and possibility of its reproduction.
OBJECTIVE: To assess the practicality of their diagnosis and treatments of the proposed classification and evolution of the same in the 27 subsequent years with different tactics from those described initially, keeping unchanged the classification.
METHOD: Describes the five treatment groups and percentages of each of the last 200 operated cases. 614 cases were operated from 2001 to 2011, with possible outcomes to obtain.
RESULTS: The classification was effective in 99% of the operated cases.
CONCLUSION: The classification proposed by Bozola and Psillakis remains unchanged, the treatments included new tactics, now more extensive and intense liposuction (vibroliposuction) plications of the rectus and obliques through tunnels hipsters in areas without major perforating vessels that supply skin and subcutaneous tissue of the abdomen, it refixando aponeurotic wall, reducing seroma and hematoma. And reducing traction and skin resection, with better quality of scars, and results.
Keywords: Abdominoplasty. Abdomen/Surgery. Liposuction.
RESUMO
INTRODUÇÃO: O autor recorda a classificação proposta por Bozola & Psillakis em 1988, e as "patologias estéticas" abdominais divididas em cinco grupos idênticas à inicial, no tratamento desse segmento corporal, conforme excedente de pele, gorduras subcutâneas do tronco, diastasis dos músculos retos, oblíquos externos, e posição de implantação vertical do umbigo. Propõe modelo de abdome esteticamente bonito semelhante à "lira", como havia feito, com saliências e depressões, brilhos e sombras, criando o relevo. Define beleza e possibilidade de sua reprodução.
OBJETIVO Analisar a praticidade de diagnósticos e respectivos tratamentos da classificação proposta, e evolução dos mesmos nos 27 anos subsequentes, com táticas diferentes das descritas inicialmente, mantendo inalterada a classificação.
MÉTODO: Descreve o tratamento nos cinco grupos e porcentagens de cada um nos últimos 200 casos operados. Seiscentos e catorze casos foram operados de 2001 a 2011, com os resultados possíveis de se obter.
RESULTADOS: A classificação foi efetiva em 99% dos casos operados.
CONCLUSÃO: A classificação proposta por Bozola & Psillakis permanece inalterada, os tratamentos incluíram novas táticas, atualmente com mais extensa e intensa lipoaspiração (vibrolipoaspiração), plicaturas dos músculos retos e oblíquos através de túneis descolados em áreas sem vasos perfurantes importantes que irrigam pele e subcutâneo do abdome, refixando-o a parede aponeurótica, reduzindo seromas e hematomas. E redução da tração e ressecção de pele, com melhor qualidade das cicatrizes, e dos resultados.
Palavras-chave: Abdominoplastia. Abdome/Cirurgia. Lipoaspiração.
Based on their experience since 1982, in 1988, Bozola and Psillakis1 proposed a new concept of the aesthetic form of the abdomen as well as a classification for abdominoplasty candidates in which the various committed segments were grouped according to their treatment. This evolved into appropriate treatments for each type of "cosmetic condition" according to the following tissues and segments involved: (1) excess skin; (2) excess subcutaneous fat; (3) diastasis and flaccidity of the musculoaponeurotic layer or lack thereof; and (4) vertical placement of the umbilicus, dividing the abdomen into the upper and lower segments. This approach deviates from the previous concept of a single standard surgery. Using the same classification described in 1988, treatment tactics evolved with the advent and development of liposuction2 and subsequently vibroliposuction, involving larger and longer liposuctions3 as well as less undermining, tunneling4,5, and skin resections1,6-10. Treatment approaches were modified, consequently improving results. Therefore, this classification was retained. However, other classifications have emerged since11-13, prompting the need to distinguish what was once a standard treatment into several others according to the more correct diagnosis of existing "aesthetic pathologies."
Aesthetics of the abdominal anatomy
Bozola and Psillakis1 determined that a perfect and beautiful belly is not flat but has contours. The incidence of light on the protrusions and depressions mark lines, points, shadows, and reflections that collectively resemble a lyre1,6,8-10 (Fig. 1A-C).
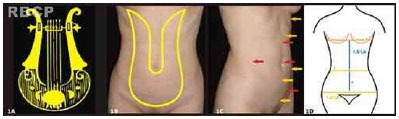
Figure 1 - A - The "lyre;" B - Lyre over the abdomen; C - Depressions of the abdomen causing shadows (red arrows) and protrusions causing reflections (yellow arrows); D - Ratio between the infra- and supraumbilical segments, and waist-to-hip ratio approximately 1:1.5 to 1:1.6 (i.e., the golden ratio).
The shape of the abdomen attracts admiration and is considered beautiful; beauty encompasses shape, volume, dimensions, proportions, reliefs, light, reflection, shadows, colors, posture, and dynamic movement in living organisms. This collectively stimulates the brain's limbic systems and has existed throughout the evolution of humanity. Beauty also encompasses optics, physics, and mathematics and is capable of being replicated; it is not subjective.
Thus, understanding which kinds of features make an abdomen aesthetic is important. What can the plastic surgeon identify in a beautiful anatomical shape and how can they replicate it when correcting aesthetic pathologies during abdominoplasty? What is the anatomical shape of the abdomen?
A standard of beauty of the abdominal form can be established, allowing its replication and avoiding poor cosmetic results of abdomi-noplasties.
Abdominal protrusions are determined by the rectus abdominis muscles, iliac crests, pubis, hypogastrium, and inferior costal margins. Depressions include the supraumbilical midline, umbilicus, iliac fossa, and semilunar lines, which are defined by the insertion of external obliques in the lateral portion of rectus abdominis.
Given a median vertical line passing through the umbilicus from the pubis to a transverse line tangent to the submammary folds inferiorly in the meridian of the breast, the normal position of the umbilicus on the vertical line is in a ratio of 1:1.5 from the lower segment (i.e., infraumbilical) to the upper segment (i.e., supraumbilical)6 (Fig. 1D).
Meanwhile, ratios >1:1.4 and <1:1.6 can be classified as a high and low umbilicus position, respectively. A low position close to the Φ ratio (1:1.618) makes the abdomen visually more beautiful.
The waist-to-hip ratio ranges from 1:1.5 to 1:1.6-the latter is close to the Φ ratio of 1:1.618, which has been considered the golden ratio throughout human history; the golden number or divine proportion is known and universally recognized by architects, musicians, botanists, physicists, and astrophysicists among others14-19. It has marked the limbic brain systems in the evolution of humanity as a standard of beauty, efficiency, harmony, and balance. It is biologically necessary for individual survival and attracts attention20 to the extent that beauty seems intuitive even though it is not.
OBJECTIVE
This study analyzed the effectiveness of the classification of the diagnosis and treatments of the abdomen proposed in 1988 and their evolution in the past 27 years. Although current approaches differ from those described initially, the classification has been maintained.
METHODS
The author proposes 5 different diagnostic groups (GI-GV) with respective treatments. This classification diagnosis was proposed by the same author and co-author in 19881. However, the treatments have changed since then, involving more intense and extensive liposuction from the iliac crest to the submammary fold around the waist circumference as well as less undermining in up to 3 tunnels6; thus, the abdominal flap resembles a myocutaneous flap fed by perforator vessels from the abdominal wall. Smaller skin resections are also performed. All percentages reported hereafter refer to the past 200 consecutive patients operated on by the author.
Group I
Group I (GI) patients represented 20% of all operated patients; they were generally nulliparous women with excess subcutaneous fat in all or some abdominal areas, flanks, the lumbar region, hypochondrium, generally more evident in the infraumbilical region and flanks up to the upper portion of the buttocks. The patients generally had good skin tone. Abdominal muscles also had good tone without diastasis. Therefore, in addition to the anterolateral abdominal wall fat, the entire circumference of the trunk from the inguinal folds to the submammary fold was treated as well.
The subcutaneous fat of the abdomen was treated by liposuction2-4,6 (i.e., vibroliposuction using pneumatic equipment) using 3-mm cannulas or 4 mm in patients with thicker adipose tissue. Incisions were made on the xiphoid process, iliac fossa, flanks, and hypochondrium when required. In general, the whole circumference of the trunk was lipoaspirated.
Infiltration of the areas was always performed with hypoosmolar solution; 2 L was generally used; at most, 3 L was used in patients with large body area and thick adipose tissue. Two liters saline solution comprised 1000 mL saline, 1000 mL distilled water, 10 mg dexamethasone, 2 mL adrenaline (1:1,000), 5000 IU hyaluronidase, and 20 mL 2% lidocaine.
Vibroliposuction was performed in layers while preserving 0.5 to 1.5 cm surface layer fat depending on the initial thickness of the fat panniculus to avoid surface irregularities of the treated areas. Patients were always in the supine position with slight elevation of the lower extremities. Liposuction of the flanks was subsequently performed in the decubitus position; this was achieved by flexing the patient's legs and placing the right leg over the left one and turning the torso to the side, easily exposing the posterior region of the flanks and vice versa without the need to change position (Figure 2).

Figure 2 - Decubitus position for performing lateral and posterolateral liposuction
Before starting the surgery, 1 g hydrocortisone was administered intravenously. In addition, 10 mg dexamethasone was administered at the end of surgery. The operating room was maintained at a temperature exceeding 20ºC.
GI diagnosis: excess subcutaneous fat, normal skin, and normal muscles
GI treatment: vibroliposuction of subcutaneous fat (Figure 3A-F)

Figure 3 - A-F - GI patient, pre- and postoperatively
Group II
Group II (GII) patients represented 15% of operated patients. They generally had a depressed suprapubic transverse scar after a previous cesarean Pfannenstiel incision and protrusion of the hypogastrium and pubic region caused by the absence of fascia superficialis suturing21 during surgery involving transverse suprapubic incisions, including abdominoplasty; this results in contraction, depressing the scar and causing the hypogastrium and pubic region to bulge.
Patients exhibited excess subcutaneous fat similar to GI, with slight excess skin in the infraumbilical segment and good tone of the muscle - aponeurotic wall without muscle diastasis. The normal height of the umbilicus position involves infra- and supraumbilical segments in an approximate ratio of 1:1.5 6.
Subcutaneous fat was treated by vibroliposuction in all required segments similar to GI; a transverse subcutaneous fusiform skin section3 was resected up to the muscle aponeurosis in the shape of an indigenous canoe, and variable lateral extension was performed as needed (Figure 4). The vertical extension ran approximately 12 to 14 cm from the edge of the incision to the umbilicus with the skin slightly stretched. The inferior incision was low enough as to avoid cutting the bottom of the lyre following the inguinal folds 1 to 1.5 cm above them without crossing them. The lower demarcation was always made with the skin stretched up toward the umbilicus. The planes were sutured with nonabsorbent sutures, first recomposing the fascia superficialis transversely and then the deep sub-dermis. In the last 116 cases, transparent slow-absorption sutures were used in the intradermal plane, avoiding the elimination of sutures through the skin and visibility of the dark sutures in the subdermal plane.

Figure 4 - GII: fusiform skin resected in the shape of an indigenous canoe
GII diagnosis: excess subcutaneous fat equal to that in GI, slight excess skin in infraumbilical segment, good-quality aponeurotic wall muscle, and normal umbilicus placement
GII treatment: vibroliposuction of subcutaneous fat, and fusiform resection of transverse suprapubic skin (Figure 5A-F)

Figure 5 - A-F - GII patient pre- and postoperatively.
Group III
Group III (GIII) patients represented 5% of all patients. They exhibited changes similar to those of GII with respect to subcutaneous tissue and skin but with more diastasis of the external oblique muscles and normal umbilicus position. The treatment of subcutaneous fat and skin resection were performed in manners similar to those in GI and GII, respectively. The insertions of the external oblique muscle in the lateral portion of the rectus muscles were exposed through 2 lateral tunnels from the iliac crest to the laterocostal margin, allowing them to traction medially, correct the diastasis, and reduce waist circumference such that it was just wide enough to expose the aponeurosis and therefore the diastasis (Fig. 6). This region does not have important perforator vessels supplying the abdominal subcutaneous and skin flap. Therefore, the undermining of the supra-aponeurotic tunnels presents minimal bleeding4,6,22. The diastasis was marked, and its closure began in the laterocostal margin using nonabsorbent anchored continuous suturing ending near the inguinal ligament; the sutures can be enhanced with separate sutures on the continuous one. The flap was subsequently pulled down, fixing the aponeuroses23,24, and the upper edge was sutured to the lower one as described in GII.

Figure 6 - Lateral tunnel exposing the diastasis of the lateral oblique muscle at the insertion with the rectus abdominis.
GIII diagnosis: excess subcutaneous fat equivalent to GI and GII, excess skin equivalent to GII, aponeurotic muscle wall with diastasis of the external oblique muscles, and normal umbilicus height.
GIII treatment: vibroliposuction equivalent to GI and GII, resection of skin and subcutaneous tissue equivalent to GII, and plication of the external oblique muscles through lateral tunnels (Figures 7A-F).

Figure 7 - A-F - GIII patient pre- and postoperatively
Group IV
Group IV (GIV) patients represented 28% of all patients. GIV exhibited subcutaneous fat similar to GI-III, little excess skin in the supra and infraumbilical segments, diastasis of the rectus muscles, and high umbilicus placement (>1:1.4 , sometimes even 1:1.2). Patients were treated with vibroliposuction of subcutaneous fat similar to GI-III. Skin and subcutaneous resection were similar to those in GII and GIII. Diastasis of the rectus muscles was treated by suturing the medial edges of the muscle aponeurosis through a tunnel in the midline from the top edge of the resection zone of the skin to the xiphoid4-6 (Fig. 8). The sutures were anchored continuously and reinforced with separate stitches from the xiphoid to the pubis. To better expose the diastasis and facilitate its treatment, the umbilicus was detached from its aponeurotic implantation and attached to the flap in a form resembling a glove finger. The detached areas on the diastasis did not exhibit major perforating vessels supplying the abdominal flap5,6,22. Two important umbilical vascular pedicles can be preserved during undermining. The abdominal flap was sutured over the corrected aponeurotic wall with a slight pull-down using absorbable sutures23,24. The umbilicus was reimplanted in the aponeurosis with a bolster stitch through its back skin 2 to 4 cm below the original implantation; this consequently pulled the supraumbilical skin segment and altered the ratio between the infra- and supraumbilical segments up to 1:1.6, close to the Φ ratio, making the abdomen more aesethetic6. Thus, the high umbilicus placement becomes normal or low. The rest of the procedure was similar to those for GII and GIII6.
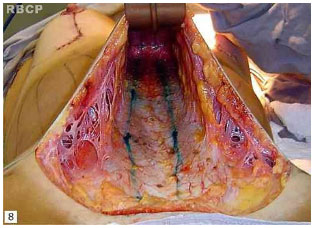
Figure 8 - Central tunnel exposing the diastasis of the rectus abdominis muscle
GIV diagnosis: excess subcutaneous fat equivalent to GI-GIII, slight excess skin in the infra- and supraumbilical segments, musculoaponeurotic wall with diastasis of the rectus abdominis muscles, and high navel placement
GIV treatment: vibroliposuction of affected areas, fusiform skin resection equivalent to GII and GIII, midline tunneling and plication of the rectus abdominis muscles, and reimplantation of the umbilicus below the original point at an infra-/ supraumbilical ratio of up to 1:1.6 (Figures 9 A-F, 10 A-F)

Figure 9 - A-F - GIV patient pre- and postoperatively. Note the lower placement of the umbilicus.

Figure 10 - A-F - An overweight GIV patient
Group V
Group V (GV) represented 7% of all operated cases. This group exhibited excess subcutaneous fat, excess skin in the large supraumbilical segment, diastasis of the rectus muscles and sometimes external oblique muscles, and low-set umbilicus with an infra-/supraumbilical ratio <1:1.6 . The supraumbilical segment was long, and the infraumbilical segment may or may not be flaccid and long. GV was treated with vibroliposuction similar to GI-IV as well as transverse fusiform skin and subcutaneous tissue resection from the pubis to the umbilicus, with the removal of excess skin width as needed. Plication of the rectus muscles via a tunnel similar to GIV from the xiphoid to the pubis was performed. Furthermore, plication of the external oblique muscle through 2 lateral tunnels similar to GIII from the laterocostal margin to the inguinal ligament was performed if necessary. In such cases, there were 3 tunnels in areas without major vascular perforators (Figure 11). Finally, transpositioning of the umbilicus with omphaloplasty (Figure 12A, B), fixing the abdominal flap undermined in tunnels to the aponeurosis, and suturing the fascia superficialis and skin were performed in manners similar to those in GII-IV. This procedure is a classic abdominoplasty associated with vibroliposuction and undermining in tunnels for muscle plication (i.e., lipoabdominoplasty).

Figure 11 - The 3 possible tunnels to avoid compromising the vascularity of the skin and subcutaneous tissue of the abdomen. The entire abdomen becomes an axial flap supplied by perforating vessels of the rectus abdominis and oblique muscles.

Figure 12 - A - Fusiform marking for removal of skin from the pubis to the umbilicus; B - Transposition of the umbili-cus for omphaloplasty.
GV diagnosis: excess subcutaneous fat equivalent to GI-IV, excess skin in the supra- and infraumbilical segments, aponeurosis with diastasis of the rectus abdominis muscles and/or oblique muscles, and low umbilicus placement
GV treatment: vibroliposuction of affected areas, resection of fusiform skin from the pubis to the umbilicus, midline tunneling and plication of the rectus abdominis muscles sometimes with side tunneling and plication of the external oblique muscles, and omphaloplasty at the original position of the umbilicus (Figure 13A-F).

Figure 13 - A-F - GV patient pre- and postoperatively.
RESULTS
The approaches and techniques described herein were based on observations of 614 patients operated on between October 2001 and October 2011. The data presented herein are from the most recent 200 consecutive cases.
Two patients (1%) were treated as in GIV. Results were unsatisfactory because of insufficient skin traction. They underwent further surgery and were classified as GV. The classification was effective for the diagnosis of abdominal cosmetic changes in 99% of cases. There were small touches of "ears" or small bulges that were not considered in the analysis of the effectiveness of the classification; however, 7% of them had to be retouched in some little detail.
GI-V accounted for 75% of cases; the remaining 25% represented sequelae and/or secondary abdominoplasties, usually by excessive removal of skin, 2% of which were performed by the author. There were 2 cases of nosocomial infection, necrosis of the edge of the flap, suture dehiscence, and healing by secondary intention, and reoperation after 6 months.
Regarding the shapes of the abdomen and trunk, good results were obtained with more intense and extensive liposuction. Meanwhile, the suprapubic transverse scar was always placed very low without severing the bottom of the lyre. The scars of patients in GII were always less extensive than those of GIII-V; however, scar quality was similar among all groups: good without enlargement or hypertrophy due to poor traction on the suture line.
DISCUSSION
The data reported herein are from the last 200 consecutive cases operated on in a private clinic. The percentage of patients in each group varied over time, indicating increasing demand for surgery by patients with minor cosmetic changes to improve quality of life. Reasons for this increase include increases in purchasing power in Brazil, body care, and media influence. The reduction of GI was due to improved body care in younger women, including better nutrition and physical activity; this contrasts with other social segments, particularly women with lower income and educational levels. GIV increased markedly in the past 3 years, especially in women who have had 1 or 2 pregnancies; these were generally women who take care of themselves before, during, and after pregnancy; had little excess skin; small or medium diastasis; and cesarean scars, which are highly prevalent in Brazil.
GIV also increased as a result of reductions in GII and GIII. Patients in GIII migrated to GIV, because plication of the rectus muscles in this group was performed to compensate for the plicatures of the oblique muscles; this resulted in the same efficiency, and long-term results were maintained. Meanwhile, GII patients migrated to GIV, because the plication of the rectus muscles even with minor diastasis reduces the waist circumference, improving the proportion to hip circumference. In addition, demand increased as a result of patients with sequelae and poor results. The migration from GV to GIV indicates the tendency of the author to resect less skin.
The steep increase in sequelae treated by the author was due to surgeons in other specialties with less technical training who performed this surgery inappropriately, the availability of the author in the labor market, and ultimately increased demand from patients for near-perfect results.
Except for vibroliposuction, the procedures are similar for all groups when no excess subcutaneous tissue is present. For the proper adjustment of the skin and subcutaneous aponeurosis, the areas are infiltrated and vibroliposuction without suction is performed.
If the transverse scar is high in GV, the bottom of the lyre can be cut; this will make the abdomen unattractive, causing an aesthetic disconnect of the abdomen with the pubis and vulva25. This poor result is common when the abdomen is operated on as per GV, and surplus supraumbilical skin is short and the umbilicus high. To correct this misdiagnosis and treatment, after 6 months, the infraumbilical flap can be detached above the fascia superficialis to the umbilicus and pulled down, resecting the skin below the primary scar and recovering the bottom of the lyre.
The positioning of the umbilicus dividing the abdomen into 2 segments is an important parameter for classifying the abdomen.
When the fascia superficialis is not sutured, it shrinks because it is elastic, causing the hypogastrium and pubic to bulge and depresses the scar. Furthermore, there will be an aesthetic disconnect between the pubis-vulva and abdomen, making the region unaesthetic25. The same occurs with high and wide scars that cut the bottom of the lyre. Sutures must always be made using nonabsorbable threads, reducing the tension of the skin sutures.
All tunnels made to expose the diastasis are made in areas without major vascular perforators; only the edges of the muscles are exposed with their respective aponeuroses. The correction of diastasis of the oblique muscles recomposes the semilunar lines6. In GIII and GIV, 2 umbilical perforators, which are responsible for most of the vascularization of the infraumbilical segment of remaining skin, are always preserved, allowing the infraumbilical segment to undergo greater undermining. Where possible, the preservation of these vessels results in less edema of the detached infraumbilical flap than when they are sectioned; in GV, their preservation is impossible, because they block the sliding of the flap toward the pubis. Fortunately, the infraumbilical portion is removed in this group.
The hypogastrium sometimes remains bulging even with vertical aponeurotic plicatures. Such cases may require transverse plication of an iliac fossa to the other or plication of the oblique muscles from the lower end of the plication to the other contralateral one.
Fixing of the abdominal flap to the aponeurosis in the tunnels23,24 reduces seroma and prevents hematoma; resultant depressions disappear quickly. Compression of the abdomen with a compression garment is initiated immediately after surgery while the patient is still in hypotension 20% below baseline blood pressure. The muscle plication and compression garment increase the venous pressure within the abdominal cavity and lower limbs; to reduce its consequences, the abdominal cavity and lower limbs should be kept elevated throughout the perioperative, and immediate and late postoperative periods until the resumption of normal activities.
The gauze fragment from the bolster stitch that fixes the bottom of the umbilicus to the aponeurosis in GIV should remain in place for 2 weeks; it should be soaked in antibiotic- and corticosteroid-containing ointment.
In cases previously submitted to liposuction, the skin and subcutaneous flap do not slide easily, requiring greater care during the extension of skin resection.
The transverse suprapubic scar should never cross the inguinal folds.
Tractions with exaggerated skin resections do not make the abdomen more attractive, and the scar will be longer and of poorer quality.
When removing skin after liposuction, some surgeons3 leave the fascia superficialis and remainder of the lamellar layer of fat beneath it, pulling and suturing it over itself, thus folding it into 3 layers; the vascular and lymphatic systems are also folded. In the author's experience, the infraumbilical edema is greater in such cases than if all layers down to the aponeurosis are removed. This edema is most severe in GIII and GIV.
Some patients in GII and GIII have an umbilicus with a transverse shape with a very long top fold of skin, giving it a "sad" appearance. There are 3 ways to fix this6: (1) remove a crescent-shaped skin segment approximately 2 cm from its upper half (Figure 14A-C); (2) undermine the infraumbilical flap to the umbilicus, and section the base and re-implant it immediately below, changing its anteroposterior axis by using a bolster stitch; (3) release the umbilicus from the flap as in GV, pull the flap, suture the umbilical wound in layers, and perform omphaloplasty immediately above, resulting in a periumbilical scar and another small vertical scar between the umbilicus and transverse suprapubic scar (Figure 15A, B) or from the umbilicus toward the pubis. In such cases, the cosmetic result is better than "mini T-scars." This approach is also appropriate for abdomens with a flaccid supraumbilical segment and not overly high umbilicus, which would lead to aesthetically inappropriate ratios exceeding 1:1.6 (which is too low) if operated on as GIV. If operated on as GV, there will be excessive skin traction, resulting in a high scar, hypertrophy or enlargement, and an excessively high pubis.

Figure 14 - A - Slight excess supraumbilical skin; B - Removed in a half-moon shape; C - Removal scheme.

Figure 15 - A, B - Abdomen with intermediate vertical scar between the pubis and umbilicus caused by would closure due to its release.
There are also cases classified as GIII with diastasis of the rectus muscles. In such cases, 3 tunnels6 are made; the umbilicus is released from the aponeurosis and re-implanted in its original position. There are also GIV and GV cases with diastasis of the oblique muscles in which 3 tunnels can be made.
Placing the umbilicus at an infra-/supraumbilical ratio less than 1:1.6 makes the abdomen unaesthetic.
In otherwise healthy overweight patients classified in GV who are unwilling to lose weight and usually male, a hygienic surgery can be performed by performing liposuction on the supraumbilical segment, removing the infraumbilical segment of skin and subcutaneous tissue, and transposing the umbilicus without undermining the supraumbilical area through liposuction and redeploying it. In such cases, the umbilicus has a pedicle long enough for this procedure. No plicatures are performed. However, seroma is ever present.
After bariatric surgery and major weight loss, GV patients generally exhibit excess skin in the vertical and horizontal directions, which requires vertical and horizontal resection with anchor-shaped scars sometimes up to the flanks or coccyx without undermining the skin flap with or without liposuction and muscle plications of the rectus abdominis muscles.
CONCLUSION
With the evolution of liposuction, the treatment of aesthetic pathologies of the abdomen has been modified with respect to scope and intensity. However, the classification of different cosmetic alterations in comparison to a model of ideal beauty, i.e., a lyre with depressions and protrusions, has remained unchanged since 1988.
Current approaches are characterized by more extensive liposuction, significant reduction of undermining, and tunneling in areas without major vascular perforators for muscle plication. Finally, less traction and skin resection are performed, and flaps and their respective underlying aponeuroses are fixed, reducing the incidence of seroma.
The classification proposed in 1988 by Bozola and Psillakis1 helps correct different aesthetic pathologies of the abdomen, which require different treatments according to excess fat, skin, diastasis of the rectus abdominis and obliques, and height of umbilicus placement. This classification is effective in 99% of operated cases.
REFERENCES
1. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93.
2. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-7.
3. Avelar J. Fat suction versus abdominoplasty. Aesthetic Plast Surg. 1985;9(4):265-75.
4. Leão C. Curso de Abdominoplastias. Chair man: Bozola AR. XXXVII Congr Bras Cir Plast. Porto Alegre, Brasil: 12 a 15 nov. 2000.
5. Saldanha OR, De Souza Pinto EB, Mattos WN Jr, Pazetti CE, Lopes Bello EM, Rojas Y, et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-7.
6. Bozola AR. Abdominoplasty: same classification and a new treatment concept 20 years later. Aesthetic Plast Surg. 2010;34(2):181-92.
7. Graf R, de Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;30(1):1-8.
8. Bozola AR. Abdominoplastias. In: Mélega JM, Zanini AS, Psillakis JM. Cirurgia Plástica Reparadora e Estética. Rio de Janeiro: Medsi Editora Médica e Cientifica; 1988.
9. Bozola AR. Abdominoplastias. In: Mélega JM, Zanini AS, Psillakis JM. Cirurgia Plástica Reparadora e Estética. Rio de Janeiro: Medsi Editora Médica e Cientifica; 1992.
10. Bozola AR. Abdomen. Classificación y análisis de los tratamientos quirúrgicos em: cirurgia plastica, reconstructiva y estetica. In: Coiffman F (ed.). Cirugía Plástica, Reconstructiva y Estética, 1 ed. Barcelona: Ed. Salvat; 1994. p.3086-95.
11. Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg. 1991 ;15(2):111-21.
12. Pitanguy I, Salgado F, Murakami R, Radwanski HN, Mauad Junior R. Abdominoplastia: classificação e técnicas cirúrgicas. Rev Bras Cir. 1995;85(1):23-44.
13. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg. 2001;108(6):1787-95.
14. Livio M. La proporción áurea, la historia de PHI, el numetro más sorprendente del mundo. Barcelona: Editorial Ariel; 2005.
15. Eco H. Storia della bellezza. Milano: Bompiani; 2004.
16. Atalay B. A Matemática e a Monalisa - A confluência da arte com a ciência. São Paulo: Mercurio; 2007.
17. Etcoff NL. Psychology. Beauty and the beholder. Nature. 1994;368(6468):186-7.
18. Marquardt SR. Marquardt beauty analysis [Accessed 2010 Mar 15th]. Available at: http://www.beautyanalysis.com/
19. Preston JD. The golden proportion revisited. J Esthet Dent. 1993;5(6):247-51.
20. Ricketts RM. The biologic significance of the divine proportion and Fibonacci series. Am J Orthod. 1982;81(5):351-70.
21. Sterzi G. "La Fascia Superficialis" in II Tessuto Sottocutaneo. Firenze: Luigi Nicolai Tipografo Editora; 1910.
22. Tregaskiss AP, Goodwin AN, Acland RD. The cutaneous arteries of the anterior abdominal wall: a three-dimensional study. Plast Reconstr Surg. 2007;120(2):442-50.
23. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
24. Pollock H, Pollock T. Progressive tension sutures: a technique to reduce local complications in abdominoplasty. Plast Reconstr Surg. 2000;105(7):2583-6.
25. Bernabei J. Importância da área pubiana na abdominoplastia. Mesa Redonda 12, 13 novembro - 12/13 horas 48º Congresso Brasileiro de Cirurgia Plástica, Goiânia 11/15 novembro; 2011.
PhD, Professor of Plastic Surgery. Head of the Plastic Surgery Service of the Hospital de Base, São José do Rio Preto, SP, Brazil
Antonio Roberto Bozola
Av. Brig. Faria Lima, 5416
CEP: 15090-000. São José do Rio Preto, SP, Brasil
Article received: 10/08/2013
Article accept: 01/09/2013
Work performed at the Faculty of Medicine of São José do Rio Preto - Famerp. São José do Rio Preto, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter