

Original Article - Year 2013 - Volume 28 -
Evaluation of cutaneous sensitivity in patients with acute injuries of the upper limb peripheral nerves
Avaliação da sensibilidade cutânea em pacientes com lesões agudas de nervos periféricos em membros superiores
ABSTRACT
BACKGROUND: Peripheral nerve injury in the upper limbs has serious functional and social repercussions. The aim of this study was to describe the use of the Pressure-specified Sensory Device (PSSD) to measure recovery of cutaneous sensitivity in patients who undergo microsurgery reconstruction for traumatic injury of upper limb peripheral nerves.
METHOD: The study included 25 patients with acute injury on the upper limb peripheral (ulnar and/or median) nerves in which the PSSD was used to measure sensitivity. Patients were divided into three groups according to injury location: group 1, forearm; group 2, wrist; and group 3, fingers. Analysis of variance with repeated measurements was used for comparisons.
RESULTS: Interaction effects showed statistical differences (P < 0.05) in the considered parameters as the time of assessment increased.
CONCLUSIONS: The PSSD was an adequate method for determining cutaneous pressure thresholds in the ulnar and median muscles in patients presenting with acute nerves injuries in the forearm, wrist, and fingers and showed a progressive improvement in pressure thresholds over time.
Keywords: Median nerve. Ulnar nerve. Peripheral nerve injuries. Skin. Diagnosis. Prognosis.
RESUMO
INTRODUÇÃO: A injúria de nervos periféricos em membros superiores é uma condição com repercussões funcionais e sociais graves. O objetivo deste estudo é descrever a utilização do Pressure Specified Sensory Device (PSSD) como método de mensuração da recuperação da sensibilidade cutânea em pacientes com reconstruções microcirúrgicas de lesões traumáticas de nervos periféricos em membros superiores.
MÉTODO: O estudo incluiu 25 pacientes com diagnóstico de lesões agudas de nervos periféricos em membros superiores (nervos mediano e/ou ulnar), nos quais o PSSD foi utilizado para mensuração de sensibilidade. Os pacientes foram divididos em três grupos, de acordo com a localização da lesão: grupo 1, antebraço; grupo 2, punho; e grupo 3, dedos. O teste estatístico utilizado para análise das comparações foi a Análise de Variância (ANOVA) com Medidas Repetidas.
RESULTADOS: Foram encontrados efeitos de interação com diferença estatística (P < 0,05) para os parâmetros considerados à medida que se aumenta o tempo de avaliação.
CONCLUSÕES: O PSSD se mostrou um método capaz de determinar os limiares cutâneos de pressão nos territórios dos nervos mediano e ulnar nos pacientes com lesões agudas desses nervos em antebraço, punho e dígitos, demonstrando que houve melhora progressiva dos limiares de pressão ao longo do tempo.
Palavras-chave: Nervo mediano. Nervo ulnar. Traumatismos dos nervos periféricos. Pele. Diagnóstico. Prognóstico.
Tactile information is decoded through mechanoreceptors with specialized endings involving the terminal sensitive nerve. Histological and physiological studies have identified four types of mechanoreceptors in hairless skin1:
Tactile stimulation is decoded by electrical impulses through different morphologies of terminal receptors described above and ascends via peripheral nerve axons of the dorsal root ganglia through nervous fibers of various diameters2.Meissner corpuscles: fast adaptation receptors found at the margins of the papillary sulcus that are responsible for fine mechanical sensitivity and comprise fluid-filled globular structures with epithelial cells that involve the terminal nerve; Merkel disks: slow adaptation receptors found at the center of the papillary sulcus with a semi-rigid structure that transmits the skin pressure to the nerve endings; Paccini corpuscles: physiologically similar to Meissner corpuscles but less numerous, respond to fast deformation of the skin but not at the sustained pressure, deeply positioned at the subcutaneous tissue, and have a flexible capsule that is sensitive to the vibratory stimulation (200-300 Hz) of the skin; Ruffini endings: slow adaptation receptors concentrated at the subcutaneous tissue of the skin sulcus in the articulations in the palm of the hand and in the nails and capture skin stretching or nail curvature and transmit information to the nerve endings, the decoded information from which contributes to the perception of object forms.
Normal hand sensitivity is extremely important for hand function, and several tests have been used to evaluate it. These tests were introduced in the clinical practice by Weber in 1835 (the two-point discrimination) and Von Frey in 1905; both tests evaluate traumatic injuries of the upper limb nerves3.
To monitor progressive neural regeneration, it is important to quantitatively measure sensitivity and motor ability in order to evaluate surgical and rehabilitation results, particularly those involving upper limb injuries4.
Cutaneous sensitivity tests may help monitor neural regeneration; however, these tests have drawbacks including that they cannot be generalized and lack precision and standardization; further, no consensus has been reached relevant information such as sensitivity modalities4. According to Dellon5, there has been a gradual improvement in the instrumentation and progress in the qualitative to quantitative aspects of measuring this modality.
The two-point discrimination test described by Weber essentially determines the minimum distance at which a patient can discriminate feeling contact between two points4.
In 1992, Dellon5 introduced a computerized test for evaluating cutaneous sensitivity in clinical practice: the Pressure-specified Sensory Device (PSSD), which measures cutaneous pressure thresholds. This instrument allows the determination of pressure perception parameters that were not previously available.
The PSSD was introduced in the Hospital das Clinicas at the Faculty of Medicine, University of São Paulo in 1998 and has been used to evaluate cutaneous sensitivity in different conditions after plastic surgery and in neuropathies of the lower limbs in diabetic patients6,7.
This study aimed to use the PSSD to determine cutaneous pressure thresholds in the ulnar and median nerves in patients with acute injuries of these nerves in the forearm, wrist, and fingers and to compare the results with those at different injury locations.
METHOD
Patients with a diagnosis of acute injury in the upper limb peripheral nerves submitted a standard questionnaire containing data regarding history and physical examination, which was administered by the same professional. The intraoperative diagnosis of the injuries of the ulnar and/or median nerves was used to include patients in the protocol.
Patients were divided into three groups: group 1, patients with injuries to the ulnar and/or median nerves in the forearm; group 2, patients with injuries to the ulnar and/or median nerves in the wrist; and group 3, patients with injuries to the ulnar and/or median nerves in the fingers.
Patients with the following characteristics were excluded from this study: systemic neurological disorders, peripheral polyneuropathies, previous surgeries on peripheral nerves, a previous history of upper motor neuron injury, comprehension or cooperation deficits during testing, or an inability to perform motor functions required for the test.
A total of 25 patients with acute injury of peripheral nerves were included in this study. Average patient ages were as follows: group 1, 35.7 years (standard deviation [SD], 7.09); group 2, 31.2 years (SD, 5.31); and group 3, 38.0 years (SD, 7.15). Group 1 included 11 hands of 11 patients; group 2, seven hands of seven patients; and group 3, seven hands of seven patients.
All patients underwent surgery. The diagnosis of injury was confirmed intraoperatively under general anesthesia or blockage by the medical team attending training in the same institution. Standardized microsurgical techniques were used. Surgical repair comprised neurorrhaphy with the epineural technique using nylon 9.0 or 10.0 sutures and a surgical microscope that was distributed circumferentially to the affected nerve using standardized incisions and approaches.
In the postoperative period, all complications were registered, including bleeding, infections, scar alterations, neuroma formation, or hypersensitivity in the area of the repaired nerve. The occupational therapy team monitored the patients' hand function progress.
Sensitivity tests were conducted using the PSSD, which is equipped with two parallel metal ends with blunt edges (Figure 1), the distance between which may be adjusted by the evaluator (from 2.5 to 20 mm). These ends are connected to pressure transducers that allow us to verify the strength applied to the skin for one- or two-point pressure measurements. The PSSD was plugged into a computer so that data could be visualized on the screen as well as used for data analysis and storage (Figure 2).

Figure 1 - A Pressure-specified Sensory Device, as a pressure transducer: adjustments in the distance (in millimeters) between two points.

Figure 2 - Overall view of the computer to which the Pressure-specified Sensory Device is connected.
The test was performed in a calm environment free of distractions. During the test, the patient was seated in front of the evaluator with the hand examined while comfortably at rest on the table. The patient was not able to see the computer screen. Prior to initiating the test, the evaluator explained how the exam would be performed and that it would not cause damage or pain. The chosen and standardized test regions were the digital pulp of the index finger for the median nerve and the digital pulp of the little finger for the ulnar nerve.
The instrument should be calibrated for gravity at the beginning of each test. The evaluator continuously increased pressure from the metal end over the digital pulp. When the stimulus was perceived by the patient, he or she pressed a button connected to a warning sound (Figure 3), and that value was stored in the computer. Ten attempts were made, among which the three most adequate were selected by the computer. The arithmetical mean of the three measures was calculated and accepted as the result.

Figure 3 - Sound activated by the patient during cutaneous pressure threshold measurements.
Measurements were registered for the static test, static one-point discrimination (s1PD), in which the evaluator applies continuously increasing pressure without moving the instrument in order to measure the function of slow adaptation fibers of superficial sensation. Next, the evaluator performed a gradual pressure movement to measure the function of fast adaptation fibers by using one of the instrument ends in movement. The moving one-point discrimination (m1PD) test was registered. Subsequently, the two-point cutaneous pressure thresholds were tested: the static test, for static two-point discrimination (s2PD), and the moving test, for moving two-point discrimination (m2PD). The evaluator took care to avoid touching the end of the instrument or applying more pressure in one of the two ends of the instrument, which would help the patient feel the two ends. The same way, the two ends were maintained in the position or movement to measure the function of the slow or fast adaptation fibers, respectively. When testing the two points, the evaluator emphasized to the patient that the button should only be pressed when the two separate point sensation occurred in the digital pulp and not when the patient feels the pressure stimulus. The total test duration was approximately 40 minutes.
We were interested in comparing the average results obtained in the groups (called the group effect) and simultaneously between four points of the assessment over time, with measurements performed at 1, 3, 6, and 12 months after surgical nerve repair (time effect). Repeated-measures analysis of variance was used to compare variables between the groups and moments.
Due to the interaction effect observed, we identified differences in injuries evaluated at 1, 3, 6, and 12 months and points at which injuries differed, depending on the location of the injury: the forearm, wrist, and fingers. For that purpose, multiple comparisons (two-by-two comparisons) were performed using the Bonferroni test.
RESULTS
Variable of interest: s1PD
According to the data mentioned above and shown in Table 1, we observed interaction effects. Multiple comparisons were performed to identify which groups had significant differences. Multiple comparison revealed a difference only between the fingers and remaining groups (P < 0.05) at all time points, except for the 12-month evaluation. This result showed that the s1PD value was lower in the finger injury group than in the remaining groups. All of the groups showed significant differences at the 12-month evaluation, showing that fingers injuries had a lower s1PD value, followed by wrist and forearm injuries, which had higher values. Multiple comparisons performed among injury locations revealed a difference at all time points (P < 0.05), showing that the s1PD value tended to decrease as evaluation time increased. This phenomenon was observed for all injury types (Figure 4).
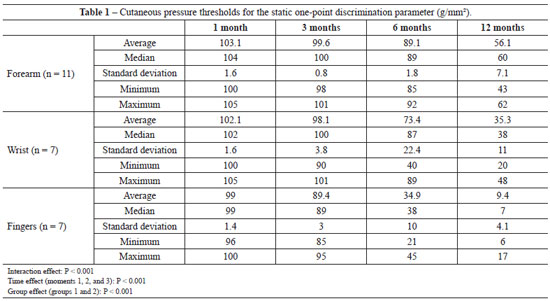
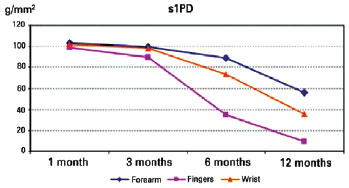
Figure 4 - Multiple comparisons of the static one-point discrimination (s1PD) parameter at locations of nerve injuries at three time points.
Variable of interest: s2PD
According to data mentioned previously and shown in Table 2, we observed interaction effects. Multiple comparisons were performed to identify groups that showed significant differences. Differences were observed only between the finger and the other groups (P < 0.05) at months 1 and 6, showing that the s2PD value is higher in the finger injury group than the remaining groups. No differences in interactions effects were observed between the groups (P > 0.05) at the 3-month follow-up. All groups showed significant differences in interactions effects at the 12-month follow-up, and the finger injury showed a lower s2PD value, followed by the wrist and forearm, which had higher values (Figure 5). Multiple comparisons of months for each injury showed differences in finger and wrist injuries for all time points, except in the 1-month follow-up, which did not differ from the 3-month result (P < 0.05), indicating that the s2PD value decreased as evaluation time increased. With regard to the forearm, the 1-month measurement did not differ from the 3-month measurement, which was not different from the 6-month measurement. In the remaining situations, differences were observed between months, and the s2PD value decreased as the evaluation time increased.
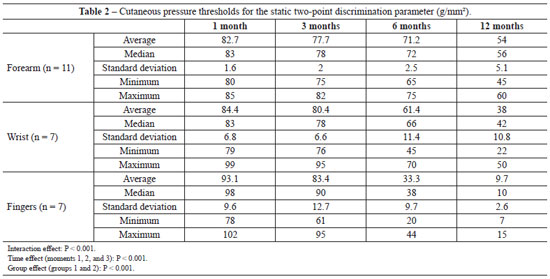
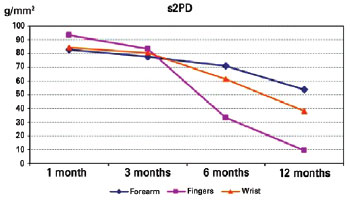
Figure 5 - Multiple comparisons of the static two-point discrimination (s2PD) parameter at locations of nerve injuries at 3 time points.
Variable of interest: m1PD
According to the data mentioned previously and shown in Table 3, we observed the interaction effect. Multiple comparisons were performed to identify which groups showed statistically significant differences. Multiple comparison showed no statistically significant differences in interaction effect among injuries (P > 0.05) at the 1-month time point. Differences in interaction effects were seen only between the finger group and the remaining groups (P < 0.05) in the 6-month measurement, indicating that the m1PD value was higher in the finger injury group than in the remaining groups. The values among the groups were statistically significant at the 6- and 12-month time points (P < 0.05), indicating that the finger injury had a lower m1PD value, followed by the wrist and forearm, which had higher values (Figure 6). Multiple comparisons performed by injury revealed differences between all time points for the forearm and wrist, except at 1 month, which was not significantly different from the result obtained at 3 months (P < 0.05), indicating that the m1PD value decreased as the evaluation time increased. With regard to the finger injury group, multiple comparisons revealed differences for all time points (P < 0.05), indicating that the m1PD value decreased as the evaluation time increased.
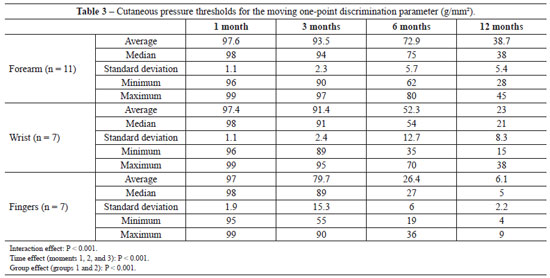
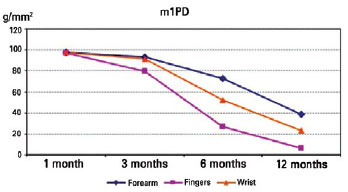
Figure 6 - Multiple comparisons of the moving one-point discrimination (m1PD) parameter at locations of nerve injuries at 3 time points.
Variable of interest: m2PD
According to the data mentioned previously and shown in Table 4, we observed the interaction effect. Multiple comparisons were performed to identify which groups had statistically significant differences. Multiple comparisons revealed no statistically significant differences in interaction effects between injuries (P > 0.05) in month 1, except between the forearm and finger groups, indicating that the m2PD value was higher in finger injury than in forearm injury. There was no statistically significant difference between groups (P > 0.05) in interaction effect at 3 months. At 6 months, a difference in interaction effect was seen between the finger group and the remaining groups (P < 0.05), indicating that the m2PD value was higher in finger injury than in the remaining groups. At 12 month, values among all groups were statistically significant (P < 0.05), indicating that finger injury had a lower m2PD value, followed by wrist and forearm injuries, which had higher values (Figure 7). Multiple comparisons of the months by injury revealed differences among all time points for the forearm and wrist, except for month 1, which was not significantly different from that at 3 and 6 months, which was not significantly different from that at 12 months (P < 0.05). This showed that for the remaining time points, the m2PD value decreased as the evaluation time increased. With regard to finger injury, multiple comparisons of the months revealed significant differences among all time points, except those at 6 months, which were not significantly different from those at 12 months (P < 0.05), indicating that the m2PD value decreased as the evaluation time increased.
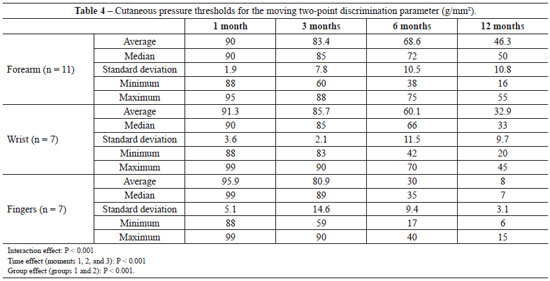
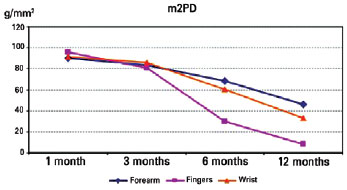
Figure 7 - Multiple comparisons of the moving two-point discrimination (m2PD) parameter at locations of nerve injury at three time points.
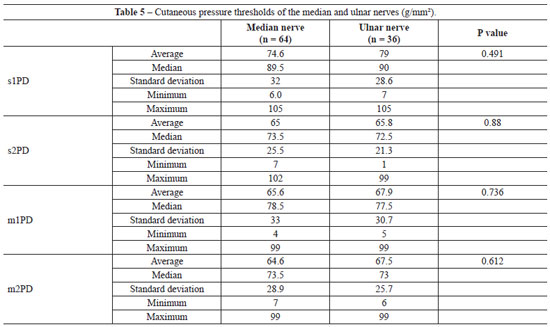
Comparison of points (s1PD, s2PD, m1PD, and m2PD) between median and ulnar nerves
To compare the quantitative variables between the two groups of interest (median and ulnar), Student's t-test was used with a 5% significance level. Considering the results shown in Table 5, we observed that there were no statistically significant differences between the groups for any of the variables (P > 0.05).
DISCUSSION
Few studies in Brazil have reported the use of PSSD as an instrument to help the diagnosis or monitoring of conditions; thus, our study is an important reference in the evaluation of cutaneous sensitivity in patients after acute trauma to the upper-limb peripheral nerves.
Two types of quantitative tests assess cutaneous sensitivity: the cutaneous pressure threshold test and the two-point discrimination test. Moberg8 disseminated the importance of the two-point discrimination as a measure related to hand function, which was subsequently confirmed by various authors9. A correlation was seen between two-point discrimination and fiber density in a given region, i.e., the higher the fiber density, the lower is the distance identified as two separate points10.
Nevertheless, controlling pressure during test is difficult, leading to difficulty in comparing data among institutions, patients, and often even among different evaluations in the same patient11.
The Semmes-Weinstein is the most well-known cutaneous pressure threshold test. This test allows estimation of the interval of perception of cutaneous pressure thresholds in patients. The inability to provide continuous results, a limitation of this test, is a drawback inherent to the test that may for example, not detect an alteration in cutaneous sensitivity when it remains within the same interval obtained previously12.
Levin et al.13 evaluated the calibration and mechanical properties of Semmes-Weinstein monofilaments and calculated deformation stress and material strength. They concluded that mistakes in technique use and interpretation may lead to great variability, influencing the results13.
Dellon et al.12 referred to PSSD as a way to relate the concepts of cutaneous pressure threshold and two-point discrimination. Each of these parameters evaluates different aspects of the peripheral nerve with unique advantages, such as the continuous measurement of the cutaneous pressure threshold (in a different way from the Semmes-Weinstein test, which, as previously mentioned, measures value intervals) and the possibility of controlling pressure in the skin by the instrument, as used in the two-point discrimination test, thus adding precision. It is possible to measure not only the distance between two points but also the lower pressure in which there is perception of cutaneous stimulus between two points.
The cutaneous pressure thresholds for the m1PD parameter measured by the PSSD at the end of the 12-month evaluation tended to be lower, mainly in the group of patients with finger injuries, followed by patients with wrist and forearm injuries. There was a decrease in cutaneous sensitivity values as the time of surgical repair of the nerve increased, except after 1 month, which was not significantly different from that of 3 month (P > 0.05), and evidence suggested recovery of fibers that are responsible for the perception of movement and vibration. Paccini and Meissner corpuscles are responsible since they are associated with those fibers in hairless skin.
A progressively decreasing pattern was also observed in the cutaneous pressure thresholds registered by the PSSD for the s1PD, s2PD, and m2PD parameters in patients with finger injuries, followed by those with wrist and forearm injuries. In the majority of the groups under consideration, no statistically significant differences were seen between the 1- and 3-month evaluation results. However, there was a statistically significant progression in cutaneous pressure thresholds over time.
The group of patients with finger nerve injuries had lower cutaneous pressure thresholds than those in the remaining groups, since the progression of regeneration throughout the distal segment of the repaired nerve, at an expected rate of 1-4 mm/day,14,15 would reach the mechanoreceptors, which are responsible for capturing tactile stimulus, primarily in the finger nerves compared to the remaining groups with upper limb injuries.
The majority of cutaneous pressure threshold results of the s1PD, m1PD, s2PD, and m2PD parameters between 1 and 3 months did not demonstrate statistically significant differences.
A progressive improvement was seen in all of the evaluated parameters over time, i.e., lower cutaneous pressure thresholds were determined using the PSSD instrument.
CONCLUSIONS
The PSSD proved to be a method capable of determining cutaneous pressure thresholds in the median and ulnar nerves of patients with acute injuries in these nerves in the forearm, wrist, and fingers and showed progressive improvement in pressure thresholds over time.
REFERENCES
1. Vallbo AB, Johansson RS. The tactile sensory innervations of the glabrous skin of the human hand. In: Gordon G, ed. Active touch. New York: Pergamon; 1978. p. 29-54.
2. Burgess PR, Wei JY, Clark FJ, Simon J. Signaling of kinesthetic information by peripheral sensory receptors. Annu Rev Neurosci. 1982;5:171-87.
3. Hentz VR, Lalonde DH. Self-assessment and performance in practice: the carpal tunnel. Plast Reconstr Surg. 2008;121(4 Suppl):1-10.
4. Dellon AL. Evaluation of sensibility and re-education of sensation in the hand. Baltimore: Williams and Wilkins;1981.
5. Dellon AL. Specific applications & normative data-upper extremity. In: Somatosensory testing and rehabilitation. Bethesda: The American Occupational Therapy Association; 1997. p. 299-343:
6. Ferreira MC, Costa MP, Cunha MS, Sakae E, Fels KW. Sensibility of the breast after reduction mammaplasty. Ann Plast Surg. 2003;51(1):1-5.
7. Ferreira MC, Rodrigues L, Fels K. New method for evaluation of cutaneous sensibility in diabetic feet: preliminary report. Rev Hosp Clin Fac Med São Paulo. 2004;59(5):286-90.
8. Moberg E. Aspects of sensation in reconstructive surgery of the upper extremity. J Bone Joint Surg Am. 1964;46:817-25.
9. Dellon AL. The moving two-point discrimination test: clinical evaluation of the quickly adapting fiber/receptor system. J Hand Surg Am. 1978;3(5):474-81.
10. Novak CB, Mackinnon SE, Kelly L. Correlation of two-point discrimination and hand function following median nerve injury. Ann Plast Surg. 1993;31(6):495-8.
11. Bell-Krotoski JA, Buford WL Jr. The force/time relationship of clinically used sensory testing instruments. J Hand Ther. 1997;10(4):297-309.
12. Dellon AL, Mackinnon SE, Brandt KE. The markings of the Semmes-Weinstein nylon monofilaments. J Hand Surg Am. 1993;18(4):756-7.
13. Levin S, Pearsall G, Ruderman RJ. Von Frey's method of measuring pressure sensibility in the hand: an engineering analysis of the Weinstein-Semmes pressure aesthesiometer. J Hand Surg Am. 1978;3(3):211-6.
14. Mackinnon SE, Dellon AL. Nerve repair and nerve grafts. In: Mackinnon SE, Dellon AL, eds. Surgery of the peripheral nerve. New York: Thieme Medical Publishers; 1988. p. 89-129.
15. Mackinnon SE. New directions in peripheral nerve surgery. Ann Plast Surg. 1989;22(3):257-73.
1. MSc in Plastic Surgery, full member of the Brazilian Society of Plastic Surgery, plastic surgeon at the Hospital Sírio-Libanês, São Paulo, SP, Brazil
2. Full professor of the Module in Plastic Surgery, Faculty of Medicine/University of São Paulo (FMUSP), São Paulo, SP, Brazil
3. Assistant physician of the Module in Plastic Surgery, FMUSP, São Paulo, SP, Brazil
4. Assistant physician of the Module in Plastic Surgery, FMUSP, São Paulo, SP, Brazil
Correspondence to:
Nelio Watanabe Aguilera
Rua Barata Ribeiro, 490 - cj. 105 - Bela Vista
São Paulo, SP, Brazil - CEP 01308-010
E-mail: nwaguilera@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 25, 2012
Article accepted: December 15, 2013
Work performed at the Hospital das Clinicas of the Faculty of Medicine, University of São Paulo, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter