

Original Article - Year 2013 - Volume 28 -
Abdominoplasty following massive weight loss: a critical analysis of complications in 130 consecutive cases
Abdominoplastia após grandes perdas ponderais: análise crítica de complicações em 130 casos consecutivos
ABSTRACT
BACKGROUND: The massive weight losses caused by bariatric surgery have considerably increased the demand for plastic surgery, with abdominoplasty being the most requested procedure. In this study, an analysis of post-abdominoplasty complications was conducted in a consecutive series of 130 patients who experienced massive weight loss.
METHODS: One hundred and thirty patients who underwent abdominoplasty were studied, and the differences between the genders, surgery types (anchor-line vs. conventional), drain usage, adhesive sutures, and lost weight during the weight loss phase and at the time of abdominoplasty as well as the occurrence of complications such as seroma, hematoma, and infection were analyzed.
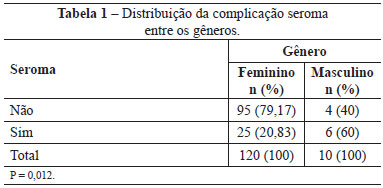
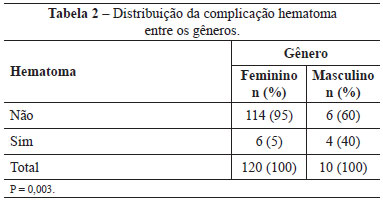
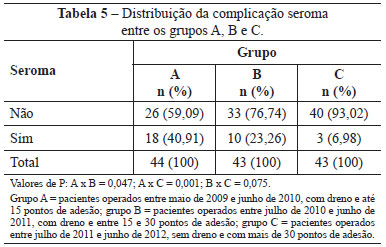
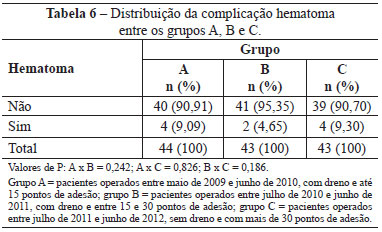
RESULTS: Ten men and 120 women underwent surgery (mean age, 38.3 years). The anchor-line abdominoplasty and conventional techniques were performed in 99 and 31 patients, respectively. Seroma was the most prevalent complication in men (P = 0.012) and was more frequent in group A and B patients (with drains and fewer than 30 adhesive sutures, respectively) relative to group C patients (without drains and more than 30 adhesive sutures), with respective P values of 0.001 and 0.075, and in patients who underwent abdominoplasty and weighed more than 70 kg (P = 0.002). Hematoma was more prevalent in men (P = 0.003) and in patients who underwent abdominoplasty and weighed more than 70 kg (P = 0.008). There were no significant differences with respect to the infection incidence between the tested groups or between the anchor-line and conventional abdominoplasty procedures.
CONCLUSIONS: Seroma was the main complication and could be avoided by using an appropriate number of adhesive sutures. Male patients weighting more than 70 kg at the time of abdominoplasty developed more complications.
Keywords: Bariatric surgery. Obesity. Abdominoplasty.
RESUMO
INTRODUÇÃO: As grandes perdas ponderais causadas pelas cirurgias bariátricas vêm aumentando consideravelmente a demanda por cirurgias plásticas, sendo a abdominoplastia o procedimento mais requisitado. Neste estudo é feita uma análise das complicações posteriores à abdominoplastia em pacientes após grandes perdas ponderais numa série consecutiva de 130 casos.
MÉTODO: Foram estudados 130 pacientes submetidos a abdominoplastia, analisando-se diferenças entre gêneros, tipos de cirurgia (em âncora vs. convencional), utilização de drenos, pontos de adesão, peso perdido no emagrecimento e na abdominoplastia, além de complicações ocorridas, como seroma, hematoma e infecções.
RESULTADOS: Foram operados 10 homens e 120 mulheres (média de idade de 38,3 anos). A técnica de abdominoplastia em âncora foi realizada em 99 pacientes e convencional, em 31 pacientes. Seroma foi a complicação mais prevalente no gênero masculino (P = 0,012), nos pacientes dos grupos A e B (com dreno e menos de 30 pontos de adesão) em relação aos do grupo C (sem dreno e mais de 30 pontos de adesão), com valores de P = 0,001 e 0,075, respectivamente, e nos pacientes que realizaram abdominoplastia pesando mais de 70 kg (P = 0,002). Hematoma foi mais prevalente nos homens (P = 0,003) e nos pacientes que realizaram abdominoplastia pesando mais de 70 kg (P = 0,008). Não houve diferenças significativas quanto a infecção entre os grupos testados nem entre as abdominoplastias em âncora ou convencional.
CONCLUSÕES: O seroma foi a principal complicação, podendo ser evitado com uma quantidade adequada de pontos de adesão. Gênero masculino e pacientes pesando mais de 70 kg no momento da abdominoplastia tiveram mais complicações.
Palavras-chave: Cirurgia bariátrica. Obesidade. Abdominoplastia.
In Brazil, there are currently 30 million obese individuals, of whom 10% are considered morbidly obese. Obesity can now be considered an endemic disease that leads to the development of comorbidities such as hypertension and diabetes, thus rendering the fight against obesity a matter of public health1.
In most cases involving surgical treatment for obesity, treatment is performed via the Fobi-Capella procedure, which has become routine and effective because of its combined weight loss activities (disabsorptive and restrictive)2,3. In the last 7 years, there was an estimated 275% increase in bariatric surgery procedures; additionally, 60 thousand such procedures were performed in the year 2010 alone, of which 35% were performed via videolaparoscopy to further reduce the morbidity associated with this procedure1.
Massive weight losses in patients who have undergone bariatric surgery have generated a wide range of body contouring issues resulting from extensive excess skin. These issues have driven the considerable demand of patients for plastic surgeries to correct those deformities. Abdominoplasty is the most requested procedure by such patients because of the emotional, functional, and aesthetic damage caused by abdominal panniculi4.
In the literature, abdominoplasty for patients who have experienced massive weight loss has been the central subject of many publications along with demonstrations of the techniques and strategies involved in the proper treatment of such patients. As a result, larger numbers of complications have been identified in patients who have undergone abdominoplasty following massive weight loss relative to conventional patients who have undergone similar procedures5.
The purpose of this study was to conduct a critical analysis of the post-abdominoplasty complications, particularly those related to seroma, hematoma, and infection, in a consecutive series of 130 patients who had experienced massive weight loss.
METHODS
One hundred and thirty patients who underwent surgeries performed by the same surgeon (the author) between May 2009 and June 2012 at Vitória Hospital (Curitiba, PR) were analyzed prospectively. All patients were enrolled in the Amil-Paraná Bariatric Surgery Protocol.
The basic inclusion criteria for abdominoplasty were the maintenance of a stable weight for at least 6 months after the weight loss phase and surgical-anesthetic release following preoperative testing.
The preoperative assessment included consultations and release by a nutritionist, psychologist, endocrinologist, and bariatric surgeon. All patients were subjected to blood testing (complete blood count, blood clotting, creatinine, albumin, and glycemia), chest X-rays, electrocardiography, and a pre-anesthetic assessment. Whenever necessary, supplementary tests and cardiology assessments were performed. Smoking patients were instructed to quit smoking at least 30 days prior to surgery. All patients read and signed the free and informed consent form regarding the risks inherent to the surgical and anesthetic procedures.
The performed abdominoplasty procedures were divided into 2 techniques: anchor-line abdominoplasty and conventional abdominoplasty. Anchor-line abdominoplasty with a belt-lipectomy-type posterior extension was performed in only 1 case6.
In most cases, epidural anesthesia with sedation was the anesthetic method of choice. General anesthesia was used in situations wherein contraindications or technical difficulties with spinal anesthesia existed, as well as in some associated surgery cases. The patients received a prophylactic antibiotic upon anesthesia induction (cefazolin, 1 g).
Anchor-line abdominoplasty was indicated for all patients in whom bariatric surgery was performed via laparotomy with a midline supraumbilical longitudinal incision and in 3 other cases according to the patients' preference for this technique as a result of the amounts of striae and extensive excess vertical skin on the epigastric region. The marking for this procedure is shown in Figure 1.
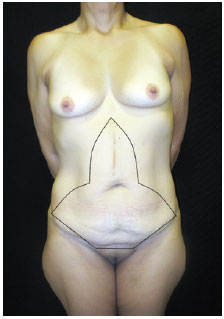
Figure 1 - Anchor-line abdominoplasty markings.
A 1:250,000 adrenaline solution was infused superficially into the markings and the navel. Dermolipectomy was performed as a monoblock via incision of the skin with a cold scalpel and of the fat and aponeurotic detachment with an electric scalpel to preserve the navel and its insertion. Patients with larger caliber vessels (e.g., superficial epigastric, superficial iliac circumflex, and periumbilical perforating arteries and veins) were subjected to ligature with 3-0 cotton thread; the remainder of the homeostatic procedure was performed with electrocoagulation. Possible abdominal wall hernias were dissected via an invagination of the hernial sac and plication of the rectus abdominis muscle in 2 layers with a 2-0 nylon thread (split in an "x" with anchored continuous running sutures). No reinforcement screens were used, and those already present from previous herniorrhaphy procedures were retained. The navel was fixed to the abdominal wall using 3-0 nylon sutures at a height corresponding to half of the height of the abdominal dermofat flap in the mesogastric region. Following fixation, the cutaneous edges of the navel were sectioned in a triangular shape with a superior base.
This study was divided into 3 phases according to the adhesive sutures and vacuum drain usage: the first phase or group A comprised patients who underwent surgery between May 2009 and June 2010; vacuum drains were used in all of these cases and only a few adhesive sutures were applied (≤ 15 sutures). The second phase or group B comprised patients who underwent surgery between July 2010 and June 2011; vacuum drains were used in all of these cases and more adhesive sutures were applied relative to group A (15-30 sutures). The third phase or group C comprised patients who underwent surgery between July 2011 and June 2012; no drains were used on these patients and > 30 adhesive sutures were applied. A 3-0 nylon thread was used for the adhesive sutures. The double-stem vacuum drains were externalized via contraincision in the pubic region and fixed to the skin with a 3-0 nylon thread.
Flap sealing was performed in layers to remove dead spaces. Specifically, 3-0 Polyglecaprone threads (Monocryl®) were used for fat sealing and deep subdermal sutures. A 4-0 thread of the same material was used for superficial subdermal and intradermal sutures. Simple 5-0 nylon sutures were applied on the inverted T region and the navel.
During vertical segment sealing, a space with an approximately 3-cm projection from the navel was left without sutures; in this space, a z-plasty was prepared via flap transposition. A triangular-shaped resection of a single z-plasty flap was then performed, leaving an orifice with the same shape and a superior base for sealing the previously prepared navel according to a similar plan (Figure 2).
Finally, a dressing comprising micropore, gauze, and cotton fillings was applied, followed by the immediate placement of a velcro-sealed compression elastic band on the abdomen.
Conventional abdominoplasty procedures were indicated for patients who had undergone videolaparoscopic bariatric surgery and had been advised regarding possible excess vertical abdominal skin. The markings for this procedure can be observed in Figure 3.
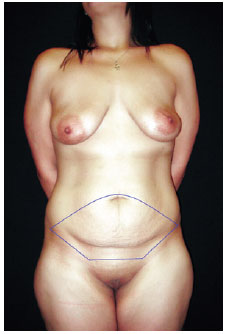
Figure 3 - Conventional abdominoplasty markings.
The procedures performed during conventional abdominoplasties (Callia-Pintaguy-Regnault)7 were similar to those performed during anchor-line abdominoplasties. The only exception was the externalization of the navel, which was performed in that region by making a Y-shaped skin incision on the partially defatted abdominal flap and fixing the ends of this incision with more superficial adhesive sutures, thus allowing the flap to move deeper into the umbilical insertion.
On the night after surgery, all patients stayed in the hospital and remained in the Fowler position with permanent bladder catheters until the following morning, were instructed to flex and extend their feet repeatedly while in bed, and were assisted to rise out of bed and walk on the following morning. Analgesics, symptomatic drugs, prophylactic antibiotics, and low-molecular-weight heparin were prescribed to all patients both during the hospital stay and after discharge.
The first return to the hospital occurred between 5 and 7 days after surgery, with approximately 3 additional returns during the first month depending on the vacuum drain output, which was removed only when a drainage volume < 20 ml was achieved. Additional monthly returns occurred for the first 3 months of the postoperative period and every quarter thereafter. The elastic band was retained until the second month of the postoperative period, and scar care was systematically administered.
During the review visits, any complications inherent to the abdominoplasty were identified and treated. Patients were classified as having seroma when receiving clinical diagnosis for the same and were subsequently subjected to a needle puncture for the drainage of mostly serous fluid either following vacuum drain removal or not in cases without drains. Patients were considered to have hematoma if they presented with a >500-ml volume of bloody drainage in the vacuum drain within the first 24 hours after surgery. For cases in which drains were not used, major skin ecchymoses and the resulting formation of bloody accumulations were evaluated and subsequently submitted to needle puncture. Patients were considered to have an infection whenever therapeutic antibiotic use was required as a result of abscesses, cellulitis, or larger wound infections. Smaller and superficial wounds were treated with topical dressings and antibiotics and were not considered in the collected data.
The data associated with each surgery were collected and inserted in table form into a Microsoft Office Excel 2010 spreadsheet (Microsoft Corp., Redmond, WA, USA). The obtained results were then compared and subjected to statistical analysis, with a P-value < 0.05 or 5% set as the level of null hypothesis rejection.
Figure 4 shows the pre- and postoperative images of some patients in this sample who underwent anchor-line abdominoplasty.
RESULTS
One hundred and thirty (130) patients underwent surgery between May 2009 and June 2012, of whom 120 were women (92.3%) and 10 were men (7.7%). The mean patient age was 38.3 years (age range, 19-66 years). Comparisons of the rates of seroma and hematoma-associated complications between the genders are shown in Tables 1 and 2.
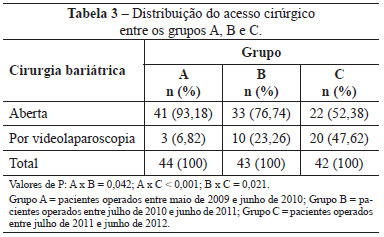
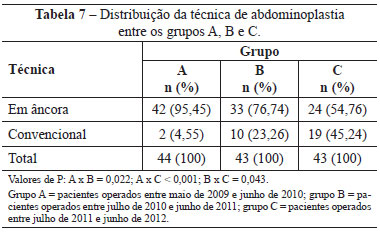
Bariatric surgery was performed between 12 and 108 months (9 years) prior to abdominoplasty, with a mean interval of 32 months (2 years and 8 months). Open bariatric surgery (i.e. supraumbilical median laparotomy) was performed in 96 (73.8%) patients and videolaparoscopy in 33 patients (25.4%); 1 (0.8%) patient lost weight without surgical treatment. Table 3 shows the access routes used for bariatric surgery in groups A, B, and C.
The most common complication during bariatric surgery was incisional hernia, which was diagnosed preoperatively in 17 patients and intraoperatively in 32 additional patients in whom small hernias originating from previous median laparotomies were present. All hernias occurred in patients who underwent open bariatric surgery, resulting in a hernia incidence of 61.5% for surgeries conducted via that access route.
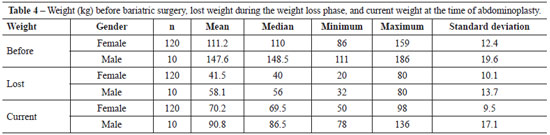
The mean time interval from weight stabilization at the time of submission to abdominoplasty was 12.1 months. The patients' weights (in kg) before bariatric surgery, amount of weight lost during the weight loss phase, and the weight at the time of abdominoplasty for both genders are presented in Table 4 along with the respective statistical analyses.
The median weight loss was 40 kg. There were no significant differences with regard to complications such as seroma, hematoma, and infection when patients who lost up to 40 kg were compared with those who lost more 40 kg, with P values of 1, 0.324, and 1, respectively. The median current weight was 70 kg. When comparing patients with weights of up to 70 kg at the time of abdominoplasty with those with weights above 70 kg, there were larger numbers of complications post-abdominoplasty, associated with seroma (12.12% vs. 35.94%; P = 0.002) and hematoma (14.06% vs. 1.52%; P = 0.008) in the first group. However, no significant difference was observed in terms of infection (3.03% vs. 7.81%; P = 0.270).
The most common complications (seromas and hematomas) associated with the use of drains and adhesive sutures within groups A, B, and C are presented in Tables 5 and 6.
The types of abdominoplasty (anchor-line or conventional) used within groups A, B, and C are shown in Table 7. No significant differences were observed between the groups when the complications of seroma, hematoma, and infection were compared with respect to the type of abdominoplasty, with P values of 0.146, 0.702, and 1, respectively.
Twenty-two patients (16.9%) underwent abdominoplasty-associated surgeries; of these, mammoplasty was the most common and was performed in 15 patients (68.2%). There were no cases of thromboembolic complications or abdominal flap necrosis. There were 14 reoperations, of which 7 (50%) were performed for scar revisions, 2 because of dehiscence, 2 because of excess skin, 2 for navel repair, and 1 for chronic seroma treatment.
Regarding the complications associated with umbilicoplasty, there was 1 case of total navel necrosis, 3 total and 4 partial cases of dehiscence, 4 cases of stenosis, and 2 cases of epidermolysis. The navel complication rate was 10.7%, of which 78% occurred in patients subjected to anchor-line abdominoplasty.
DISCUSSION
This sample of 130 individuals who underwent abdominoplasties performed by the same surgeon is significant for the detection of the most common complications in patients undergoing this type of surgery following massive weight loss; additionally, this is the largest Brazilian sample published to date5,8-11. The prospective assessment and statistical analysis contributed to the accuracy of the overall analysis, the results of which were reproducible and scientific.
The mean age of the abdominoplasty-treated patients and the gender distribution were similar to those in the previous literature8,11. The smaller proportion of men undergoing abdominoplasty is notable, given that the prevalence of men among patients undergoing bariatric surgery is approximately 20%. This discrepancy might be attributable to both the aesthetic and functional value of the abdomen for women who, in addition to prior obesity, often have a history of pregnancies that resulted in abdominal deformities. Clinically, men also appear to experience more prominent skin retraction, and often their complaints focused more on the ptosis of the pubic region than on the abdominal panniculus.
The seroma and hematoma complication rates were significantly higher among men because of the tendency of male patients to develop bleeding consequent to the effects of hormonal factors on clotting, a more significant weight loss, and a higher weight at the time of surgery, all of which contribute to increased morbidity5,8-11.
The stratification of groups A, B, and C over time with respect to the use of drains and adhesive sutures occurred along a natural curve of learning and surgical technique implementation. For group B, in which an intermediate number of adhesive sutures was applied, an expressive decrease in the vacuum drain output was already observed during the first days as well as a smaller number of days prior to drain removal. The use of adhesive sutures at intervals of 4-5 cm according to the proposal by Baroudi & Ferreira12 as well as the addition of 30 extra sutures to the anchor-line abdomen and approximately 15 extra minutes of surgery time resulted in a significant decrease in the number of seroma cases, a result that concurred with previous literature reports12-14.
There is a natural tendency to perform bariatric surgery using videolaparoscopy, as observed in this study. The training of bariatric surgeons, the growing use of the videolaparoscopic access route in both patients with private insurance and those insured by the National Health Service, the clear advantages in surgical recovery, and the lower number of complications associated with the abdominal wall are all factors that explain those results1.
In the literature, anchor-line or "fleur-de-lis" abdominoplasty or abdominoplasty with a vertical resection component have been consistently indicated for patients with supraumbilical median scars9,15. In this study, the patients from 3 cases without median scars and we selected this technique as the best option because of the large amounts of excess skin in the vertical direction or extensive skin damage. The indications for anchor-line abdominoplasties should decrease along with the decreased number of open surgeries that are replaced with conventional and circumferential surgeries6; however, residual flaccidity in the vertical direction after the performance of techniques will always present a challenge.
In this study, no significant changes were observed in the number of cases affected by hematoma or bleeding, regardless of the use of drains or adhesive sutures or of the anchor-line or conventional technique. We believe that this result was due to bleeding that originated in the superficial epigastric or superficial circumflex iliac vessels present in the horizontal incision, without interference from the adhesive sutures. In the patients in this study, these vessels had larger calibers than those in "conventional" patients, and therefore the vessels often required ligature with cotton threads. However, the conservative approach to all hematoma cases in this study, even in patients without vacuum drains, was only made possible by the use of adhesive sutures to prevent serum expansion and blood accumulation.
The stratification of patients relative to the median weight loss value and weight at the time of abdominoplasty confirmed the existing data in the literature. The morbidity incidence was greatest in patients with higher weights, a fact that must be considered during preoperative assessments, hemostatic care, surgical procedures, and when administering antibiotic and antithrombotic prophylactic therapy during the postoperative period5,10.
The indication of abdominoplasty-associated surgeries should be judicious. A surgery time > 6 hours, body mass index > 30, the presence of clinical comorbidities, and hematologic changes in the hemoglobin concentration, all of which are very common in the relevant patient group8, should represent contraindications to abdominoplasty-associated procedures. The absence of major complications in this study such as thromboembolic events and flap necroses as well as the low number of reoperations were due to rigor with respect to operative care and to the surgical indication criteria.
The literature indicates a rather strong tendency to perform neo-umbilicoplasties during abdominoplasty in patients who have experienced massive weight loss; however, we considered the number of complications associated with umbilicoplasty described in this study to be low, indicating preservation of the navel as well as good aesthetic and functional results16,17.
Abdominoplasty after massive weight loss cannot be compared to similar surgeries performed in "conventional" patients. This understanding must be clear for both the surgeon and the patients as this technique, its results, and its complications differ substantially from those associated with standard aesthetic abdominoplasties.
CONCLUSIONS
Seroma is the most common complication associated with abdominoplasty after massive weight loss and is more prevalent in men, in those with fewer than 30 adhesive sutures, and in those with body weights exceeding 70 kg. Hematoma is also more common in men and in patients with body weights exceeding 70 kg. The type of abdominoplasty (anchor-line or conventional) did not significantly affect the rates of seroma, hematoma, or infection.
ACKNOWLEDGEMENTS
I thank Wagner Allan Bertolotte, my friend and untiring colleague in surgery.
REFERENCES
1. Sociedade Brasileira de Cirurgia Bariátrica e Metabólica. Pesquisa obesidade 2010. Disponível em: www.sbcb.org.br. Acesso em 10/6/2012.
2. Capella JF, Capella RF. The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass. Am J Surg.1996;171:74-9.
3. Marema RT, Buffington CK, Perez MA. Surgical treatment of morbid obesity. In: Aly A, ed. Body contouring after massive weight loss. St Louis: QMP; 2006. p. 20-47.
4. Mitchell JE, Crosby RD, Ertelt TW, Marino JM, Sarwer DB, Thompson JK, et al. The desire for body contouring surgery after bariatric surgery. Obes Surg. 2008;18:1308-12.
5. Cavalcante HA. Abdominoplastia após perda de peso maciça: abordagens, técnicas e complicações. Rev Bras Cir Plást. 2010;25(1):92-9.
6. Aly A. Belt lipectomy. In: Aly A, ed. Body contouring after massive weight loss. St Louis: QMP; 2006. p. 72-145.
7. Pitanguy I. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. 2000;105(4):1499-514.
8. Andrade IF, Meira AAM, Ferreira FPM. Abdominoplastia após a cirurgia bariátrica: aspecto laboratorial. Rev Bras Cir Plást. 2007;22(3):158-61.
9. Lage RR, Amado BN, Sizenando RP, Heitor BS, Ferreira BM. Dermolipectomia abdominal pós-gastroplastia: avaliação de 100 casos operados pela técnica do "peixinho". Rev Bras Cir Plást. 2011;26(4):675-9.
10. Tardelli HC, Vilela DB, Schwartzmann GLE, Azevedo MA, Mello Júnior AC, Farina Júnior JA. Padronização cirúrgica das abdominoplastias em âncora pós-gastroplastia. Rev Bras Cir Plást. 2011;26(2):266-74.
11. Orpheu SC, Coltro PS, Scopel GP, Saito FL, Ferreira MC. Body contour surgery in the massive weight loss patient: three year-experience in a secondary public hospital. Rev Assoc Med Bras. 2009;55(4):427-33.
12. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
13. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119(3):1060-6.
14. Arantes HL, Rosique RG, Rosique MJF, Mélega JMA. Há necessidade de drenos para prevenir seroma em abdominoplastias com pontos de adesão? Rev Bras Cir Plást. 2009;24(4):521-4.
15. Wallach SG. Abdominal contour surgery for the massive weight loss patient: the fleur-de-lis approach. Aesthet Surg J. 2005;25(5):454-65.
16. Cavalcanti ELF. Neoumbilicoplastia como opção de reconstrução umbilical nas dermolipectomias abdominais em âncora pós-gastroplastia. Rev Bras Cir Plást. 2010;25(3):509-18.
17. Silva FN, Oliveira EA. Neo-onfaloplastia na abdominoplastia vertical. Rev Bras Cir Plást. 2010;25(2):330-6.
Masters in Clinical Surgery, full member of the Brazilian Society of Plastic Surgery, plastic surgeon at the Waldemar Monastier Children's Regional Hospital in Campo Largo, and plastic and craniofacial surgeon at the Integrated Care Center for Patients with Cleft Lip and Palate, Curitiba, PR, Brazil
Correspondence to:
Lady Wilson Canan Junior
Travessa Ferreira do Amaral, 45 - 3º andar - Água Verde
Curitiba, PR, Brazil - CEP 80620-090
E-mail: lwcananjr@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 7/22/2012
Article accepted: 12/15/2013
This study was conducted at Vitória Hospital, Curitiba, PR, Brazil.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter