

Original Article - Year 2013 - Volume 28 - Issue 3
Functional capacity of patients after breast reconstruction with a latissimus dorsi musculocutaneous flap
Capacidade funcional de pacientes submetidas a reconstrução mamária com retalho musculocutâneo de latíssimo do dorso
ABSTRACT
BACKGROUND: The latissimus dorsi muscle is responsible for the adduction, extension, and internal rotation of the humerus, and has a crucial role in the stability of the glenohumeral joint. Some authors believe that the removal of this muscle has a minimal effect on shoulder morbidity, as the residual shoulder muscles would compensate for its absence; in contrast, other authors have noted weakness, loss of movement ability, pain, and functional change. Most studies, however, were not limited to patients who undergo breast surgery and were retrospective in nature. The measurement modalities used were based on subjective methods and were not standardized; furthermore, there is little information on their reliability. Few studies compared the results with preoperative measurements. Therefore, an objective study requires the prospective assessment of patients who undergo late breast reconstruction with a latissimus dorsi musculocutaneous flap, by using the Stanford Health Assessment Questionnaire (HAQ).
METHOD: Between September 2010 and April 2012, 30 patients were enrolled in the study. They answered the HAQ at preoperative consultations and postoperatively at 3, 6, and 12 months.
RESULTS: A statistically significant difference was found between the stages of assessment, with a deterioration of postoperative functional capacity at 3 months after surgery, which returned to preoperative levels after 6 months and progressively improved until 12 months after surgery.
CONCLUSIONS: This study offers scientific evidence suggesting that breast reconstruction surgery with a latissimus dorsi musculocutaneous flap does not worsen the functional capacity of patients at 12 months after surgery.
Keywords: Mammaplasty. Latissimus dorsi muscle. Mastectomy. Questionnaires. Quality of life. Functional capacity. Surgical flaps.
RESUMO
INTRODUÇÃO: O músculo latíssimo do dorso tem a função de adução, extensão e rotação interna do úmero, com papel crucial na estabilidade da articulação glenoumeral. Para alguns autores a retirada desse músculo tem pouco efeito na morbidade do ombro, uma vez que os músculos residuais do ombro compensariam sua falta, enquanto outros têm notado fraqueza, perda de movimentos, dor e alteração funcional. Os estudos, em sua maioria, não são limitados a pacientes submetidas a cirurgia mamária, são retrospectivos, e as modalidades utilizadas para essa medição se apoiam em metodologia subjetiva, não são padronizadas e também há poucas informações sobre sua confiabilidade. Poucos comparam os resultados com as medidas pré-operatórias. O objetivo deste estudo é avaliar de maneira prospectiva a capacidade funcional das pacientes submetidas a reconstrução mamária tardia com retalho musculocutâneo de latíssimo do dorso utilizando o Stanford Health Assessment Questionnaire (HAQ).
MÉTODO: No período de setembro de 2010 a abril de 2012, 30 pacientes ingressaram no estudo. Essas pacientes responderam ao HAQ nas consultas de pré-operatório e aos 3 meses, 6 meses e 12 meses de pós-operatório.
RESULTADOS: Houve diferença estatisticamente significante entre os tempos de avaliação, sendo detectada piora da capacidade funcional aos 3 meses de pós-operatório, que retornou aos níveis do pré-operatório após 6 meses e foi melhorando progressivamente até os 12 meses de pós-operatório.
CONCLUSÕES: Este estudo oferece evidência científica de que a cirurgia de reconstrução mamária com retalho musculocutâneo de latíssimo do dorso não piora a capacidade funcional das pacientes 12 meses após a cirurgia.
Palavras-chave: Mamoplastia. Músculo latíssimo do dorso. Mastectomia. Questionários. Qualidade de vida. Capacidade funcional. Retalhos cirúrgicos.
In accordance with the data estimated by the Instituto Nacional do Câncer, 52,680 new cases of breast cancer were registered in Brazil in 2012, becoming the second most common type of cancer in women, with the highest mortality rate. The most common treatment methods include surgery (nodulectomy or mastectomy), chemotherapy, radiotherapy, and hormone therapy; usually, 2 or more methods are used complementarily.
The removal of the breast causes esthetic and functional problems with immediate physical and psychological repercussions that could be traumatic for most women and reduce their quality of life1. Despite the frequent success of therapy, many adverse effects have been observed that lead to a considerable functional decline. The effects experienced by patients are related to the type of treatment used, with fatigue being the most commonly observed, affecting at least 30% of all surviving patients2. This forced reduction in the levels of physical activity causes a pathological condition that, when associated with other adverse effects such as loss of appetite, can intensify the physical strain and, consequently, lead to a loss of total muscle strength. This loss in muscle strength is yet another factor that affects the ability of cancer patients to carry out simple daily tasks, considerably compromising their quality of life2.
For women who will undergo a mastectomy, breast reconstruction is a surgical option that generally promotes their quality of life and psychosocial adjustment without reducing their chances for survival, independent of the stage of their disease3. Breast reconstruction can be achieved with many techniques, including the use of the latissimus dorsi musculocutaneous flap.
The latissimus dorsi muscle is responsible for the adduction, extension, and internal rotation of the humerus, and has a crucial role in maintaining the stability of the glenohumeral joint. Many authors4-7 have established that the removal of the latissimus dorsi muscle has a minimal effect on shoulder morbidity, as the residual shoulder muscles compensate for its loss. Others8,9, however, have noted weakness, loss of movement ability, pain, and functional change. However, most of the previous studies were not limited to patients who underwent breast surgery, and were retrospective in nature. Furthermore, the measurement modalities used were based on subjective methods and were not standardized; in addition, there is little information on their reliability10. Few studies10,11 compared the results with preoperative measurements.
Functional capacity refers to much more than physical performance alone; it indicates how well patients could carry out their daily activities. Functional capacity determines how well patients deal with their disease in terms of their daily routines; it is dependent on the individual patient and is determined by an interaction between clinical variables and psychosocial factors. It has been used as a health assessment parameter related to the quality of life12.
The use of the latissimus dorsi musculocutaneous flap has been reported to result in a minimal change in functional capacity4-5; however, the instruments used for measurement are difficult to standardize and have questionable reliability11. In general, there is consensus in the existing literature that most of the women who undergo breast surgery will experience transitory morbidity; however, "normal" functional capacity will return after breast reconstruction with a latissimus dorsi musculocutaneous flap. Nevertheless, it seems necessary to assess such changes by using an instrument that can objectively measure the effect on global function rather than focusing on the measurement of isolated movements11. Functional capacity should therefore be measured by using standardized, validated, reliable, and reproducible methods.
For such a purpose, questionnaires that are able to objectively collect, quantify, and compare subjective data should be used. They must be easy to apply and understand, valid, reproducible, and reliable, and should have a suitable administration time.
The objective of this study was to prospectively assess the functional capacity of patients after breast reconstruction with a latissimus dorsi musculocutaneous flap, by using the Stanford Health Assessment Questionnaire (HAQ).
METHODS
This prospective cohort study was conducted at Programa de Pós-Graduação em Cirurgia Translacional, Universidade Federal de São Paulo (Escola Paulista de Medicina) and Pérola Byington and A.C. Camargo hospitals, both in São Paulo, Brazil, between September 2010 and April 2012. The study protocol was approved by the relevant local ethics committees.
All surgeries were conducted by the same surgeon, in accordance with the standard transfer technique of the latissimus dorsi muscle flap, with a cutaneous horizontal flap and introduction of a breast implant (Figure 1) in addition to adhesion sutures (Baroudi sutures) for the closure of the donor area (Figure 2). Vacuum suction drains were placed in the anterior and posterior thoracic areas and were maintained for 5-10 days, on average.
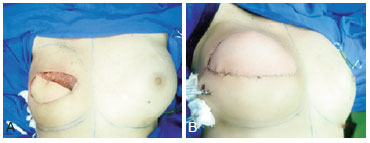
Figure 1 - A, transoperative flap rotation. B, posterior placement of the silicone implant and introduction of suction drainage.

Figure 2 - A, transoperative creation of the flap. B, adhesion sutures.
Thirty-five consecutive patients who began attending the Department of Plastic Surgery were selected.
The included patients were women who underwent unilateral modified radical mastectomy owing to an oncological indication, with adjuvant treatment ending after at least 1 year; these patients were between 18 and 70 years of age and subsequently underwent breast reconstruction with a latissimus dorsi musculocutaneous flap.
Patients with a local recurrence or systemic relapse, previous surgery to the latissimus dorsi muscle, illiteracy, previous psychiatric treatment, smoking habits, a body mass index of > 30 kg/m2, or a chronic insufficiency disease were excluded.
The collection procedure began with the patients voluntarily signing the informed consent form, after reading the information leaflet. The HAQ was applied to assess functional capacity.
The HAQ is one of the most frequently used tools for assessing functional capacity; it consists of 20 questions that assess different aspects of patients' daily life, such as dressing, getting out of bed, eating, walking, hygiene, reaching objects, physical exertion, and outdoor activities. Functional capacity as assessed with the HAQ has been significantly correlated with work-related measures, such as work capacity, completion of household tasks, work incapacity, occupation, and the ability to live independently13. The version used in this study was translated into Portuguese, adapted to Brazilian culture, and validated14.
Patients answered the HAQ during preoperative consultations and postoperatively at 3, 6, and 12 months after surgery. The same researcher applied the questionnaire throughout the study period.
During the first postoperative month, all patients attended a weekly session of outpatient physiotherapy and were instructed on how to perform daily exercises at home.
Statistical Analysis
To fulfill the study objectives, first, the Pearson correlation was calculated between age and the HAQ score at each stage of assessment, to determine whether the presence of a relationship between age and functional capacity.
The patients' age was described with summary measurements (mean, standard deviation, median, and minimum and maximum). For HAQ scores, measurements were taken at each assessment stage and were compared by using repeated measures analysis of variance. When making multiple comparisons, Bonferroni's correction was employed to determine exactly when differences occur between scores of functional capacity.
The results are illustrated with a mean profile chart with the respective standard error, and tests were conducted at a 5% significance level.
RESULTS
Of the total of 35 patients initially selected for the study, 2 refused to participate, 2 died due to breast cancer relapse before reconstruction, and 1 moved out of the state and did not return for postoperative consultations; they were excluded from the study. Therefore, 30 patients were effectively enrolled.
All patients underwent unilateral breast reconstruction, 20 of whom underwent latissimus dorsi muscle transfer of the dominant side, and 10, of the nondominant side. Concerning immediate complications, 1 patient (3.33%) presented seroma, which was resolved with repeated puncture-aspiration. One patient (3.33%) presented partial dehiscence of the wound with prosthesis exposure, which required removal; this patient underwent prosthesis replacement surgery after 6 months. Concerning late complications, 7 patients (23.3%) complained of unsightly scars.
The mean age of patients was 46.4 years (range, 24-70 years). There was no statistically significant correlation between patient age and the functional capacity scores at any of the assessed stages (P > 0.05). This means that the functional capacity measured by the HAQ was not affected by age.
The mean functional capacity scores (Table 1) were significantly different between stages of assessment (P = 0.023). The mean functional capacity score was significantly different between before surgery and 3 and 6 months postoperatively (Table 2) (P > 0.05), it decreased significantly from before surgery to 12 months postoperatively (P = 0.029), and it decreased significantly between the remainder of the assessed times (P < 0.05). This is because initially (3 months postoperatively), the patients presented deteriorated functional capacity (increase in the HAQ score), which returned to preoperative levels after 6 months and improved progressively (decrease in the HAQ score) until 12 months postoperatively (Figure 3).
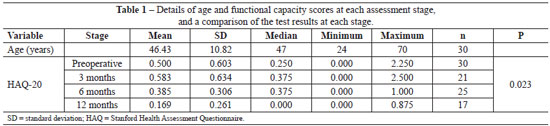
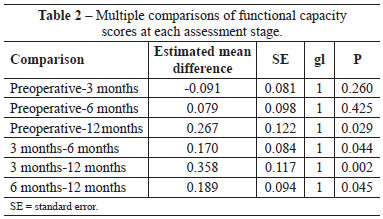
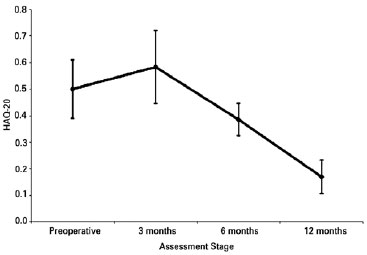
Figure 3 - Graph showing a visible mean reduction in the functional capacity score from 6 months. HAQ = Stanford Health Assessment Questionnaire.
Figures 4 to 7 illustrate 4 of the cases described in this case study.

Figure 4 - A to D, surgical marks from the frontal, left oblique, left lateral, and posterior views. E and F, frontal and left oblique postoperative views at 6 months. G and H, postoperative frontal and left oblique views at 12 months.

Figure 5 - A, C, and E, preoperative frontal, right oblique, and right lateral views. B, D, and F, postoperative frontal, right oblique, and right lateral views at 12 months.

Figure 6 - A and B, preoperative frontal and left oblique views. C and D, postoperative frontal and left oblique views at 6 months. E and F, postoperative frontal and left oblique views at 12 months, after symmetrization.

Figure 7 - A and B, preoperative frontal and right oblique views. C and D, postoperative frontal and right oblique views at 6 months. E and F, postoperative frontal and right oblique views at 9 months and after symmetrization. G and H, postoperative frontal and right oblique views at 12 months, after areolar-papillary complex reconstruction.
DISCUSSION
Anatomically, the latissimus dorsi muscle is part of the shoulder belt muscles. This muscle is flabelliform in shape (i.e., like a fan), which is due to the spinous processes of the thoracic, lumbar, and sacral vertebrae; the iliac crest; and the lumbar fascia. This muscle converges and runs around a larger round muscle as it inserts into the greater tubercle of the humerus. Its primary roles are the adduction, internal rotation, and extension of the shoulder. These actions are particularly relevant in sports activities such as swimming, gymnastics, rowing, and climbing15.
The complications that could occur after a latissimus dorsi musculocutaneous flap transfer are uncommon, and can be categorized as immediate or late complications. Immediate complications include partial or total flap necrosis (rare), hematomas, seromas, dehiscence, and infection. On the other hand, some of the possible late complications include hypertrophic scarring or keloids, capsular contracture with cranial displacement of the prosthesis, change to the reconstructed breast due to contracture of the latissimus dorsi muscle on the prosthesis, and extrusion of the prosthesis16.
The functional capacity of the shoulder has been assessed with objective measurements, such as the range of movement and muscle strength. Nevertheless, objective measurements can prove impracticable in certain situations because they require too much time and direct contact with the patient. Furthermore, although functional limitation of the shoulder is frequently associated with a restriction in the range of movement and muscular weakness, these measurements do not always present direct clinical significance for patients, whose main concern is to live their daily lives without pain. Currently, treatment efficiency has been more frequently assessed by using results that have direct relevance to patients17.
Bochdansky et al.7 assessed the postoperative functional capacity of 26 patients who underwent reconstruction of the lower limb by using the latissimus dorsi flap on the dominant side of the body. No effects of the surgery or on dominance were observed in terms of isometric muscular strength, measured with an electronic device (Hottinger-Baldwin-Messtechnik). The authors believe that latissimus dorsi muscle function can be compensated for by synergistic muscles. This is consistent with the results obtained in our study and also those of other authors18, which offer evidence suggesting that the muscle continues to influence shoulder movement. The retrospective nature of the study and the fact that the latissimus dorsi muscle was used as a free flap limits specific analysis for breast reconstruction.
Brumback et al.5 compared the dominant and nondominant sides of 17 patients after the free flap transfer of the latissimus dorsi in 17 healthy volunteers, by using a functional questionnaire, a manual muscle strength test, and an objective test of muscle strength conducted with the use of instruments. No significant difference was observed in the range of movement, strength, or function of the shoulder during monitoring for a mean of 41 months (range, 21-96 months). Therefore, it was established that a comparison in range of movement between the 2 groups was inappropriate, given that shoulder movement can vary within a normal population.
Martino et al.18 extensively described the biomechanical sequelae resulting from reconstruction with a latissimus dorsi musculocutaneous flap. The authors concluded that approximately two-thirds of the women presented movement limitation in the shoulder area after the reconstruction with a latissimus dorsi musculocutaneous flap. More than 20% of patients presented some degree of shoulder joint microdislocation, which can be clinically detected by palpation. After late breast reconstruction with a latissimus dorsi musculocutaneous flap, this muscle can continue to influence the medial rotation of the humerus; however, instead of an inferoposterior pull, it performs anterosuperior pulling, resulting in microdislocation. This abnormal medial rotation results in weakening of the lateral rotators. Nevertheless, despite the objective methods used, their measurements did not consider the daily activities of patients and did not necessarily present clinical significance. In our study, we used an assessment method that is aimed at detecting changes that will effectively lead to significant functional limitations in patients.
Adams et al.9, in a retrospective study, sent an unvalidated questionnaire by post to 36 patients who underwent breast reconstruction with a latissimus dorsi musculocutaneous flap. Their analysis showed that up to 39% of patients reported at least moderate weakness, 50% reported numbness/pressure to the dorsal region, and 22% considered their scarring to be unacceptable. Many patients had difficulty in carrying out more vigorous daily activities (P < 0.05) compared to more sedentary activities. The authors concluded that the use of a latissimus dorsi musculocutaneous flap is not fully without the risk of postoperative morbidity at the donor site. These numbers are similar to our results; however, this study, aside from being prospective in nature, employed a validated questionnaire.
In a literature review, Spear & Hess6 examined the evidence of biomechanical and functional changes to the shoulder after a latissimus dorsi muscle transfer. They concluded that, postoperatively, patients presented deficits in shoulder extension and adduction manifested by more rapid fatigue. However, this conclusion was based on studies with retrospective data and with no objective tests. Our study compared the same patients at both the preoperative and postoperative stages, whereas the analyzed studies made comparisons with the contralateral side or with a control group. Furthermore, those studies were also not restricted to breast reconstruction cases only.
Glassey et al.10, in a prospective study on 22 patients analyzed using objective parameters, concluded that there is no significant reduction in the range of shoulder movement, strength and function, or pain at 1 year after breast reconstruction with a latissimus dorsi musculocutaneous flap. However, the heterogeneity of the study population (17 patients with late and 5 with immediate reconstruction) may have generated a bias. In addition, the authors believe that the small sample size was inappropriate for the statistical analysis of results. In our study, all patients underwent late breast reconstruction with a latissimus dorsi musculocutaneous flap. We believe that this sample homogeneity coupled with a validated and objective method of assessment guarantees greater result reliability.
Button et al.11, in a prospective study, assessed the changes in DASH questionnaire scores throughout monitoring and the use of adhesion sutures for reduced seroma formation in the painful regions of patients undergoing immediate breast reconstruction with a latissimus dorsi musculocutaneous flap. The questionnaire was applied before surgery and at 8 postoperative stages, from the first visit until 3 years. The authors concluded that the DASH score increased during the first 3 months (deterioration) and later decreased with time until 36 months, despite being at a higher level than before surgery; they did not find clinical or statistical significance. Another conclusion was that adhesion sutures reduced seroma to painful areas (5% vs. 70%) but did not change the DASH score. In the same study, the authors showed that, despite the long-term normalization of function, there was initially a significant harmful impact, which requires specific measures other than patient guidance. They also report that oncology therapy (radiotherapy, chemotherapy, and tamoxifen administration) does not have a significant impact on the long-term functional capacity of the shoulder, and that the morbidity from axillary oncology surgery disappears within 6-12 months.
Activity limitation, restriction to upper limb movement, lymphedema, fatigue, pain, and peripheral neuropathy induced by chemotherapy are well-documented problems that occur after the treatment of breast cancer19. Mastectomy and adjuvant treatments can, independently, generate some functional incapacity or limitations20. In this way, early and late postoperative assessment results may have reflected the effect of both mastectomy and breast reconstruction. In our study, we only assessed patients with late breast reconstruction to eliminate the possibility of bias, as the effect of mastectomy was already experienced before reconstruction surgery (shown by a higher preoperative score). We also found that the final score was lower than the initial score, which we believe to be a consequence of the patients' capacity to adjust to a new physical condition.
CONCLUSIONS
This study offers scientific evidence showing that breast reconstruction with a latissimus dorsi musculocutaneous flap does not worsen the functional capacity of patients at 12 months after surgery.
REFERENCES
1. Arán MR, Zahar S, Delgado PGG, Souza CM, Cabral CPS, Viegas M. Representações de pacientes mastectomizadas sobre doença e mutilação e seu impacto no diagnóstico precoce do câncer de mama. J Bras Psiquiatr. 1996;45(11):633-9.
2. Dimeo F, Fetscher S, Lange W, Mertelsmann R, Keul J. Effects of aerobic exercise on the physical performance and incidence of treatment-related complications after high-dose chemotherapy. Blood. 1997;90(9):3390-4.
3. Harcourt D, Rumsey N. Psychological aspects of breast reconstruction: a review of the literature. J Adv Nurs. 2001;35(4):477-87.
4. Laitung JK, Peck F. Shoulder function following the loss of the latissimus dorsi muscle. Br J Plast Surg. 1985;38(3):375-9.
5. Brumback RJ, McBride MS, Ortolani NC. Functional evaluation of the shoulder after transfer of the vascularized latissimus dorsi muscle. J Bone Joint Surg Am. 1992;74(3):377-82.
6. Spear SL, Hess CL. A review of the biomechanical and functional changes in the shoulder following transfer of the latissimus dorsi muscle. Plast Reconstr Surg. 2005;115(7):2070-3.
7. Bochdansky T, Utku Y, Zauner-Dungl A, Schemper M, Piza-Katzer H. Evaluation of shoulder function after removal of the latissimus dorsi muscle for surgical flap. Handchir Mikrochir Plast Chir. 1990;22(6):321-5.
8. Fraulin FO, Louie G, Zorrilla L, Tilley W. Functional evaluation of the shoulder following latissimus dorsi muscle transfer. Ann Plast Surg. 1995;35(4):349-55.
9. Adams WP Jr, Lipschitz AH, Ansari M, Kenkel J, Rohrich RJ. Functional donor site morbidity following latissimus dorsi muscle flap transfer. Ann Plast Surg. 2004;53(1):6-11.
10. Glassey N, Perks GB, McCulley SJ. A prospective assessment of shoulder morbidity and recovery time scales following latissimus dorsi breast reconstruction. Plast Reconstr Surg. 2008;122(5):1334-40.
11. Button J, Scott J, Taghizadeh R, Weiler-Mithoff E, Hart AM. Shoulder function following autologous latissimus dorsi breast reconstruction. A prospective three year observational study comparing quilting and non-quilting donor site techniques. J Plast Reconstr Aesthet Surg. 2010;63(9):1505-12.
12. Freire M, Sabino Neto M, Garcia EB, Quaresma MR, Ferreira LM. Functional capacity and postural pain outcomes after reduction mammaplasty. Plast Reconstr Surg. 2007;119(4):1149-56.
13. Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol. 2003;30(1):167-78.
14. Ferraz MB, Oliveira LM, Araujo PM, Atra E, Tugwell P. Crosscultural reliability of the physical ability dimension of the health assessment questionnaire. J Rheumatol. 1990;17(6):813-7.
15. Moore KL, Dalley AF. Clinically oriented anatomy. 4th ed. Baltimore: Lippincott Williams & Wilkins; 1999.
16. Mélega JM. Cirurgia plástica: fundamentos e arte. Cirurgia reparadora de tronco e membros. 2nd ed. Rio de Janeiro: Guanabara Koogan; 2004.
17. Bot SD, Terwee CB, van der Windt DA, Bouter LM, Dekker J, de Vet HC. Clinimetric evaluation of shoulder disability questionnaires: a systematic review of the literature. Ann Rheum Dis. 2004;63(4):335-41.
18. Martino G, Godard H, Nava M. Breast reconstruction with myocutaneous flaps: biomechanical aspects. In: dell Rovere Q, Benson JR, Beach N, Nava M, eds. Oncoplastic and reconstructive surgery of the breast. New York: Taylor & Francis; 2004. p. 141-9.
19. Hayes SC, Rye S, Battistutta D, DiSipio T, Newman B. Upper-body morbidity following breast cancer treatment is common, may persist longer-term and adversely influences quality of life. Health Qual Life Outcomes. 2010;8:92.
20. Nesvold IL, Fossa SD, Holm I, Naume B, Dahl AA. Arm/shoulder problems in breast cancer survivors are associated with reduced health and poorer physical quality of life. Acta Oncol. 2010;49(3):347-53.
1. Plastic Surgeon of the Universidade Federal de Mato Grosso, Full Member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Cuiabá, MT, Brazil
2. Associate professor, Department of Plastic Surgery, Escola Paulista de Medicina, Federal University of São Paulo (EPM-UNIFESP), Full Member of the SBCP, São Paulo, SP, Brazil
3. Plastic Surgeon, Full Member of the SBCP, Full Member of the Department of Reconstructive Plastic Surgery of Hospital do Câncer-Fundação Antônio Prudente, São Paulo, SP, Brazil
4. Plastic surgeon, Full Professor of Plastic Surgery at EPM-UNIFESP, Full Member of the SBCP, São Paulo, SP, Brazil
Correspondence to:
Vidal Guerreiro
Rua Bom Pastor, 1.426 - ap. 43 - Ipiranga
São Paulo, SP, Brazil - CEP 04203-001
E-mail: drvidalguerreiro@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 27/7/2012
Article accepted: 15/12/2013
This study was conducted at Programa de Pós-Graduação em Cirurgia Translacional, Universidade Federal de São Paulo (Escola Paulista de Medicina) and Pérola Byington and A. C. Camargo hospitals, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter