

Original Article - Year 2013 - Volume 28 -
Mini-retromandibular transparotid approach for extracapsular condylar fractures of the mandible
Acesso retromandibular transparotídeo reduzido para o tratamento de fraturas extracapsulares do côndilo mandibular
ABSTRACT
BACKGROUND: Most of the current research has highlighted the need for establishing a surgical procedure for the treatment of extracapsular condylar fractures of the mandible, in case with large deviations or when the fractures are associated with other mandibular and/or fractures of the middle third of the face. Here, we aimed to describe the surgical details and postoperative outcomes of the mini-retromandibular transparotid approach for the treatment of extracapsular condylar fractures of the mandible.
METHOD: An analysis was conducted among 14 patients with extracapsular condylar fractures of the mandible who presented indications for surgical treatment and underwent the surgery between March 2011 and March 2012.
RESULTS: In this case series, the anatomical and functional outcomes achieved were satisfactory and the rate of complications was low.
CONCLUSIONS: The mini-retromandibular transparotid approach offers advantages and should be included as an option for the surgical treatment of extracapsular condylar fractures of the mandible.
Keywords: Mandibular fractures. Mandible/surgery. Mandibular condyle/surgery.
RESUMO
INTRODUÇÃO: A maioria dos trabalhos atuais enfatiza a necessidade de tratamento cruento das fraturas extracapsulares do côndilo mandibular, quando estas apresentam grandes desvios ou estão associadas a outras fraturas mandibulares e/ou terço médio da face. Este artigo tem por objetivo descrever detalhes cirúrgicos e resultados pós-operatórios do uso do acesso retromandibular transparotídeo reduzido para o tratamento das fraturas extracapsulares do côndilo mandibular.
MÉTODO: Foram analisados 14 pacientes portadores de fraturas extracapsulares de côndilo mandibular, com indicação de tratamento cirúrgico, operados no período de março de 2011 a março de 2012.
RESULTADOS: Nesta série de pacientes, os resultados anatômicos e funcionais foram considerados satisfatórios e foi observado baixo índice de complicações.
CONCLUSÕES: O acesso retromandibular transparotídeo reduzido oferece vantagens e deve ser incluído como opção para o tratamento cruento das fraturas extracapsulares do côndilo mandibular.
Palavras-chave: Fraturas mandibulares. Mandíbula/cirurgia. Côndilo mandibular/cirurgia.
The incidence rate of condylar fractures of the mandible varies in the literature-between 17.5% and 52%1. Condylar fractures of the mandible are considered the most controversial mandibular fractures in terms of diagnosis and treatment2. Most condylar fractures of the mandible are due to direct trauma. However, they may be induced by the impact of the transmission of the forces to the adjacent condyles, which is a symptom that may not be recognized and therefore may not properly diagnosed3.
An increasing number of publications have reported poor outcomes of conservative treatment of extracapsular fractures; in fact, conservative treatment was found to significantly increase the risk for functional disorders4. With an increase in the number of surgical indications for the management of extracapsular fractures, discussion of the advantages and disadvantages of the different surgical approaches available currently has become important. Several approaches have already been described for the surgical treatment of extracapsular condylar fractures of the mandible, such as the pre-auricular, submandibular, retromandibular, and intraoral approaches5. The approach chosen for the surgical treatment should always provide the surgeon with the proper visualization of the fracture site to allow for optimal anatomical and functional restorations of the mandible6.
Here, we aimed to describe the surgical details and postoperative outcomes of the mini-retromandibular transparotid approach for the treatment of extracapsular condylar fractures of the mandible.
METHODS
An analysis was conducted that involved 14 patients with extracapsular condylar fractures of the mandible who presented with indications for surgical treatment and underwent surgery by the same surgeon between March 2011 and March 2012. These patients were hospitalized in a well-known trauma center and initially examined by a general surgeon. All the patients underwent clinical examination and, subsequently, radiography and facial computed tomography.
Indication for Surgical Treatment
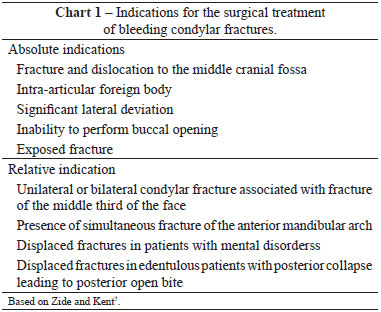
Although no consensus has been reached in the international literature on the indications for open treatment of condylar fractures4,7, a series of criteria for the indication of surgical treatment of extracapsular condylar fractures of the mandible was established and is described in Table 1.
Surgical Technique
The patients underwent surgery under general anesthesia, which was induced via intubation with a nasotracheal cannula. Thereafter, local anesthesia was administered by infiltration with an anesthetic solution of bupivacaine and epinephrine (1:200,000). This was an important step in that it not only allowed for bleeding control during the dissection and ensured the patient's comfort during the postoperative period but also served as a guide for performing a proper incision, as it was possible to search for the fracture site with the tip of the needle (Figure 1).

Figure 1 - Local anesthesia.
Once the site for surgical access was delimited, the skin was incised up to the subcutaneous tissue (Figure 2). Thereafter, tissues of the parotid gland and masseter muscle were divulsed until the fracture site (Figures 3 and 4). Langenbeck retractors were used to separate the fracture site from posterior border of the neck of the mandibular condyle for visualization. The perfect similarity between the recesses and protrusions of the fractured bone segments enabled fracture reduction to be achieved.

Figure 2 - Skin incision.

Figure 3 - Divulsion through the parotid gland and masseter muscle.
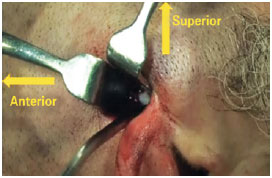
Figure 4 - Proper separation for visualization of the fracture site.
Backaus forceps (Figure 5) was used to pull the anterior arch of the mandible as a superior vector to overcome the force caused by the action of the abductor muscles of the mandible. This step assisted in the repositioning of the distal segment of the mandible and also facilitated the repositioning of the proximal fragment (usually dislocated by the action of the lateral pterygoid muscle).
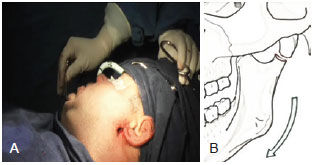
Figure 5 - Retraction of the anterior arch. A, The Backaus forceps used in the retraction. B, A schematic diagram of the mandibular movements.
Once the fracture was reduced, osteosynthesis was performed with miniplates (a 2-mm system). It is worth mentioning the order by which the screws were placed, starting with the point closest to the fracture site in the proximal segment, followed by the point nearest to the fracture site in the distal segment. Thereafter, the screws were placed in the area located as far as possible from the most proximal segment of the fracture site and, finally, the area located as far as possible from the most distal segment of the fracture (Figure 6).
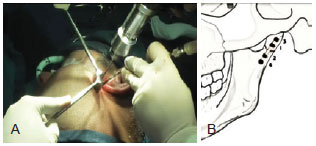
Figure 6 - A, Correct positioning for the osteosynthesis. B, Order of placement of the screws.
After finding the perfect reduction and fixation of the fracture, the outcome of the repair of the occlusion was assessed. The patients were not immobilized unless this measure was indicated by the presence of intracapsular and contralateral fractures or other fractures of the middle third of the face. The incision was closed in two planes.
After recovery from anesthesia, the patients remained hospitalized for 24 hours and underwent radiography control to assess and confirm the fracture reduction. Antibiotic prophylaxis was administered only during anesthesia.
The patients were discharged and provided with a prescription for symptomatic drugs and guidance regarding a 40-day liquid diet. The patients were monitored weekly, and after 40 days of restricted diet, they gradually shifted to higher-density diets toward eating regular, unrestricted food without displaying any symptoms.
RESULTS
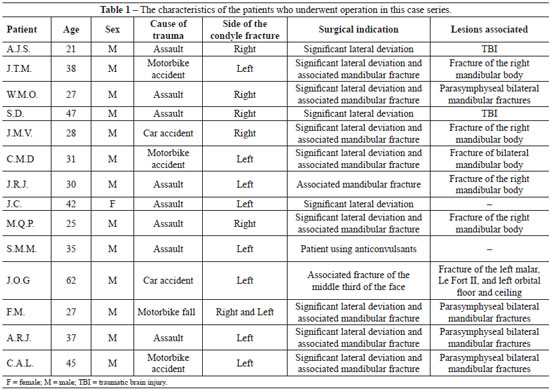
The mean age of the patients was 35 years. Among the 14 patients who underwent surgery, only one was female. The patients did not present with significant comorbidities, and only one patient was using anticonvulsants.
In the postoperative period, the patients evolved satisfactorily. Only two patients had purulent drainage in the fracture region, for which they were treated with antibiotic therapy in an outpatient setting and thereby showed complete resolution of the drainage.
The patients did not show any difficulty in the healing of the surgical wound through which the condylar fractures were accessed. Only one patient presented with paresis of the buccal branch of the facial nerve and was treated with physiotherapy, which achieved complete resolution after 2 months.
The characteristics of the patient cohort in the present study are listed in Table 1.
None of the patients required reoperation. Figures 7 and 8 present the cases of 2 patients who achieved perfect fracture reduction. Figure 9 shows that the occlusion was quite close to that prior to trauma. The scars were barely visible, as shown in Figure 10.
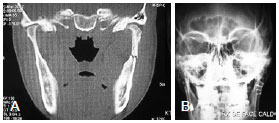
Figure 7 - Patient J.R.J. A, Preoperative computed tomographic image. B, Postoperative radiograph.
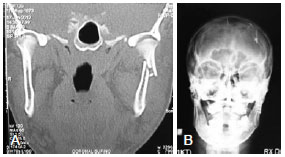
Figure 8 - Patient C.A.L. A, Preoperative computed tomographic image. B, Postoperative radiograph.

Figure 9 - Appearance 2 months after surgery, indicating reestablishment of the occlusion.

Figure 10 - Appearance 4 months after surgery, revealing a barely visible scar.
DISCUSSION
Condylar fractures of the mandible are classified as either intracapsular or extracapsular8. They are also divided anatomically into head condylar (intracapsular), neck condylar (extracapsular), and subcondylar fractures9, according to the scheme presented in Figure 11.

Figure 11 - Anatomy of the condylar fractures of the mandible.
Condylar fractures of the mandible may also be classified according to the degree of deviation as follows: not diverted, with deviation but maintaining bone continuity, and with dislocation of bone fragments (medial, lateral, or no mandibular condyle in the glenoid cavity)10. Displacement of the fractured segments was influenced by several factors such as direction of the impact, magnitude of the trauma, and exact point on which the force was applied, along with the patient's dental conditions and the presence of occlusion prior to trauma11. The presence of molar teeth in contact, in the neutral occlusion, during the trauma, will cause fractures with little or no dislocation. Conversely, in cases in which there is no dental contact or the mouth is open during trauma, transmission of the force typically leads to large displacements of the fractured segments12.
For diagnosis, the main parameter analyzed is dental occlusion. However, the objective evaluation of this occlusion does not always correlate with the discomfort reported by the patients13. Performing a facial tomography, in coronal and axial sections, is also essential, as it provides the surgeon with information of the fracture anatomy5.
In the literature, the indication for surgical treatment of extracapsular condylar fractures of the mandible varies significantly14. For a long time, conservative treatment had been considered to be standard owing to the technical difficulties in reducing fractured fragments, besides the possibility of nerve injury to facial nerve branches during surgery15. In the follow-up of patients treated conservatively, functional disorders and facial growth were observed in a large number of patients9. Therefore, surgical treatment is currently indicated for adults whose radiographic findings demonstrate the presence of displaced condyle fractures that cause clinical repercussions. Moreover, there are some other absolute and relative indications (Chart 1). Conservative treatment remains the best option for patients with nondisplaced, intracapsular, comminuted, condylar fractures, especially for children younger than 12 years16.
The best surgical approach should be as easy as possible for the surgeon to perform, should be versatile, and should allow for good visualization of the fracture site, with a short procedural time and low rate of complications17. The surgical approaches for the treatment of condylar fractures may be either intraoral or extraoral. The intraoral approach, first described in 1925, confers a low risk for nerve injuries and no visible scars. However, it may be difficult to perform in cases of high fractures with medial deviation. Moreover, it requires the use of the endoscope and a longer surgical time compared with other approaches18. Several authors reported high rates of postoperative complications related to endoscopic reduction, such as incomplete fracture reduction, condylar reabsorption, and postoperative occlusal diseases19.
Most extraoral approaches have already been described, such as preauricular, submandibular, and retromandibular approaches. These extraoral procedures present higher risks for nerve damage and consequent cutaneous visible scars as compared to intraoral approaches20. In particular, the pre-auricular approach increases the risk for injury to the temporal and zygomatic branches of the facial temporal nerve, along with its inability to properly treat subcondylar fractures7. Moreover, it is associated with an increased risk for hematoma, sensory loss, and hypertrophic scars21. However, these extraoral approaches are not indicated for the treatment of all types of fractures. The pre-auricular approach is indicated for high fractures, as common submandibular and retromandibular approaches do not allow for the proper visualization of high fractures17.
The description of the approach used for the patients in this series differs from the classic description of the submandibular and retromandibular approaches5,17,22,23. Besides the size of the incision, which does not exceed 20 mm, the divulsion of deep tissues using hemostatic forceps, without making an incision but just bluntly dissecting the tissues, significantly reduces the occurrence of nerve injury and parotid complications (fistulas and Frey's syndrome). Moreover, it contributes to low patient morbidity, without hampering the proper treatment of the condylar fracture. In addition to considering the surgical approach, it is important to underline the anatomical repair of the posterior border of the mandibular condyle, which becomes an important parameter for optimal fracture reduction.
CONCLUSIONS
In light of recently published studies, the indication for surgical treatment and rigid fixation of extracapsular condylar fractures of the mandible becomes clearer in the case of large deviations or when the fracture is associated with other mandibular fractures and/or the middle third of the face. Complications due to the surgical approach implemented significantly influence the final outcome and may cause nerve injuries and/or sensory damage, unsightly scars, and ineffective reduction of the condylar fracture. Therefore, the miniretromandibular transparotid approach offers advantages and should be included as an option for the surgical treatment of extracapsular condylar fractures of the mandible.
REFERENCES
1. Biglioli F, Colletti G. Mini-retromandibular approach to condylar fractures. J Craniomaxillofac Surg. 2008;36(7):378-83.
2. Villarreal PM, Monje F, Junquera LM, Mateo J, Morillo AJ, González C. Mandibular condyle fractures: determinants of treatment and outcome. J Oral Maxillofac Surg. 2004;62(2):155-63.
3. Pereira MD, Marques A, Ishizuka M, Keira SM, Brenda E, Wolosker AB. Surgical treatment of the fractured and dislocated condylar process of the mandible. J Craniomaxillofac Surg. 1995;23(6):369-76.
4. Haug RH, Brandt MT. Closed reduction, open reduction, and endoscopic assistance: current thoughts on the management of mandibular condyle fractures. Plast Reconstr Surg. 2007;120(7 Suppl 2):90S-102S.
5. Tang W, Gao C, Long J, Lin Y, Wang H, Liu L, et al. Application of modified retromandibular approach indirectly from the anterior edge of the parotid gland in the surgical treatment of condylar fracture. J Oral Maxillofac Surg. 2009;67(3):552-8.
6. Trost O, Trouilloud P, Malka G. Open reduction and internal fixation of low subcondylar fractures of mandible through high cervical transmasseteric anteroparotid approach. J Oral Maxillofac Surg. 2009;67(11):2446-51.
7. Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983;41(2):89-98.
8. MacLennan WD. Fractures of the mandibular condylar process. Br J Oral Surg. 1969;7(1):31-9.
9. Lindahl L. Condylar fractures of the mandible. I. Classification and relation to age, occlusion, and concomitant injuries of teeth and teeth-supporting structures, and fractures of the mandibular body. Int J Oral Surg. 1977;6(1):12-21.
10. Hyde N, Manisali M, Aghabeigi B, Sneddon K, Newman L. The role of open reduction and internal fixation in unilateral fractures of the mandibular condyle: a prospective study. Br J Oral Maxillofac Surg. 2002;40(1):19-22.
11. Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006;34(7):421-32.
12. Rowe NL. Fractures of the facial skeleton in children. J Oral Surg. 1968;26(8):505-15.
13. Trost O, Abu El-Naaj I, Trouilloud P, Danino A, Malka G. High cervical transmasseteric anteroparotid approach for open reduction and internal fixation of condylar fracture. J Oral Maxillofac Surg. 2008;66(1):201-4.
14. Trost O, Kadlub N, Abu El-Naaj I, Danino A, Trouilloud P, Malka G. Surgical management of mandibular condylar fractures in adults in France, 2005. Rev Stomatol Chir Maxillofac. 2007;108(3):183-8.
15. Widmark G, Bågenholm T, Kahnberg KE, Lindahl L. Open reduction of subcondylar fractures. A study of functional rehabilitation. Int J Oral Maxillofac Surg. 1996;25(2):107-11.
16. Hovinga J, Boering G, Stegenga B. Long-term results of nonsurgical management of condylar fractures in children. Int J Oral Maxillofac Surg. 1999;28(6):429-40.
17. Biglioli F, Colletti G. Transmasseter approach to condylar fractures by mini-retromandibular access. J Oral Maxillofac Surg. 2009;67(11):2418-24.
18. Loukota RA. Endoscopically assisted reduction and fixation of condylar neck/base fractures: the learning curve. Br J Oral Maxillofac Surg. 2006;44(6):480-1.
19. Schneider M, Lauer G, Eckelt U. Surgical treatment of fractures of the mandibular condyle: a comparison of long-term results following different approaches - functional, axiographical, and radiological findings. J Craniomaxillofac Surg. 2007;35(3):151-60.
20. Kempers KG, Quinn PD, Silverstein K. Surgical approaches to mandibular condylar fractures: a review. J Craniomaxillofac Trauma. 1999;5(4):25-30.
21. Yang L, Patil PM. The retromandibular transparotid approach to mandibular subcondylar fractures. Int J Oral Maxillofac Surg. 2012;41(4):494-9.
22. Girotto R, Mancini P, Balercia P. The retromandibular transparotid approach: our clinical experience. J Craniomaxillofac Surg. 2012;40(1): 78-81.
23. Nicolai G, Lorè B, De Marinis L, Calabrese L. Combined surgical approach retromandibular and intraoral to subcondylar mandibular fractures. J Craniofac Surg. 2011;22(4):1354-7.
1. Associate Professor I of the Plastic Surgery Service, Hospital das Clínicas da Universidade Federal do Paraná (UFPR), Full Member of Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Plastic Surgeon of Hospital Erasto Gaertner and Craniomaxillofacial Surgeon of Hospital Universitário Cajuru, Curitiba, PR, Brazil
2. Craniomaxillofacial and Plastic Surgeon, Head of Face Surgery Service, Hospital Universitário Cajuru, Curitiba, PR, Brazil
3. Craniomaxillofacial and Plastic Surgeon, Associate Professor I and Head of Reconstructive and Plastic Surgery Service of the Hospital das Clínicas/ UFPR, Curitiba, PR, Brazil
Correspondence to:
Maria Cecília Closs Ono
Rua Rosa Kaint Nadolny, 190 - Ap. 701 - Campo Comprido
Curitiba, PR, Brazil - CEP 81200-525
E-mail: mccono@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 5/7/2012
Article accepted: 7/10/2012
This manuscript was submitted as partial requirement to achieve the Full Member grade of the SBCP.
This study was performed at the Facial Surgery Service of the Cajuru University Hospital of Curitiba, Curitiba, PR, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter