

Original Article - Year 2013 - Volume 28 - Issue 3
Mastopexy combined with augmentation: systematic use of Ribeiro's inferiorly-based flaps
Mastopexia com implantes: uso sistemático dos retalhos de base inferior de Ribeiro
ABSTRACT
INTRODUCTION: In the last few decades, mastopexy has been a much discussed topic among plastic surgery specialists. Mastopexy associated with augmentation improves breast projection and ptosis correction. However, several authors have reported a high incidence of complications; the most feared being the extrusion of the implants. The use of Ribeiro's inferiorly-based flaps can be a good alternative to increase the safety of the procedure.
METHODS: Twenty-five consecutive patients who underwent augmentation-associated mastopexy using the inverted-T technique and Ribeiro's type I and type III inferiorly-based flaps between 2008 and 2011 were analyzed. The cases were assessed with regard to patients' age, type of surgery, purpose of the surgery, simple or associated procedure, follow-up period, positioning of the implants, type of implants, type of flaps, rate of complications and rate of revision surgeries.
RESULTS: The mean age of the patients was 39.5 years; 92% of the surgeries were performed for cosmetic reasons; 72% of the surgeries were primary procedures and 80% were associated procedures. In 24% of the cases, the patients exhibited grade II ptosis and 76% exhibited grade III ptosis. The follow-up period ranged from 3 months to 48 months. Two patients (8%) exhibited slight distress at the junction of the inverted-T, which was resolved with conservative treatment. No complications, such as seroma, hematoma, necrosis of the nipple-areola complex, infection, or implant loss, were observed. Moreover, no revision surgeries due to unsatisfactory results were necessary.
CONCLUSION: The systematic use of Ribeiro's inferiorly-based flaps can help increase the safety of the procedure and yield good results.
Keywords: Mammaplasty. Breast implantation. Surgical flaps. Mammaplasty/methods. Breast/surgery.
RESUMO
INTRODUÇÃO: A mastopexia tem sido muito discutida entre os especialistas nas últimas décadas. Mastopexia associada a implantes possibilita melhorar a projeção mamária e a correção da ptose. Vários autores relatam grande incidência de complicações, sendo a mais temida a extrusão dos implantes. O uso dos retalhos de base inferior de Ribeiro pode ser uma boa alternativa para aumentar a segurança do procedimento.
MÉTODO: Foram analisados 25 casos consecutivos de mastopexia com implantes em T-invertido e uso de retalhos de base inferior de Ribeiro dos tipos I e III, operados entre 2008 e 2011. Os casos foram avaliados quanto a idade das pacientes, tipo de cirurgia, motivação, procedimento simples ou associado, tempo de seguimento, posição dos implantes, tipo de implante, tipo de retalho, e índice de complicações e de reoperações.
RESULTADOS: A média de idade das pacientes foi de 39,5 anos, 92% das cirurgias foram por motivação estética, 72% das cirurgias foram primárias e 80%, associadas. Em 24% dos casos, as pacientes apresentavam ptose grau II e em 76%, grau III. O período de seguimento variou de 3 meses a 48 meses. Duas (8%) pacientes apresentaram pequenos sofrimentos na junção do T-invertido, tratados de maneira conservadora. Não foram obervadas complicações como seromas, hematomas, necroses do complexo areolopapilar, infecções, perda dos implantes, tampouco foram necessárias reoperações por resultados insatisfatórios.
CONCLUSÕES: O uso sistemático dos retalhos de base inferior de Ribeiro pode auxiliar a aumentar a segurança do procedimento, permitindo a obtenção de bons resultados.
Palavras-chave: Mamoplastia. Implante mamário. Retalhos cirúrgicos. Mamoplastia/métodos. Mama/cirurgia.
In the past few decades, the topic of mastopexy has generated intense interest and debate among plastic surgery authors. The use of breast implants has increased the range of options that allow surgeons to achieve a more balanced relationship between breast skin and content1,2. Because of current aesthetic demands, the insertion of breast implants is increasingly frequent in plastic surgery3. Its use in mastopexy procedures is also frequent, with good acceptance and results in the treatment of breast changes after gestation, breast feeding, or significant weight loss4. Despite the technical improvements and pleasing aesthetic results, there are many reports of complications and proposals for treatment algorithms to minimize the need for surgical revisions and unfavorable results3-8.
At the end of the 1960s, Ribeiro developed the inferior-based flap technique for breast reduction, which has been widely accepted and used because it is effective and relatively simple to execute9. Since then, the technique has been applied in mammaplasty, including with some adaptations8.
The present study aims to present the author's experience in the use of type I and type III inferiorly-based glandular dermo-lipo flaps described by Ribeiro et al.9 as additional tissue coverage for the area corresponding to the intersection of the lower breast quadrants in mastopexy combined with augmentation for aesthetic or reconstructive purposes.
METHOD
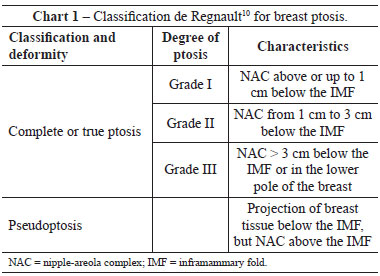
Thirty-eight consecutive patients who underwent one-stage mastopexy combined with augmentation between 2008 and 2011 were selected by reviewing medical records. Twenty-five patients with moderate to severe breast ptosis (grades II and III, according to Regnault's classification10 - Chart 1) treated with the inverted-T technique. The remaining patients were excluded from the study because they were treated with other mastopexy techniques (vertical or periareolar) that were not of interest to the study.
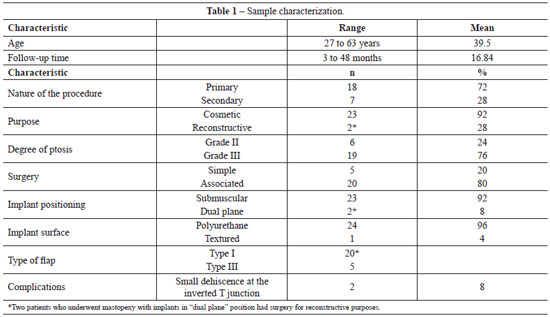
The following data were recorded: age, nature of the procedure (primary or secondary), reconstructive or aesthetic purpose of the surgery, degree of ptosis, simple or associated surgery, follow-up period, positioning of the implants, type of implant surface coating, type of flap, occurrence and type of complications, as well as occurrence of revision surgery (Table 1). Pre- and postoperative photos were compared to conduct a preliminary assessment of the aesthetic result.
Anatomy of Ribeiro's Flaps I and III
The type I flap has a rectangular shape, and its dimensions are approximately 9 cm in height, 6 cm in width and 3 cm in thickness. The flap receives blood supply via the perforating arteries of the 4th to 7th intercostal spaces, which are branches of the internal mammary artery; blood flow through the perforator branches of the 5th intercostal space is more constant9.
For its application in mastopexy combined with augmentation, a flap with a base and height of approximately 7 cm and thickness of 3 cm, respectively, was drawn. A base/height ratio of 1:2 was maintained to avoid trophic problems. Extension did not exceed 7 cm, because in our sample, the vertical portion of the scars had a maximum height of 6 cm. In a practical manner, we were able to correlate the distance between points B and C of the marking to the width of the base of the flap (Figures 1 and 2).
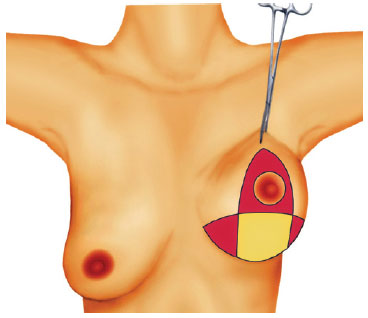
Figure 1 - Ribeiro's type I inferiorly-based flap.

Figure 2 - Ribeiro's type I inferiorly-based flap.
The type III flap has the shape of a triangle or parallelepiped; this flap is specified when the aim is to spare the maximum amount of breast tissue. The thickness of type III flap is similar to that of the type I flap (3 cm); its base usually follows the length of the horizontal portion of the inverted-T marking and extends upward as far as 2 cm to 3 cm below the nipple-areola complex (NAC), forming a triangle. Similarly to pedicle I, it receives blood supply from the perforator arteries of the 5th to 7th intercostal spaces. In addition, there is a random secondary blood supply from the subdermal plexus of its lower portion9 (Figures 3 to 5).
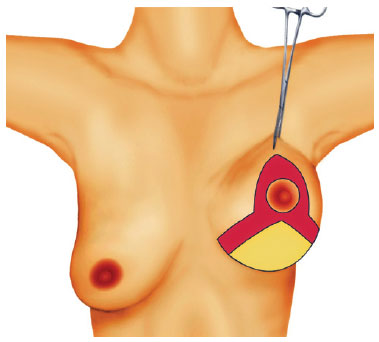
Figure 3 - Ribeiro's type III inferiorly-based flap.
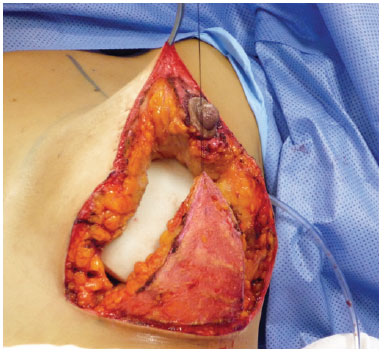
Figure 4 - Ribeiro's type III inferiorly-based flap.
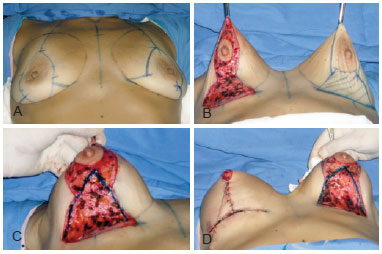
Figure 5 - Surgical sequence in a patient with major weight loss (approximately 40 kg) and Ribeiro's type III inferiorly-based flap.
However, we believe that in patients who underwent previous augmentation, the vascular pattern of the flaps was not according to that described by Ribeiro et al.9. After the pocket for the breast implants was prepared, the perforator vessels (branches of the internal mammary artery) were sectioned. We think that the flaps used in patients who underwent previous breast augmentation received blood supply via random autonomous vascularization of the subdermal plexus of the inframammary fold, perforator branches of the superior epigastric artery, or inferior intercostal perforator branches. In surgery secondary to augmentation mammaplasty, the inferiorly-based flap is the lower pole of the breast with the skin decorticated. For this reason, these flaps are less thick than are the type I and type III flaps described by Ribeiro et al.9; however, in this series, the geometric configuration described by these authors was maintained. Similar flaps have been described by other authors, particularly in cases of reconstructive surgery11.
Similarly to what occurred in cases without previous breast augmentation, a base/height ratio of 1:2 was maintained. The decorticated inferiorly-based flap was sutured to the pectoralis major muscle to provide extra coverage at the upper and lower poles; a "dual plane"12 type positioning of the flap was thus obtained (Figures 6 to 8).
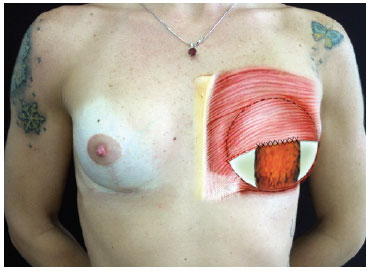
Figure 6 - Inferiorly-based flap decorticated for mastopexy after augmentation.

Figure 7 - Inferiorly-based flap of secondary surgery sutured to the pectoralis major muscle; implant positioned in "dual plane".
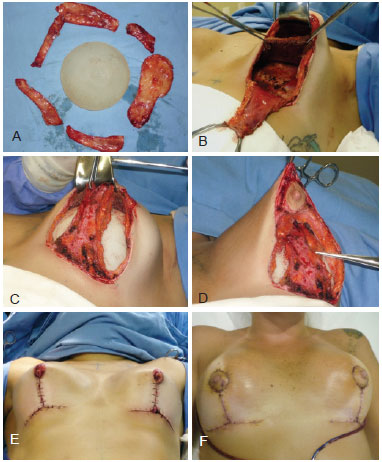
Figure 8 - Case of patient with history of previous breast augmentation, followed by mastopexy combined with augmentation and periareolar resection with insufficient result. She exhibited chronic seroma with a history of cutaneous fistula. Treated with inverted-T mastopexy combined with augmentation, repositioning in retromuscular pocket and decorticated inferiorly-based dermoglandular flap sutured to the pectoralis major muscle. In A, capsulectomia due to chronic seroma. In B, elevation of the pectoralis major muscle to pocket in dual plane. In C, suture of the decorticated inferiorly-based flap to the pectoralis major muscle. In D, detail of flap covering the positioned implant. In E, postoperative appearance of the breast mounting. In F, one-week evolution.
The described dimensions are not fixed; they can be adjusted according to the specific conditions of each case and to the need of breast tissue resection for an adequate relationship between breast skin and content.
Surgical Technique
The choice of the type of technique to be used (periareolar, vertical or inverted-T) should take into consideration the degree of ptosis exhibited by the patient on examination, which should be classified according to Regnault's classification10, and the assessment of skin asymmetries and sagging13. In our practice, cases of mild to moderate breast ptosis are treated using the technique of periareloar resection with the Benelli suture14 or with the diamond technique that results in a vertical scar9; in both cases, implants are inserted. These cases were not included in the present study. Patients with grade II and grade III ptosis were treated with the inverted-T technique, using type I and type III flaps of Ribeiro et al.9 combined with breat implants (Table 1).
Mastopexy with Simultaneous Augmentation: Inverted-T technique
With the patient under general anesthesia, in the semi-sitting position and with the arms in abduction relative to the body, the pocket area for implant insertion was marked according to the following limits: upper limit - the 2nd intercostal space; medial limit - a line 2 cm parallel to the midsternal line; lower limit - the inframammary fold; and lateral limit - the anterior axillary line. The areola was marked (4 cm in diameter) using a medium areola cutter and a line was drawn from the midpoint of the clavicle to the areola.
Next, the approximate marking parameters are described, as these measurements vary according to the anatomical references of each patient and the aim of the procedures, such as breast augmentation, reduction, and mastopexy. Point A is the point of greatest projection at the junction of the points determined according to the surgeon's judgment and by pinching the skin, at the level of the breast's meridian. This corresponds to transposing the position of the inframammary fold to the upper pole of the breast, as in the classical description by Pitanguy15. Point A is approximately 19 cm distant from the suprasternal notch. Points B and C correspond to the points where the skin is pinched; they determine point A. The distance between points B and C and point A is approximately 8 cm to 9 cm, and the distance between B and C is approximately 9 cm to 10 cm. Points D and E, which correspond to the 2 triangles of excess skin to be resected in the lower quadrants of the breast, were marked after points B and C were joined over the line of the inframammary fold. By joining points A, B, C, D, and E, a marking results which is similar to that obtained when the Pitanguy technique is used15 (Figure 9).
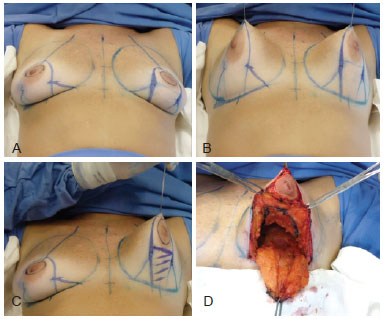
Figure 9 - Surgical sequence of mastopexy combined with augmentation and use of Ribeiro's type I inferiorly-based flap. In A to C, flap marking and outline. In D, "dome" resection. Resection reduces the weight of the gland on the implants, facilitating the involvement of implants by the upper pole.
Once the drawing of the technique was outlined, the dimensions of the flap that would serve as support between the lower portion of the implants and the vertical portion of the resulting scar were marked. The standard measurements of the type I flap were the following: 6 cm to 8 cm in width, upper extension 2 cm below the NAC, thickness of approximately 3 cm, height not exceeding 6 cm. These measurements ensure an adequate maximum base/height ratio of 1:2, which provides safe blood supply to the flap (Figure 9C). The type III flap has a triangular shape and its base runs along the entire horizontal portion of the inverted-T marking (Figure 5).
The procedure began with areola incision and the Schwartzman maneuver between points A, B, and C. Then, the skin was decorticated where the flap had been previously marked. Confection of the inferiorly-based flap began with the division of the breast into 2 hemispheres (upper and lower), perpendicular to the fascia of the pectoralis major muscle, to the Chassaignac lamina, to make the retroglandular pocket for the implants. Special care was taken regarding the inferior undermining to ensure that vascularization of the flap was not compromised, which could impede the procedure. The flap was released from the medial and lateral portions of the breast to the fascia of the pectoralis major muscle. Following the division of the breast into 2 hemispheres and the confection of the retroglandular pocket, the glandular adipose breast tissue was resected, starting with the lower lateral and medial segments of the breast that corresponded to the triangles formed by the joining of points B, D and C, E with the lateral portions of the pedicle and the demarcation of the inframammary fold. Routine semicircular resection on the upper hemisphere of the breast, called "dome resection", was performed, with a thickness of approximately 3 cm to ensure vascular nutrition of the NAC's flap. This resection reduced the weight of the breast's upper flap on the implants and allowed for a better adjustment of the tissues, thus yielding a more stable aesthetic appearance16 (Figure 9D).
The implants were positioned in the prepared pocket (retroglandular or retromuscular) and 3-0 nylon thread was used in the upper extremity of the inferiorly-based flap, which is repaired with hemostatic stitches. Points B and C were joined and fixed on the breast's midpoint in the inframammary fold, with the flap gently pulled towards the head by the repaired thread (Figure 10).
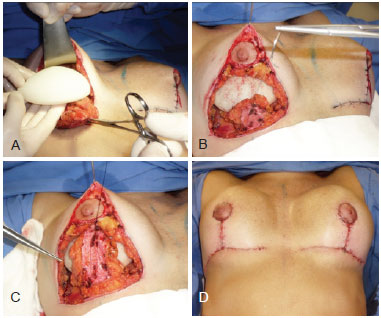
Figure 10 - In A, detail of the implants. In B and C, position of the flap relative to the implants. In D, final postoperative appearance.
When the implants were inserted in retromuscular pockets, the inferiorly-based flap was sutured to the pectoralis major muscle with 3-0 nylon stitches, after its release from the medial insertion in its lower third (Figure 8). At this point, the NAC was elevated and the inferior pedicle flap was fixed at the level of its widest vertical extension, without tension, to the pillars of the gland using a previously repaired thread (Figures 8C and 10C). Once the vertical portion of the flap was fixed, it was confirmed that the implants were completely covered and the attachment of the vertical portion via transposition of the lateral flaps over the inferior pedicle flap was concluded with sutures in 3 planes: simple nylon thread 3-0 stitches in the glandular plane, colorless nylon thread 4-0 in the subglandular plane, and intradermal suture with monofilament poliglecaprone thread 4-0 (Figures 8F and 10D).
During the immediate postoperative period, routine aspiration draining was performed in closed system for 24 to 48 h (time depends on drain output). Padded dressings were kept for 12 to 24 h and replaced with sterile micropore tape before hospital discharge. The tape was replaced after 5 to 7 days and maintained for 30 days.
RESULTS
Twenty-five women aged between 27 and 63 years (mean: 39.5 years) were included in the study. Twenty-three women (92%) underwent surgery for purely cosmetic reasons and 2 women (8%) for reconstructive reasons. Eighteen (72%) procedures were primary surgeries and 7 (28%) were secondary surgeries. The patients included in the present study had grades II (24%; n=6) and III (76%; n=19) ptosis, according to the classification by Regnault10.
Eighty percent of surgeries were associated with other procedures (n=20) and 20% (n=5) were simple surgeries, i.e., mastopexy with augmentation. The patients' follow-up time after the surgery ranged between 3 and 48 months. Regarding the implants, 96% (n=24) were coated with polyurethane foam and 4% (n=1) were textured implants. Regarding the positioning of the implants, 92% (n=23) were placed in a subglandular pocket and 8% (n=2) in a "dual plane" type pocket using Ribeiro's type I flap. Regarding the type of flap used, 80% (n=20) were type I and 20% (n=5) were type III.
Two (8%) patients exhibited a complication characterized by a small area of dehiscence at the junction of the vertical and horizontal portions of the inverted T, which was resolved with conservative treatment (Figure 11). There were no occurrences of NAC necrosis, seroma, hematoma, infection, or the need for implant removal or revision surgery due to insufficient results.
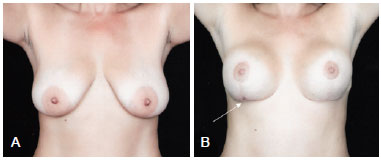
Figure 11 - In A, preoperative appearance of a patient who underwent insertion of a 235 ml polyurethane implant. The Ribeiro's type I inferiorly-based flap acts as a protection shield between the implant and the scar and increases the safety and coverage of the implants. In B, 6-months postoperative appearance, with an area of slight distress (arrow) at the junction between the vertical and the horizontal portions of the inverted-T scar, which was resolved with conservative treatment.
DISCUSSION
The use of breast implants combined with mastopexy is a reality in plastic surgery today1,2,5. It allows greater freedom to adjust the skin over the breast content and, as a consequence, yields satisfactory aesthetic results17 (Figures 12 and 13). The literature contains many descriptions of techniques to correct breast hypertrophy and ptosis15,18.
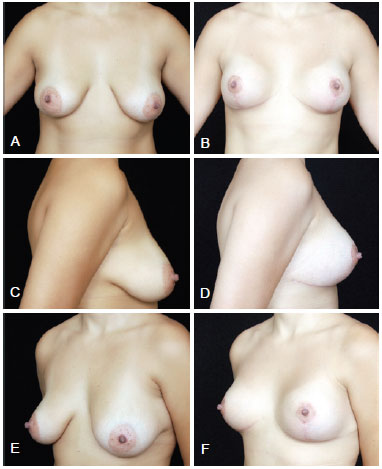
Figure 12 - Comparison of appearance of patient with postgestational breast ptosis, grades II and III according to Regnault, and asymetry. The patient underwent primary mastopexy combined with augmentation using 235 ml polyurethane implants, inverted-T technique, retroglandular positioning of the implants and Ribeiro's type I inferiorly-based flap. In A, C and E, preoperative appearance, in frontal view, right profile, and left oblique view, respectively. In B, D and F, postoperative appearance, in frontal view, right profile, and left oblique view, respectively.
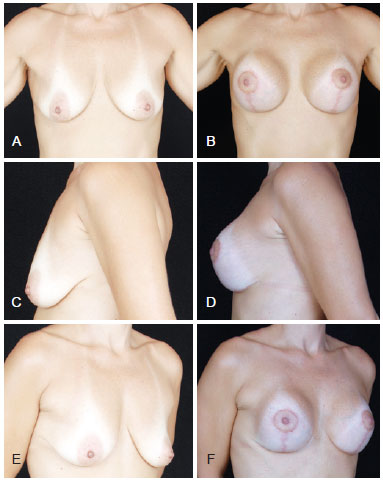
Figure 13 - Patient who underwent mastopexy combined with augmentation following major weight loss, using 215 ml polyurethane implants, retroglandular pocket and Ribeiro's type III inferiorly-based flap. In A, C and E, preoperative appearance, in frontal view, left profile, and right oblique view, respectively. In B, D and F, postoperative appearance, in frontal view, left profile, and right oblique view, respectively.
In 1980, Tanski19 described the use of an inferiorly-based adipose glandular flap combined with augmentation with silicone implants for the treatment of breast hypertrophy and ptosis or for prophylactic mastectomy cases. In 1989, Georgiade et al.20 described a technique based on a dermoglandular areolado flap with a pyramid shape, initially used in surgeries for the treatment of breast hypertrophy. Hammond et al.11, in 2002, and Nava et al.21, in 2006, described the use of deepithelized inferior flaps to cover silicone implants in immediate breast reconstructions, thus minimizing the risk of implant exposure following dehiscence at the junction of the vertical and horizontal lines of scars that result in an inverted-T.
In Brazil, Ribeiro developed, already in 1969, the technique of the inferiorly-based flap for breast reduction, which was presented at the Congresso da Regional da Guanabara da Sociedade Brasileira de Cirurgia Plástica in 1971 and, later, internationally at the XII Congresso Latino-Americano, in São Paulo, and at the Congresso da International Society of Aesthetic Plastic Surgery (ISAPS), in Rio de Janeiro, in 1972. It was first published in the Revista Espanhola de Cirurgia Plástica, in 1973, describing the use of an inferiorly-based dermo-lipo flap as an alternative to excessive resection of breast tissue in the application of the Pitanguy technique when the keel resection is used, which he initially called "pedículo de seguridad". Following the observation of more stable results with the use of the safety pedicle, he applied it in other breast surgery techniques, both in cosmetic and reconstructive surgery, which led him to classify the flaps into 5 subtypes9. Ribeiro's inferiorly-based flaps technique is an important contribution to breast plastic surgery and is widely accepted and established today because it is effective, relatively simple to execute, and versatile.
In our practice, Ribeiro's inferiorly-based type I and type III flaps in mastopexy combined with augmentation for cosmetic purposes is used to provide adequate coverage with vascularized tissue in the area where the vertical portion of the scars that result from the inverted-T technique is projected.
Various authors have reported their reluctance regarding mastopexy combined with augmentation because of the high rate of complications described in studies. These complications range from small suture dehiscence to the need for revision surgery to adjust excess skin, hypocorrection or ptosis recurrence, and asymmetries, among others. However, implant loss is the most feared complication 3,5,6,22. Moreover, there are reports showing concern regarding the reliability of tissue coverage over the implants3. The indication to place the implants in a retromuscular pocket is frequent; however, the lower portion of the implants is insufficiently covered. The use of inferiorly-based decorticated flaps to prevent or treat the insufficiency of tissue over the implants has been described in reconstructive oncoplastic surgery, cases of major weight loss, and cosmetic surgery11,13,19,21,22. Following breast tissue resection during mastopexy, the implants become more vulnerable and very close to the line of suture; this is a frequent postoperative complaint. The weight of the implants, in particular on the vertical line of the scar, at the point where it joins the areola and the inverted-T, can lead to implant exposure and loss. One advantage of the inferiorly-based flap is that it contains the implants, thus avoiding excessive movement over the horizontal portion of the scar and reducing the risk of it becoming palpable or visible16,22. According to our experience, this fact provides grounds for the routine use of Ribeiro's type I and type III flaps, which provide adequate implant coverage.
The data obtained from our sample are in line with the principal studies published in the literature. In this series, we observed 67.8% of mastopexy procedures using the inverted-T technique, a result that is similar to that described by Stevens et al.17. The overall rate of complications in this sample was 8%, including small scar problems in the vertical portion of the scar and at the inverted-T junction. In this series of cases, there were no cases of implant loss due to exposure and no implant-related complications were observed.
We have been routinely using implants coated with polyurethane foam in augmentation mammaplasties since 2003. For mastopexy combined with augmentation, we opted for round implants with medium projection and a polyurethanecoated surface; however, in this study, 1 (4%) of the patients demanded to receive an implant with a textured surface. In this patient, there was early implant movement, compared to the cases in which implants coated with polyurethane foam were used. Although we considered this result as suboptimal, the patient was satisfied and did not wish to undergo revision surgery (Figure 14). The described rate of revision surgery is 10.9% for implant-related problems and 3.7%, for problems related to ptosis recurrence or permanence17.
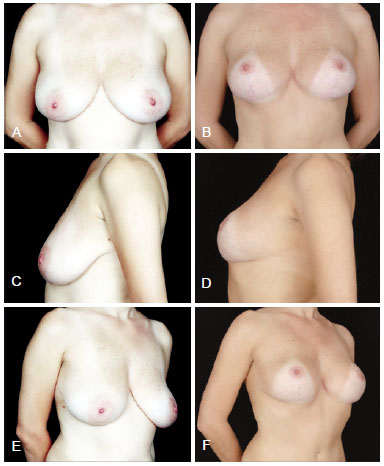
Figure 14 - Primary mastopexy with textured surface 230 ml implants. Note the emptying of the upper pole, with movement of the implants over the lower pole. Although we did not consider this result ideal, the patient was satisfied and did not want to undergo revision surgery. In A, C and E, preoperative appearance, in frontal view, left profile, and right oblique view, respectively. In B, D and F, postoperative appearance after 36 months, in frontal view, left profile, and right oblique view, respectively.
In patients who underwent previous breast augmentation, the process of peri-implant tissue atrophy, the insufficient tissue coverage, the additional weight of the new implant, and the tension exerted on the vertical portion of the scar can lead to implant exposure if slight distresses or suture dehiscence occur11,21 (Figure 15).
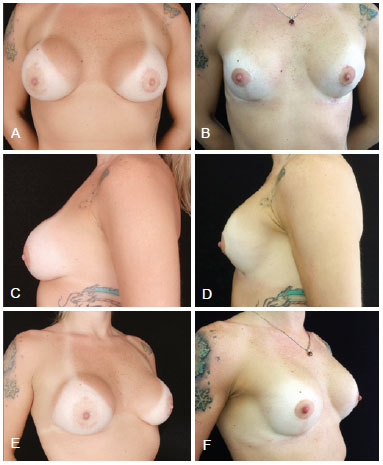
Figure 15 - Patient with a history of 2 previous mastopexies with periareolar resection due to unsatisfactory results. Right breast exhibited chronic seroma and cutaneous fistula. The patient underwent 305 ml polyurethane implant placement in retromuscular position, with decorticated inferiorly-based flap sutured to the pectoralis major muscle, "dual plane" pocket. In A, C and E, preoperative appearance, in frontal view, left profile, and right oblique view, respectively. In B, D and F, postoperative appearance after 2 years, in frontal view, left profile, and right oblique view, respectively.
Inspired by the versatility of Ribeiro's inferiorly-based pedicles, we started applying an inferiorly-based dermo-lipo pedicle as a "protection shield" to the most vulnerable area of the breast implants when the mastopexy inverted-T technique is applied in combination with augmentation.
CONCLUSION
Mastopexy combined with augmentation is a treatment modality that can be viewed as a good alternative treatment of breast ptosis cases, as it yields satisfactory results. Although the sample used in this study was small, the systematic use of Ribeiros's inferiorly-based flaps (type I and type III) in mastopexy combined with augmentation is a relatively simple technique to execute that allows for reliable implant coverage at the junction of the lower quadrants when vertical and inverted-T techniques are used. The application of the method described herein may help prevent the occurrence of complications on the most vulnerable area during mastopexy combined with augmentation, which is the point of convergence of the inverted-T portions.
REFERENCES
1. Gonzalez-Ulloa M. Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg Transplant Bull. 1960;25:15-26.
2. Regnault P. The hypoplastic and ptotic breast: a combined operation with prosthetic augmentation. Plast Reconstr Surg. 1966;37(1):31-7.
3. Handel N. Secondary mastopexy in the augmented patient: a recipe for disaster. Plast Reconstr Surg. 2006;118(7 Suppl):152S-63S.
4. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67.
5. Spear SL, Boehmler JH 4th, Clemens MW. Augmentation/mastopexy: a 3-year review of a single surgeon's practice. Plast Reconstr Surg. 2006;118 (7 Suppl):136S-47S.
6. Spear SL. Augmentation/mastopexy: "surgeon, beware". Plast Reconstr Surg. 2006;118(7 Suppl):133S-4S.
7. Karnes J, Morrison W, Salisbury M, Schaeferle M, Beckham P, Ersek RA. Simultaneous breast augmentation and lift. Aesthetic Plast Surg. 2000;24(2):148-54.
8. Camara O, Egbe A, Koch I, Herrmann J, Gajda M, Baltzer P, et al. Surgical management of multiple bilateral fibroadenoma of the breast: the Ribeiro technique modified by Rezai. Anticancer Res. 2009;29(7):2823-6.
9. Ribeiro L, Accorsi A Jr, Buss A, Marcal-Pessoa M. Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Reconstr Surg. 2002;110(3):960-70.
10. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
11. Hammond DC, Capraro PA, Ozolins EB, Arnold JF. Use of a skin-sparing reduction pattern to create a combination skin-muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg. 2002;110(1):206-11.
12. Tebbetts JB. Dual plane breast augmentation: optimizing implant-softtissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107(5):1255-72.
13. Don Parsa F, Brickman M, Parsa AA. Augmentation/mastopexy. Plast Reconstr Surg. 2005;115(5):1428-9.
14. Benelli L. A new periareolar mammaplasty: the "round block" technique. Aesthetic Plast Surg. 1990;14(2):93-100.
15. Pitanguy I. Mammaplasty. Study of 245 consecutive cases and presentation of a personal technic. Rev Bras Cir. 1961;42:201-20.
16. Mansur JR, Bozola AR. Mastopexy and breast augmentation with protection and inferior support of the prosthesis with inferior pedicle flap. Rev Bras Cir Plást. 2009;24(3):304-9.
17. Stevens WG, Freeman ME, Stoker DA, Quardt SM, Cohen R, Hirsch EM. One-stage mastopexy with breast augmentation: a review of 321 patients. Plast Reconstr Surg. 2007;120(6):1674-9.
18. Pontes R. Reduction mammaplasty: variations I and II. Ann Plast Surg. 1981;6(6):437-47.
19. Tanski EV. A new method for prophylactic mastectomy, reduction mammaplasty, and mastopexy. Plast Reconstr Surg. 1980;65(3):314-22.
20. Georgiade GS, Riefkohl RE, Georgiade NG. The inferior dermal-pyramidal type breast reduction: long-term evaluation. Ann Plast Surg. 1989;23(3):203-11.
21. Nava MB, Cortinovis U, Ottolenghi J, Riggio E, Pennati A, Catanuto G, et al. Skin-reducing mastectomy. Plast Reconstr Surg. 2006;118(3):603-10.
22. Garcia EB, Fusaro Neto R, Arruda RF, Pereira JB, Ferreira LM. Inferior pedicle breast flap for submuscular implant coverage in mammaplasty after massive weight loss. Plast Reconstr Surg. 2010;125(2):74e-75e.
1. Plastic Surgeon, Master of the Postgraduate Program in Medicine/Surgical Sciences at the Faculdade de Medicina da Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil; Full Member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Niterói, RJ, Brazil
2. Plastic Surgeon, Full Member of the SBCP, Rio de Janeiro, RJ, Brazil
3. Plastic Surgeon, Emeritus Full Member of the SBCP, Rio de Janeiro, RJ, Brazil
4. Associate Professor of the Postgraduate Program in Medicine/Surgical Sciences at the UFRGS, Porto Alegre, RS, Brazil
Correspondence to:
Marcelo Castro Marçal Pessoa
Av. Almirante Ari Parreiras, 655 - 1008 - Vital Brasil
Niterói, RJ, Brazil - CEP 24230-321
E-mail: pessoamcm@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: May 27, 2012
Article accepted: December 2, 2012
Study conducted at the author's private practice, Niterói, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter