

Original Article - Year 2013 - Volume 28 -
Use of mid-forehead flap in nasal reconstruction
Uso do retalho médio-frontal na reconstrução do nariz
ABSTRACT
BACKGROUND: Six hundred years before Christ, the mid-forehead flap was described by the Indian Sushruta Samhita. Until today, this flap called "Indian flap", has a major role in the reconstruction of the nose. The aim of this work was to analyze the results of the 38th Infirmary of the Santa Casa da Misericórdia of Rio de Janeiro, Professor Ivo Pitanguy's Service, in nasal reconstruction with the mid-forehead flap.
METHODS: We did a retrospective study of 10 cases operated in the service for nasal reconstruction with Indian flap, during a 21 year period (1991-2012).
RESULTS: The number of nasal sub-units affected varied from 4 to 9, with an average of 6.5 subunits. In 70% of the patients, was performed a previous expansion of the mid-forehead flap and in 90% were used cartilage grafts and/or bones. Five patients had postoperative distortions, that were corrected with other surgeries. No cases of infection, necrosis of the flap or graft extrusion were recorded.
CONCLUSIONS: This study allowed to demonstrate that the mid-forehead flap still have an important role in nasal reconstruction of major defects, showing satisfactory results due to its vascular safety, the amount of skin which is obtained, likeness of color, texture and skin thickness.
Keywords: Reconstructive surgical procedures. Nose/surgery. Surgical flap. Forehead/surgery. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: Seiscentos anos antes de Cristo, foi descrito o retalho médio-frontal pelo indiano Sushruta Samhita. Até hoje, esse retalho, chamado "retalho indiano", é usado na reconstrução do nariz. O objetivo deste trabalho foi analisar os resultados da 38ª Enfermaria da Santa Casa da Misericórdia do Rio de Janeiro, Serviço do Professor Ivo Pitanguy, na reconstrução nasal com emprego de retalho médio-frontal.
MÉTODO: Foi realizado estudo retrospectivo com 10 casos operados no serviço referido para reconstrução nasal com retalho indiano, no período de 21 anos (1991 a 2012).
RESULTADOS: O número de subunidades nasais atingidas variou de 4 a 9, com média de 6,5 subunidades. Em 70% dos pacientes foi realizada expansão prévia do retalho médio-frontal e em 90% foram utilizados enxertos cartilaginosos e/ou ósseos. Cinco pacientes apresentaram distorções pós-operatórias, que foram corrigidas por outras cirurgias. Nenhum caso de infecção pós-operatória, de necrose do retalho ou de extrusão de enxertos foi registrado.
CONCLUSÕES: Este trabalho permitiu demonstrar que o retalho médio-frontal tem ainda importante papel na reconstrução nasal de grandes defeitos, com resultados satisfatórios, atribuídos a sua segurança vascular, à quantidade de pele que se obtém, e à semelhança de cor, textura e espessura cutâneas.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos. Nariz/cirurgia. Retalhos cirúrgicos. Testa/cirurgia. Cirurgia plástica/métodos.
Breasts with inferior pole hypoplasia have a disharmonious appearance due to a high inframammary fold and the prevalence of glandular volume in the upper quadrants that results in a lower inclination of the nipple-areola complex (NAC)1-6.
Von Heimburg et al.2 classified deformities of the base of the breast into four different types:
Breasts presenting with inferior pole hypoplasia, regardless of von Heimburg classification types I, II, or III, are not tuberous, although they share several treatment difficulties. Moreover, patients with deformities of the base of the breast often exhibit mammary asymmetry as well, which renders the treatment even more complex.Type I - only the lower-medial quadrant of the breast is deficient; Type II - the presence of deficiencies in both inferior quadrants of the breast but no skin deficiency within the subareolar region; Type III - deficiencies in both inferior quadrants of the breast and one or more subareolar skin deficiencies; and Type IV - deficiencies within all four quadrants of the breast (tuberous breast).
The available methods for the treatment of breast inferior pole hypoplasia typically include mastopexia, which implies the use of implants and an extensive scar burden, and periareolar, associated with a lower vertical or "inverted T" type3. In these cases, the goal is to correct the disharmonious shape of the breasts and the possible asymmetries using minimal or inconspicuous scars. Taking this into account, some patients may benefit from techniques that use rotated internal flaps to reshape the breast and reposition the inframammary fold, a result achieved using only the scars where the implants would then be positioned as routes for surgical access as described in this case series.
METHODS
This study presents a series of four patients who underwent correction of breast inferior pole hypoplasia between 2010 and 2011. The patients underwent the following:
Design and planning of the incisions - with the patient standing, an ideal inframammary fold was delineated, and sometimes, the fold was delineated to > 5 cm below the pre-existing inframammary fold. During the procedure, the incision along the ideal inframammary fold had sufficient extension. In the cases reported in this study, we chose incisions approximately 6 cm long; Dissection - beginning in the subglandular plane and continuing until above the NAC projection. In the upper portion of the mammary gland, a breast tissue flap was prepared (Figure 1A) to be positioned with the inferior base parallel to the skin and was then rotated 180º inferiorly (Figure 1B);
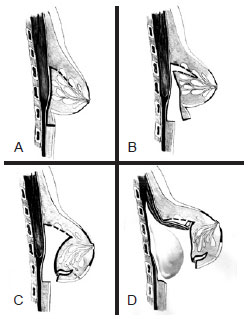
Figure 1 - Schematic drawing of the procedure used to correct breast inferior pole hypoplasia. In A, incisions of the inframammary fold and initial dissection of the subglandular plane. In B, internal flap dissection. In C, rotation of the extremities of the flap inferiorly and fixation next the edge of the surgical wound. This rotation promotes filling of the inferior breast pole and pushing of the skin from the inside to the outside to cause the disappearance of the pre-existing inframammary fold. In D, dissection of the submuscular plane for the insertion of breast implants in the dual plane. Prior to the implant insertion, the edge of the pectoral muscle was re-sutured to the breast using 3-0 monocryl thread.
Fixation of the flap - the upper extremity of the flap to the upper edge of the surgical wound was sutured with 3-0 monofilament nylon threads. This promotes filling of the inferior breast pole and pushing of the skin from the inside to the outside to cause disappearance of the pre-existing inframammary fold (Figure 1C). This step also ensures that, after surgery, the new inframammary fold would be positioned adjacent to the surgical wound; Double plane dissection and implant insertion - the plane below the pectoral muscle was dissected for breast implant insertion according to the double plane procedure. Subglandular dissection was vertically extensive owing to preparation of the flap, and it extended above the NAC. For this reason, it was considered necessary to re-suture the edge of the pectoral muscle to the breast using 3-0 monocryl threads prior to implant insertion (Figure 1D); and Closing - suturing by planes using 3-0 monocryl threads was performed, and the skin was closed using intradermal sutures.
RESULTS
The procedure described here was used in four patients aged 19-27 years with breast inferior pole hypoplasia. In all cases, we used texture-coated, cohesive, and high-profile silicone implants with volumes of 225-325 cc.
No complications were observed in the postoperative period. The longer followed up was of 2 years.
Figures 2 to 5 illustrate the results obtained in the four cases. The breast deformities were corrected, and the inframammary fold was appropriately repositioned without any irregularities in the inferior breast contour.
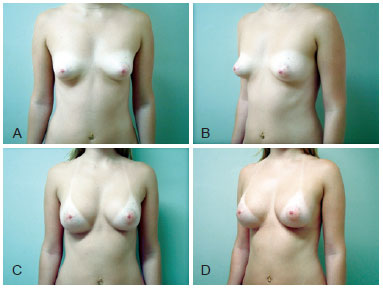
Figure 2 - Case 1. A 25-year-old patient. In A and B, frontal and left preoperative profile, respectively. In C and D, 1-year and 10-month frontal and left postoperative profile, respectively. We used textured, cohesive gel and 250 cc high-profile silicone implants.
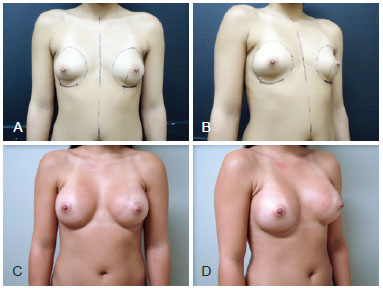
Figure 3 - Case 2. A 27-year-old patient. In A and B, frontal and right preoperative profile, respectively, showing mammary asymmetry. In the right profile view, observe the detailed demarcation below the pre-existing inframammary fold. In C and D, 1 year and 6 month frontal and right postoperative profile, respectively. We used textured, cohesive gel and 325 cc (right) and 300 cc (left) high-profile silicone implants.

Figure 4 - Case 3. A 22-year-old patient. In A and B, frontal and right preoperative profile, respectively. In C and D, 3-month frontal and right postoperative profile, respectively. We used textured, cohesive gel and 225 cc high-profile silicone implants.
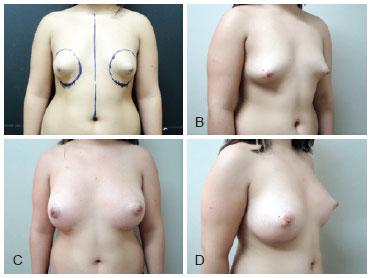
Figure 5 - Case 4. A 19-year-old patient. In A and B, frontal and right preoperative profile, respectively. In the frontal view, observe the detailed demarcation below the pre-existing inframammary fold. In C and D, 1-week frontal and right postoperative profile, respectively. We used textured, cohesive gel and 275 cc3 high-profile silicone implants.
DISCUSSION
The procedure used in this case series closely resembled the technique described by Oroz e al.1 in 2005 in which internal breast flaps were used to reconstitute the volume of the inferior breast pole and reposition the inframammary fold. The flaps were dissected starting from the same incision through which the implants were inserted. This is the main (or only) difference between the procedure described by Oroz et al.1 and the technique used in this study.
The procedure described in the study by Oroz et al.1 used a lower periareolar incision, whereas the route for surgical access in this series was through the inframammary fold. Otherwise, the approach within the breast and the dissection of the flap are identical.
The procedure described herein is an option for the treatment of breast inferior pole hypoplasia, as scars are significantly reduced compared to those of conventional mastopexy. Moreover, it is possible to correct deformities, increase breast volume, and safely achieve a new and proper inframammary fold position without causing any irregularities in the inferior breast contour.
The cases presented here evolved positively. The patients were satisfied with the result, and thus far, no complications have been observed in the postoperative period.
CONCLUSIONS
Despite the small sample size and limited follow-up period, the results obtained here suggest that the proposed procedure is a suitable alternative for the treatment of selected cases of breast deformities and inferior pole hypoplasia.
REFERENCES
1. Oroz J, Pelay MJ, Escudero FJ. Reconstruction of the tuberous breast. An Sist Sanit Navar. 2005;28 Suppl 2:101-8.
2. von Heimburg D, Exner K, Kruft S, Lemperle G. The tuberous breast deformity: classification and treatment. Br J Plast Surg. 1996;49(6):339-45.
3. Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas D, Lambrinaki N, Ioannidou-Mouzaka L. Aesthetic reconstruction of the tuberous breast deformity. Plast Reconstr Surg. 2003;112(4):1099-108.
4. Costa SS, Blotta RM. Assimetrias da mama. Rio de Janeiro: Revinter; 2007.
5. Ribeiro L, Canzi W, Buss A Jr, Accorsi A Jr. Tuberous breast: a new approach. Plast Reconstr Surg.1998;101(1):42-50.
6. Ribeiro L, Accorsi A Jr, Buss A, Pessĵa MC. Short scar correction of the tuberous breast. Clin Plast Surg. 2002;29(3):423-31.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Master in Medicine-Surgery by the Universidade Federal do Rio Grande do Sul (Federal University of Rio Grande do Su), preceptor of the Medical Residence of the Plastic Surgery Service of Hospital Cristo Redentor (Cristo Redentor Hospital), Porto Alegre, RS, Brazil
2. Plastic surgeon, associated member of SBCP, staff of the Plastic Surgery Service of Hospital Cristo Redentor (Cristo Redentor Hospital), Porto Alegre, RS, Brazil
3. Aspirant member of SBCP, medical resident of the Plastic Surgery Service of Hospital Cristo Redentor (Cristo Redentor Hospital), Porto Alegre, RS, Brazil
Correspondence to:
Victor Vieira Orsi
Rua Itaboraí, 840/703 - Bairro Jardim Botânico
Porto Alegre, RS, Brazil - CEP 90670-030
E-mail: victor.orsi@brturbo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 18, 2013
Article accepted: May 10, 2013
This study was performed at the Hospital Cristo Redentor - Grupo Hospitalar Conceição (Cristo Redentor Hospital - Conceição Hospital Group), Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter