

Ideas and Innovation - Year 2013 - Volume 28 -
Modified zigzag periareolar incision: alternative technique for augmentation mammaplasty
Incisão periareolar em zigue-zague modificada: técnica alternativa para mastoplastia de aumento
ABSTRACT
Augmentation mammaplasty is one of the most common surgeries worldwide. Variables such as implant size and location as well as incision type influence the final result. The periareolar approach is well known and disseminated; however, the resulting scar is a common reason for patient dissatisfaction. We present a modified periareolar technique using a zigzag incision that results in invisible scars after augmentation mammaplasty. The technique described here is an excellent alternative for augmentation mammaplasty and has an esthetic satisfactory result with imperceptible scars in the periareolar skin of the nipple-areola complex, which is naturally irregular.
Keywords: Mammaplasty. Breast implantation. Cicatrix.
RESUMO
Mastoplastia de aumento é uma das cirurgias mais realizadas em todo o mundo. Variáveis como tamanho e localização do implante, bem como o tipo de incisão, influenciam o resultado final. A abordagem periareolar é bem conhecida e difundida, porém sua cicatriz pode, muitas vezes, ser motivo de insatisfação da paciente. Uma modificação da técnica periareolar é apresentada, com incisão em zigue-zague, para mamoplastias de aumento, permitindo a obtenção de cicatrizes imperceptíveis. A técnica descrita é uma excelente alternativa para mastoplastia de aumento, proporcionando resultado estético satisfatório, com cicatriz camuflada na transição da pele periareolar com o complexo areolopapilar, que é naturalmente irregular.
Palavras-chave: Mamoplastia. Implantes mamários. Cicatriz.
Augmentation mammaplasty may be performed using different surgical approaches. Determination of the incision site as well as the location, size, form, and texture of the implant is important. All these variables contribute to the final procedural result1.
Since the advent of augmentation mammaplasty through intramammary incision using cohesive silicone gel implants2, many surgical approaches have been extensively described3-5. The most popular are the intramammary, periareolar, and axillary incisions, whereas the periumbilical and transareolar incisions are the least used approaches. All these techniques have their advantages and disadvantages6-8.
The intramammary incision allows direct access to the pocket plane and results in a very short scar (4-5 cm) positioned within the inframammary fold. This access technique is most commonly used by Brazilian plastic surgeons. The axillary incision is preferred by various authors with the aim of avoiding mammary scars. It can be conducted under direct view or with the aid of an endoscope, and the resulting S-shaped scar measures 3-4 cm.
Areolar incisions may have distinct forms. The lower periareolar incision is mainly used when it is necessary to remove mammary nodes or upon patient request. The geometric scar principle has been described for periareolar incisions and provides excellent results3,9. The aim of the present article is to present an alternative approach for augmentation mammaplasty using a periareolar approach with a zigzag incision.
SURGICAL TECHNIQUE
Preoperative markings were performed with the patient in the orthostatic position. The area of interest was marked to construct the implant pocket, leaving approximately 1.5 cm of the midline for medial undermining with the aim of avoiding symmastia. The geometric periareolar zigzag incision was carefully made in the inferior semicircle of the areola to ensure that the marks did not extend into the skin adjacent to the nipple-areola complex.
The smaller the geometric forms, the more imperceptible is the scar, so we chose to use a triangle base of approximately 0.5 cm. Another important aspect of the marking is the end part of the zigzag incision, in the three o'clock and nine o'clock positions, turned to the nipple-areola complex, to prevent possible damage to the skin around the areola during the displacement procedure to insert the implant (Figure 1). Therefore, any possible accidental extensions of the incision because of the displacement are restricted to the skin of the areola and are easier to conceal.
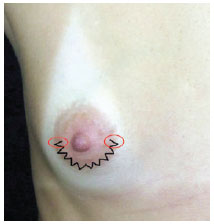
Figure 1 - Schematic drawing of the zigzag marking. Note that the marking is restricted to the skin of the areola and does not extend to the periareolar skin. Details of the marking end, turned to the center of the nipple-areola complex to avoid possible unaesthetic scars in an eventual case of inadvertent extensions of the incision during displacement to insert the implant.
After the skin infiltration was prepared with bupivacaine and adrenaline, an incision was made in the dermis and subcutaneous tissue. In the subcutaneous cellular and glandular tissues, an upper oblique incision was made until the pectoralis major fascia was reached at the level of the areola. At that point, the implant plane was dissected according to the surgeon's preference. After adequate hemostasis and implant placement, the incision was closed by planes. The peaks and depressions of the zigzag line in each side were closed with Gilles stitches using mononylon 5.0.
DISCUSSION
The zigzag approach was conducted for all patients with an indication for periareolar augmentation mammaplasty in the Plastic Surgery Service of the Hospital de Clínicas da Universidade Federal do Paraná (Clinic's Hospital of the Federal University of Paraná). In our cases, we did not observe postoperative complications such as healing delay, hypertrophic scars, or pigmentation alterations. Similarly, no cases of capsular contracture or complaints regarding the loss of sensitivity of the nipple-areola complex were found during the postoperative follow-up period.
It is important to mention some of the basic principles associated with the cicatrization process. In some cases, unaesthetic scars may develop despite the efforts made to optimize wound cicatrization. Wound cicatrization is a dynamic process that involves numerous transformations before reaching a stationary stage at around 1 year after the tissue lesion. The ideal scar should be thin and even and located inside or parallel with the lines of skin tension, while the surrounding skin should have a good corresponding color. These characteristics result in a less visible scar. Therefore, techniques that break or prevent an irregular scar line provide a greater degree of scar concealment1. Especially in the areola, which has varied color shades, a scar showing good progression turns out to be imperceptible.
Although the current tendency in mammaplasty is scar reduction, including breast reduction with a vertical scar and minimal incisions in mastopexies4,10, the quality of those incisions should not be underestimated. The incision quality should decrease the signs indicative of surgery. Better incision quality helps a patient easily accept the surgical result11.
According to Gryskiewicz & Hatfield3, this method creates a scar that imitates the naturally irregular shape of the areola and periareolar skin. They observed a delay in cicatrization among four patients and the presence of a hypertrophic scar in two patients. Carvajal & Echeverry12 described a modified approach of the semicircular periareolar incision technique, the zigzag incision, to insert mammary implants in patients with a small nipple-areola diameter.
To date, the techniques described for the semicircular zigzag incision recommend that the incision be made in the periareolar skin-areola junction. When this type of approach is used, a more apparent cicatrization pattern is seen in the skin adjacent to the nipple-areola complex, which justifies the incision only in the lower end of the skin of the areola without extension into the region of transition between the two. This modification has afforded higher satisfying results, and almost imperceptible scars (Figures 2 and 3).
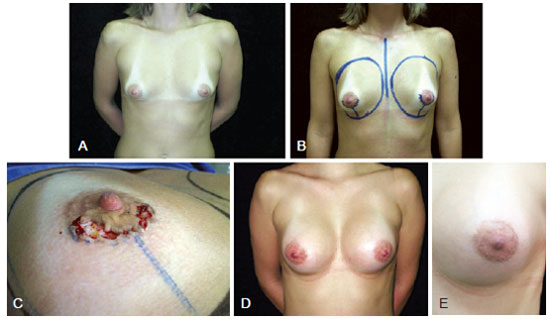
Figure 2 - In A, presurgical appearance. In B, presurgical marking. In C, details of the incision during surgery. In D, appearance 40 days after augmentation mammaplasty with periareolar zigzag incision, with a textured anatomical implant (255 cc). In E, details of the zigzag periareolar scar.
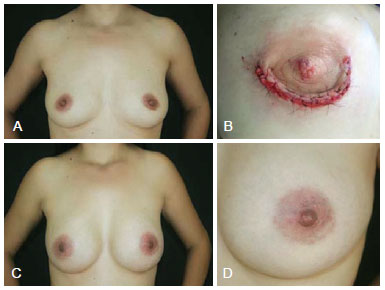
Figure 3 - In A, presurgical appearance. In B, details of closing the zigzag incision during the immediate postoperative period. In C, appearance 2 years after augmentation mammaplasty with periareolar zigzag incision with a round, high profile, 250-cc implant. In D, details of the scar 2 years after surgery.
This technique may be particularly useful for augmentation mammaplasty; however, we have also used the zigzag incision for the treatment of gynecomastia, with excellent results. The aim of the technique is to obtain an irregular scar that seems more natural.
The described technique is an excellent alternative for augmentation mammaplasty, providing a satisfactory esthetic result consisting of an imperceptible scar in the naturally irregular transitional area of the periareolar skin to the nipple-areola complex. This technique is safe and easy to perform, presents satisfactory results, and results in imperceptible scars.
REFERENCES
1. Tenius FP, Silva Freitas R, Closs Ono MC. Transareolar incision with geometric broken line for breast augmentation: a novel approach. Aesthetic Plast Surg. 2008;32(3):546-8.
2. Cronin TD, Gerow FJ. Augmentation mammaplasty: a new "natural feel" prosthesis. Transactions of the Third International Congress of Plastic Surgery; 1963 Oct 13-18; Amsterdam, The Netherlands. Excerpta Medica; 1963. p. 41-9.
3. Gryskiewicz JM, Hatfield AS. "Zigzag" wavy-line periareolar incision. Plast Reconstr Surg. 2002;110(7):1778-83.
4. Graf R, Biggs TM, Steely RL. Breast shape: a technique for better upper pole fullness. Aesthetic Plast Surg. 2000;24(5):348-52.
5. Bosch G, Jacobo O. The double pocket technique: aesthetic breast augmentation. Aesthetic Plast Surg. 2002;26(6):461-4.
6. Lai YL, Weng CJ, Chen YR, Noordhoff MS. Circumniple-incision, longitudinal-breast dissection augmentation mammaplasty. Aesthetic Plast Surg. 2001;25(3):194-7.
7. Pitanguy I. Transareolar incision for augmentation mammaplasty. Aesthetic Plast Surg. 1978;2:363-72.
8. Tebbetts JB. Alternatives and trade-offs in breast augmentation. Clin Plast Surg. 2001;28(3):481-500.
9. Candiani P, Campiglio GL. Augmentation mammoplasty: personal evolution on the concepts looking for an ideal technique. Aesthetic Plast Surg. 1997;21(6):417-23.
10. Graf RM, Bernardes A, Rippel R, Araújo LR, Damasio RC, Auerscald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8.
11. Stuzin JM, Baker TJ, Baker TM. Refinements in face lifting: enhanced facial contour using vicryl mesh incorporated into SMAS fixation. Plast Reconstr Surg. 2000;105(1):290-301.
12. Carvajal J, Echeverry A. Alternative technique for breast augmentation in patients with a small nipple-areolar complex diameter. Aesthet Surg J. 2005;25(2):117-25.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery -SBCP), adjunct professor in the Plastic Surgery Service of the Hospital de Clínicas da Universidade Federal do Paraná (Clinic's Hospital of the Federal University of Paraná -UFPR), Curitiba, PR, Brazil
2. Resident doctor in Plastic and Restorative Surgery of the Hospital de Clínicas da Universidade Federal do Paraná (Clinic's Hospital of the UFPR), Curitiba, PR, Brazil
3. Plastic surgeon, full member of the SBCP and the Brazilian Association of Craniomaxillofacial Surgery, chief of the Plastic Surgery Service of the Hospital de Clínicas da Uaniversidade Federal do Paraná (Clinic's Hospital of the UFPR), Curitiba, PR, Brazil
Correspondence to:
Ruth Graf
Rua Solimões, 1.175 - Mercês
Curitiba, PR, Brazil - CEP 80810-070
E-mail: ruthgraf@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 31, 2012
Article accepted: March 10, 2013
This study was performed at the Hospital de Clínicas da Universidade Federal do Paraná (Clinic's Hospital of the Federal University of Paraná), Curitiba, PR, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter