

Reviw Article - Year 2013 - Volume 28 -
Current state and future perspectives of craniofacial surgery research: systematic review
Estado atual e perspectivas futuras da pesquisa em cirurgia craniofacial: revisão sistemática
ABSTRACT
The term "evidence-based medicine," first used in the 1980s in Canada, is defined as "the conscious, explicit, and critical use of the best available evidence to make medical decisions regarding the care of individual patients." This study sought to estimate the viability of evidence-based medicine in modern craniofacial surgery practice 44 years after Paul Tessier first started it by showcasing his initial experience in that area. With the goal of identifying the best available evidence, the research focused on 5 central topics in this field: cleft lip and/or palate, orthognathic surgery, craniosynostoses, facial fractures, and hemifacial microsomia. This study used the Cochrane Library, the main database of evidence-based medicine. No Cochrane reviews were found for orthognathic surgery, craniosynostoses, or hemifacial microsomia. Similarly, no narrative reviews were found during the searched. No non-Cochrane reviews were found for facial fractures or craniosynostosis. The resulting number of reviews for each topic was low. A higher number of studies with clinical scientific evidence were found regarding facial fractures and cleft lip and/or palate. It was difficult to find a substantial number of articles on most of these topics when the Cochrane Library was used. As such, less confidence must be placed on studies with low levels of evidence and greater efforts are needed to service the need for good studies, which may guide clinical practice scientifically.
Keywords: Evidence-based medicine. Oral surgical procedures. Craniofacial abnormalities. Maxillofacial injuries. Review.
RESUMO
Medicina baseada em evidências é um termo cunhado nos anos 1980, no Canadá, sendo definido como o uso consciente, explícito e crítico da melhor evidência disponível para tomar decisões médicas sobre o cuidado individual de pacientes. Este estudo procurou estimar a viabilidade de prática da medicina baseada em evidências no exercício da cirurgia craniofacial moderna, após 44 anos que Paul Tessier marcou seu início, apresentando sua experiência inicial na área. Com o objetivo de identificar a melhor evidência disponível, buscas foram feitas em 5 temas centrais da área: fissura labial e/ou palatina, cirurgia ortognática, craniossinostoses, fraturas faciais e microssomia hemifacial. Para realização das pesquisas, foi utilizada a principal base de dados da medicina baseada em evidências, a Cochrane Library. Não foram identificadas revisões Cochrane para os temas: cirurgia ortognática, craniossinostoses e microssomia hemifacial. Também não foram encontradas revisões narrativas em nenhuma das buscas. Não foram encontradas revisões não-Cochrane para fraturas faciais e craniossinostose. O número de revisões resultante para cada tema se mostrou baixo. Foi encontrado maior número de ensaios com evidência científica clínica nos temas fraturas faciais e fissura labial e/ou palatina. Usando a principal base de dados da medicina baseada em evidências, não foi possível encontrar um número substancial de artigos na maioria dos temas. Desse modo, é preciso que uma menor confiança seja posta em estudos com baixos níveis de evidência, juntamente com maior esforço para suprir a necessidade de bons trabalhos que conduzam cientificamente a prática clínica.
Palavras-chave: Medicina baseada em evidências. Procedimentos cirúrgicos bucais. Anormalidades craniofaciais. Traumatismos maxilofaciais. Revisão.
Craniofacial surgery is known for its uncertainty and is associated with procedural and technical difficulties1. One of the reasons for this is the lack of high-quality studies in this field, as most are classified as reports or case studies2. The need for prolonged follow-up periods and a low prevalence of several conditions may partially explain the current situation. However, despite these issues, the World Health Organization (WHO) recommends the use of "evidence-based medicine" for the treatment of craniofacial abnormalities to overcome the lack of standardization that is currently present in craniofacial surgery1-4.
The term "evidence-based medicine" was coined at the McMaster Medical School in Canada in the 1980s to designate a clinical learning strategy that required a full decade to be developed5. This term was defined by Sackett et al.6 in 1996 as "the conscious, explicit, and critical use of the best available evidence to make medical decisions regarding the care of individual patients." Eddy7, the first to use and publish using the term "evidence-based," redefined "evidence-based medicine" as a set of principles and methods attempting to guarantee that, within reason, clinical decisions, guidelines, and other related policies are based on and consistent with evidence of their effectiveness and benefits.
The appearance of these ideas was related with the publication in 1991 that stated that only 15% of all medical interventions were supported by solid clinical trials8. The birth of evidence-based medicine was also favored by the realization that many clinicians had divergent views regarding the method of treatment of a patient, because of which there was discordance between clinical research findings and clinical practice, resulting in the need for other bases to support therapeutic decisions beyond the so-called clinical judgment and art of medicine5.
The practice of evidence-based medicine consists of 4 stages: (1) formulation of a clear clinical question arising from the patient's condition; (2) search of the scientific literature for relevant articles; (3) assessment of the validity and utility of the identified evidence; and (4) application of the information discovered in health care7.
In short, clinicians should use both experience and evidence from relevant scientific sources to make their decisions, as clinical practice becomes unjustified, wholly subjective, and harmful for patients without the best available evidence5.
The Cochrane Collaboration, an organization that collaborates with evidence-based medicine, became notorious through the publication of the Cochrane Reviews, considered by many to be the most comprehensive, reliable, and relevant sources of evidence in the scientific literature5. The name Cochrane is a tribute to Archie Cochrane, author of the influential book "Effectiveness and Efficiency: Random Reflections on Health Services" that was first published in 1972. In that book, Cochrane emphatically defended the use of evidence-based medicine on randomized and controlled clinical trials, which he considered to be much more reliable sources of information than any other options. By 1979, he suggested that critical reviews be written by specialty or sub-specialty and periodically updated of all relevant randomized and controlled clinical trials. From this idea, several systematic reviews were published in the mid-1980s covering randomized and controlled clinical trials, which guided treatment and research at that time. In 1992, the first Cochrane Center appeared in the United Kingdom that received support from researchers of several countries since its inception9.
The goals of the Cochrane Collaboration are to prepare, maintain, and disseminate updated systematic reviews of randomized and controlled clinical trials and, when these are not available, of other reliable sources of information with focus on improving health care. This organization is so structured that each reviewer at Cochrane is part of a collaborative review group, such as the Cochrane Oral Health Group, which consists of individuals who share interest in a particular medical topic. Such groups are coordinated by an editorial team, which takes responsibility for editing the module of reviews prepared by group members, such as the Oral Health Module. Subsequently, the reviews are published in the Cochrane Database of Systematic Reviews9.
In parallel with the development of the ideas of evidence-based medicine and projects supporting its practice, cranio-facial surgery became one of the fields of practice of plastic surgeons10. To many, the landmark for the birth of craniofacial surgery was the presentation of the initial experiment by Paul Tessier - considered the father of modern craniofacial surgery - in which he corrected a number of deformities at the Fourth Annual Congress of the International Confederation of Plastic Surgeons held in 196711. Tessier, with his multidisciplinary approach to patients and innovative surgical techniques, influenced several surgeons, including John M. Converse, the first surgeon ever to use a forehead flap in nasal reconstruction, Henry Kawamoto, ex-president and a rather active member of the American Society of Maxillofacial Surgeons, and Joseph G. McCarthy, the pioneer of distraction osteogenesis of the jaw, all of whom contributed to diffusion and scientific growth in this field4,12,13.
To estimate the viability of evidence-based medicine, 44 years after Tessier's presentation, we searched the Cochrane Library for articles involving 5 central topics in the field: cleft lip and/or palate, orthognathic surgery, facial fracture, hemifacial microsomia, and craniosynostosis.
METHODS
In February 2012, we searched the Cochrane Library for the following:
We recorded the number of articles found in the "Cochrane Reviews," "Other Reviews," and "Trials." The designs of the studies in the "Other Reviews" section were also noted. The main topics of the articles in the "Cochrane Reviews" and "Other Reviews" section, together with those of the publications in the "Trials" section on the subject of cleft lip and/ or palate were analyzed.Cleft lip and/or palate - simple search using the expression "cleft lip and palate" and the MeSH terms (MeSH search) "cleft lip" and "cleft palate"; Orthognathic surgery - search using the MeSH terms "orthognathic surgery" and "orthognathic surgical procedures"; Craniosynostosis - search using the MeSH term "craniosynostosis"; Facial fractures - simple search using the expression "facial fractures"; Hemifacial microsomia - simple search using the expression "hemifacial microsomia".
RESULTS
Cochrane Reviews
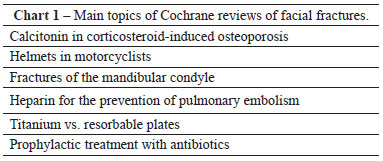
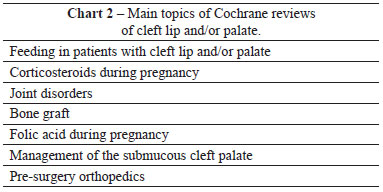
There were 7,027 Cochrane reviews of the 5 searched topics (Figure 1). The main topics of the Cochrane reviews by searched subject are listed in Charts 1 and 2.
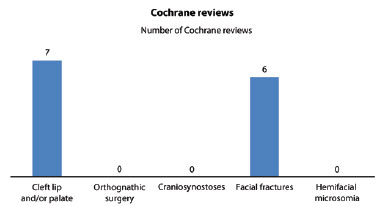
Figure 1 - Number of Cochrane reviews by the subject searched.
Other Reviews
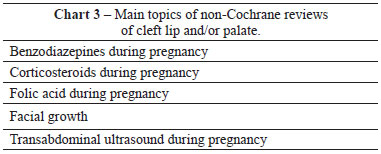
A total of 16,773 articles were noted in the "Other Reviews" section (non-Cochrane reviews) for all 5 searched topics. Five systematic reviews on cleft lip and/or palate, 5 on orthognathic surgery and 1 on hemifacial microsomia were identified. Not descriptive reviews related to any of the 5 subjects studied were found.
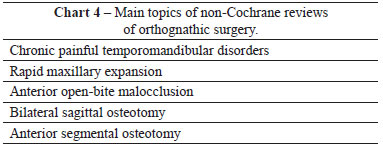
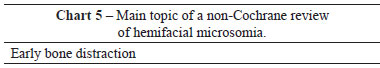
The main topics of the non-Cochrane reviews by searched subject are listed in Charts 3 to 5.
Other Studies
A total of 666,166 articles were found in the "Trials" section for all 5 searched topics (Figure 2). The main topics of the 201 selected articles on cleft lip and/or palate were noted. Table 1 shows the most frequent topics. Whenever the same study included 2 or more topics, the most important subject in the article was chosen to ensure that no article was counted more than once.
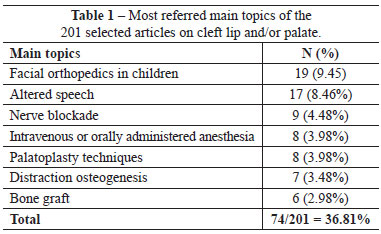
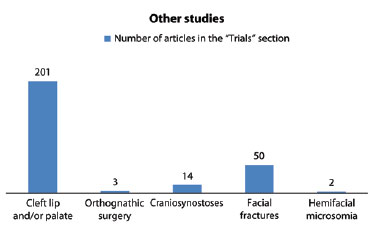
Figure 2 - Number of articles in the "Trials" section by the subject searched.
DISCUSSION
This study aimed to estimate the viability of evidence-based medicine in craniomaxillofacial surgery practice. To achieve this, we focused on the best available evidence using the Cochrane Library, the main evidence-based medicine database that makes pre-analyzed articles available14. To filter the data, 5 broad topics in the field were used: cleft lip and/or palate, orthognathic surgery, facial fracture, hemifacial microsomia, and craniosynostosis. Data on the study design and main article subjects were recorded to obtain a comprehensive overview of the searched topics and methodology.
To narrow the research focus, evidence-level system information was used. Such systems categorize studies to determine recommendation strength and evidence quality. In most evidence-level systems, study design is the main criterion used to classify a particular study. Among the principal tools for this approach to be conducted are those published by the Canadian Task Force on the Periodic Health Examination, U.S. Preventive Services Task Force, Task Force on Community Preventive Services, Oxford Centre for Evidence Based Medicine, and, the most currently used, Grading of Recommendations Assessment, Development and Evaluation15-17.
Despite system heterogeneity, all confirm that systematic reviews of well-conducted randomized and controlled clinical trials are the best study designs for determining the causal relationship between intervention and results8. The concept of review may theoretically be defined as the synthesis of all state-of-the-art research related to the clinical question under investigation. Within that definition, there are 2 different types of reviews: systematic and descriptive. The latter summarizes the relevant articles without describing the methodology. In contrast, the latter involves a comprehensive search for primary studies regarding pre-established clinical questions, which should contain all of the elements in the PICO acronym (Patient, Intervention, Comparison, and Outcome); in this review type, articles must be selected using clear and reproducible criteria and their results must be summarized using a pre-determined and well-explained method.
During the Cochrane review search performed here, few results were observed, and no articles were found on orthognathic surgery, craniosynostosis, or hemifacial microsomia. These data are in agreement with a survey conducted in 2008 that analyzed 3,487 articles on oral and maxillofacial surgery and found only 2 meta-analyses of randomized and controlled clinical trials18. Related data were recorded in a Cochrane Library search for articles on surgery, where it was found that only 5.3% of all systematic reviews were related to surgery19.
Facial fractures and cleft lip and/or palate were probably the only 2 topics with available Cochrane reviews because they represent groups of diseases that did not allow the retrieval of exact surgical data such as the prevention of facial fractures through the use of helmets, a fact that limited the orthognathic surgery search. Additionally, cleft lip and/or palate are congenital disorders with the highest prevalence of all 3 under investigation, which possibly contributed to the findings20-22. Similarly, of the high number of people (407,167) who suffered from facial fractures in the United States in 2007, the deaths of 3,057 of these individuals and the expenditure of $1 B USD in that period are factors that may help explain the interest in this topic23.
When analyzing the topics in the Cochrane and non-Cochrane reviews as well as in other studies on patients with cleft lip and/or palate, greater interest in and analysis of attitudes associated with the surgical procedure or not associated with the surgical procedure itself were observed. Such an observation is supported by data from a study conducted in 2005 that assessed the topics covered in surgical articles and showed that <25% of the same had surgery as their main subject, with most investigating the use of surgery-related drugs19.
On the other hand, all results of the identified non-Cochrane reviews of the 5 chosen topics were systematic. However, only articles related to hemifacial microsomia, cleft lip and/or palate, and orthognathic surgery were retrieved. Therefore, in our approach, a prevalence of Cochrane-quality reviews for facial fractures was observed, together with a large amount of systematic reviews obtained from several journals regarding the topic of orthognathic surgery.
A much higher number of articles was found in the "Trials" section, in which clinical scientific evidence trials are found, than in the other categories. Since these are primary articles14, the logical conclusion is that they are more likely to be much more frequent than secondary studies, such as reviews. Additionally, a prevalence of the topics facial fractures and cleft lip and/or palate was seen, as was the case in the Cochrane reviews. However, in such an approach to the database, there was clear superiority of the results on cleft lip and/or palate. It is possible that, although the interest on the part of the Cochrane Collaboration regarding both topics seems similar, the worldwide scientific community does not follow suit. Another possibility is that studies on facial fractures are more difficult to conduct due to the morphological variations associated with this disease23, which could lead both to a lower total number of available articles and to a higher number of low-quality studies that were filtered out by the Cochrane system.
Similarly to what was reported for craniomaxillofacial surgery, the practice of evidence-based medicine in surgery presents certain difficulties. One of the consequences of that fact is the lack of meta-analyses and randomized and controlled clinical trials (RCCTs) in that field. In support of that statement, a survey conducted in 2003 estimated that only 3.4% of all publications in the main journals of surgery were RCCTs. It was also observed in 2003 that the number of meta-analyses and RCCTs published in 4 prominent surgical journals (Annals of Surgery, Archives of Surgery, British Journal of Surgery, and Surgery) represented only 20% of the total of 4 general medical journals (British Medical Journal, Journal of the American Medical Association, Lancet, and New England Journal of Medicine)19. Moreover, the few surgical publications with such study designs are usually of low quality and inadequately reported24.
As with other surgical fields, craniomaxillofacial surgery has little high-quality evidence available, such as in systematic reviews. Some explanations for this are the difficulty in standardizing treatment. The use of control groups with placebo or without therapeutic intervention may be considered undesirable or unethical. Blinding of all subjects is often impractical and difficult to execute. Skewing of the learning curve to the right and upward can occur as a surgeon increases the number of times he/she performs a surgery. Further, the surgical results obtained are dependent on certain factors, such as the surgeon's experience, which hampers reproducibility; use of a small sample of patients who require a specific procedure; and the presence of studies with little or no evidence, such as reports and case studies12,24,25.
It should also be noted that craniofacial surgery is a relatively new field. While the American Society of Maxillofacial Surgeons (ASMS) was founded in 194712, the American Association of Plastic Surgeons, American College of Surgeons, and American Medical Association were established in 192113, 191326, and 184727, respectively. As such, only 64 years have passed since the pioneer ASMS was founded, and modern craniofacial surgery began only 44 years ago, after Tessier's presentation in 196711. Thus, considering that the field is new, there has probably not been enough time for the 6 principles proposed by Harold Gillies - the father of plastic surgery and pioneer in craniofacial surgical procedures - to be fully achieved: approach the patient in a multidisciplinary setting, allow continuous treatment of patients aged 0-18 years, have its own teaching and training, hold financial resources and infrastructure in an organized manner, be directed by protocols, and be connected to a research database4. According to our study and the evidence cited, these last 2 goals are far from being achieved.
CONCLUSIONS
The practice of evidence-based medicine is limited in craniomaxillofacial surgery, largely because of a lack of RCCTs and well-conducted systematic reviews. As such, less confidence should be placed in studies with low evidence levels, while we must increase our efforts to produce more high-quality studies to scientifically guide clinical practice.
REFERENCES
1. World Health Organization. Global strategies to reduce the health-care burden of craniofacial anomalies: report of WHO meetings on International Collaborative Research on Craniofacial Anomalies, Geneva, Switzerland, 5-8 November 2000; Park City, Utah, USA, 24-26 May 2001. Geneva: World Health Organization; 2002.
2. Kyzas PA. Evidence-based oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008;66(5):973-86.
3. Sandhu A. The evidence base for oral and maxillofacial surgery: 10-year analysis of two journals. Br J Oral Maxillofac Surg. 2012;50(1):45-8.
4. Simpson DA, David DJ. Herbert Moran Memorial Lecture. World War I: the genesis of craniomaxillofacial surgery? ANZ J Surg. 2004;74(1-2):71-7.
5. Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem-solving. BMJ. 1995;310(6987):1122-6.
6. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71-2.
7. Eddy DM. Evidence-based medicine: a unified approach. Health Aff (Millwood). 2005;24(1):9-17.
8. Lau SL, Samman N. Evidence-based practice in oral and maxillofacial surgery: audit of 1 training center. J Oral Maxillofac Surg. 2007;65(4):651-7.
9. Chalmers I. The Cochrane collaboration: preparing, maintaining, and disseminating systematic reviews of the effects of health care. Ann N Y Acad Sci. 1993;703:156-63.
10. Faculdade de Medicina da Universidade de São Paulo. Cirurgia Plástica da Faculdade de Medicina da Universidade de São Paulo. Histórico. Disponível em: http://www.fm.usp.br/plastica/historico.html. Acesso em: 16/2/2012.
11. Associação Brasileira de Cirurgia Crânio-maxilo-facial. Histórico: a biografia de Paul Tessier. Disponível em: http://www.abccmf.org.br/cmf/Sbcc/Hist/historia2.html Acesso em: 16/2/2012.
12. Cohen SR, Juhala CA, Manson PN, Crawley WA, Jacobs JS. History of the American Society of Maxillofacial Surgeons: 1947-1997. Plast Reconstr Surg. 1997;100(3):766-801.
13. Randall P, McCarthy JG, Wray RC. History of the American Association of Plastic Surgeons, 1921-1996. Plast Reconstr Surg. 1996;97(6):1254-98.
14. Pai M, McCulloch M, Gorman JD, Pai N, Enanoria W, Kennedy G, et al. Systematic reviews and meta-analyses: an illustrated, step-by-step guide. Natl Med J India. 2004;17(2):86-95.
15. Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health. 2002;56(2):119-27.
16. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
17. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-6.
18. Kyzas PA. Evidence-based oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008;66(5):973-86.
19. Slim K. Limits of evidence-based surgery. World J Surg. 2005;29(5):606-9.
20. Monahan R, Seder K, Patel P, Alder M, Grud S, O'Gara M. Hemifacial microsomia. Etiology, diagnosis and treatment. J Am Dent Assoc. 2001;132(10):1402-8.
21. Yañez-Vico RM, Iglesias-Linares A, Gómez-Mendo I, Torres-Lagares D, Gonzáles-Moles MA, Gutierrez-Pérez JL, et al. A descriptive epidemiologic study of cleft lip and palate in Spain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2012.
22. Kweldam CF, van der Vlugt JJ, van der Meulen JJ. The incidence of craniosynostosis in the Netherlands, 1997-2007. J Plast Reconstr Aesthet Surg. 2011;64(5):583-8.
23. Allareddy V, Allareddy V, Nalliah RP. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011;69(10):2613-8.
24. Sade RM. "Surgical research or comic opera" redux. Ann Thorac Surg. 2006;82(4):1173-4.
25. Horton R. Surgical research or comic opera: questions, but few answers. Lancet. 1996;347(9007):984-5.
26. American College of Surgeons. History and overview: history of the College. Disponível em: http://www.facs.org/archives/acshistory.html Acesso em: 16/2/2012.
27. American Medical Association. Illustrated highlights: 1847 to 1899. Disponível em: http://www.ama-assn.org/ama/pub/about-ama/our-history/illustrated-highlights/1847-1899.page? Acesso em: 16/2/2012.
1. Medical student at the Faculty of Medicine of the University of São Paulo (FMUSP), São Paulo, SP, Brazil
2. Full professor in Plastic Surgery by the FMUSP, associate professor at the FMUSP, head of the Craniomaxillofacial Surgery Department, Division of Plastic Surgery and Burns, Hospital das Clínicas, Faculty of Medicine of the University of São Paulo, São Paulo, SP, Brazil
Correspondence to:
Nivaldo Alonso
Rua Afonso Brás, 473 - cj. 65 - Vila Nova Conceição
São Paulo, SP, Brazil - CEP 04511-000
E-mail: nivalonso@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: February 27, 2012
Article accepted: April 21, 2012
This study was performed at the Faculty of Medicine of the University of São Paulo, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter