

Case Report - Year 2013 - Volume 28 -
Total-thickness lesion of the scalp of infectious origin
Lesão de couro cabeludo de espessura total de origem infecciosa
ABSTRACT
Scalp reconstruction aims to achieve an appropriate appearance and is fundamentally important to the integrity of the skeletal structure to protect the central nervous system. The present work describes the case of a child aged 1 year and 5 months with a total-thickness lesion of the scalp presenting with ischemic areas in the cranial calotte and absence of periosteum after infection. The lesion was urgently debrided, washed with 9% normal saline, and dressed with silver sulfadiazine ointment for 2 days. The patient was subsequently transferred to the surgical center, and multiple perforations were made in the outer table of the skull. A dressing was made with rayon gauze soaked with petrolatum emulsion and removed 7 days after the surgery accompanied by antibiotic administration. Finally, 10 days after surgery, split-thickness skin grafting was performed, and satisfactory aesthetic results were obtained.
Keywords: Skull/surgery. Scalp/injuries. Scalp/surgery.
RESUMO
A reconstrução do couro cabeludo, além do propósito de manutenção da forma, é de fundamental importância para a integridade do arcabouço ósseo, com o objetivo de proteção do sistema nervoso central. No presente trabalho, é descrito o caso de uma criança de 1 ano e 5 meses de idade, com lesão de espessura total do couro cabeludo, presença de áreas de isquemia na região da calota craniana após infecção e ausência de periósteo. Foram realizados, em regime de urgência, desbridamento da lesão, lavagem com soro fisiológico a 9% e curativo com pomada de sulfadiazina de prata, durante dois dias. Posteriormente, o paciente foi levado ao centro cirúrgico para realização de múltiplas microperfurações da tábua externa do crânio. Foi realizado curativo com gaze raiom embebida em emulsão de petrolatum, que foi retirada no sétimo dia de pós-operatório, acompanhado de cobertura antibiótica. Finalmente, no décimo dia de pós-operatório, foi realizado enxerto de pele parcial, com obtenção de resultado estético satisfatório.
Palavras-chave: Crânio/cirurgia. Couro cabeludo/lesões. Couro cabeludo/cirurgia.
The covering of the cephalic segment is formed by specific and distinct anatomic structures. It may be divided in soft parts, represented by the scalp and its layers, and bone tissues, which consist of the cranial calotte. The soft parts are divided into 5 anatomic layers: the skin, subcutaneous tissue, galea, loose areolar tissue, and pericranial tissue.
With a purely didactic aim, lesions can be classified according to their anatomic purposes (e.g., soft and bone parts), thickness (e.g., partial and total), and time of progression (e.g., acute and late).
In total-thickness lesions of the scalp involving the loss of all the layers and exposure of the cranial calotte, covering the bone structure with vascularized tissues is critical; moreover, closing the lesion area is important for preventing alopecia1-6. The lack of covering of the cranial calotte may also lead to bone necrosis and infections of bone tissues, which may result in the loss of the cranial calotte and exposure of the central nervous system. These lesions are primarily of traumatic origin such as dog bites, burns, and neoplasia, and are rarely caused by infections.
Here, we report the case of a patient with a total-thickness lesion of the scalp of infectious origin.
CASE REPORT
The patient was 1 year and 5 months of age with a history of a neglected abscess in the frontal region (a home treatment was attempted); the lesion evolved to necrosis of the scalp area, and the patient was examined in the emergency unit of the Josina Machel Hospital, Luanda, Angola.
On physical examination, the patient presented with a total-thickness lesion of the scalp with ischemia in the region of the outer table of the cranial calotte, with the length being 15 cm and the width being 8 cm, irregular borders, and the presence of purulent secretion (Figure 1).

Figure 1 - Ischemic areas in the outer table of a part of the left frontal and parietal bones with the absence of periosteum after a lesion of an infectious nature of the scalp.
The borders of the lesion were urgently debrided, washed with 9% normal saline, and dressed with silver sulfadiazine ointment for 2 days.
The patient was subsequently transferred to the surgical center to receive multiple perforations in the outer table of the skull (Figure 2). A dressing was made with rayon gauze soaked with petrolatum emulsion and was removed 7 days after the surgery accompanied by antibiotic administration.
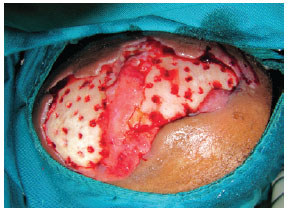
Figure 2 - Intraoperative photograph of the micro-perforations made in the outer table of the skull 2 days after the debridement of the lesion.
Finally, 10 days after surgery, granulation was observed in 96% of the lesion (Figure 3). Consequently, split-thickness skin grafting was performed (Figure 4) and satisfactory aesthetic results and good graft integrity were observed.

Figure 3 - Granulation tissue in the lesion region 10 days after the micro-perforations were made.

Figure 4 - View of the lesion 7 days after split-thickness skin grafting, showing some areas lacking graft integration.
The patient is currently scheduled to undergo treatment of the alopecic area (Figure 5), which will be conducted with the help of a tissue expander.

Figure 5 - View of the lesion 30 days after split-thickness skin grafting.
DISCUSSION
In cases of extensive lesions of the scalp with loss of pericranial tissue, associated infections, or debilitated patients, or even when there is a lack of resources to conduct more elaborate procedures, the technique of micro-perforations of the outer table of the skull is the most strongly indicated.
Because children particularly present with a diploe that contains a large quantity of highly vascularized spongy bone tissue, this technique allows the formation of granulation tissue in a few days; moreover, a split-thickness skin graft can be applied over this, thus facilitating the closure of the bone area.
Although microsurgery is increasingly being recommended, the technique applied herein was developed several years earlier and remains the best option in these cases. Considering the initial infection and lesion extent, it is very important to quickly define the therapeutic plan, while taking advantage of the large amount of diploe vascularization, which is typical of patients of this age; this promotes good granulation in a few days, and allows the prompt application of a split-thickness skin graft.
REFERENCES
1. Alpert BS, Buncke HJ Jr, Mathes SJ. Surgical treatment of the totally avulsed scalp. Clin Plast Surg. 1982;9(2):145-59.
2. Argenta LC, Watanabe MJ, Grabb WC. The use of tissue expansion in head and neck reconstruction. Ann Plast Surg. 1983;11(1):31-7.
3. Temple CL, Ross DC. Scalp and forehead reconstruction. Clin Plast Surg. 2005;32(3):377-90.
4. Gosain AK, Zochowski CG, Cortes W. Refinements of tissue expansion for pediatric forehead reconstruction: a 13-year experience. Plast Reconstr Surg. 2009;124(5):1559-70.
5. Nahai F, Hurteau J, Vasconez LO. Replantation of an entire scalp and ear by microvascular anastomoses of only 1 artery and 1 vein. Br J Plast Surg. 1978;31(4):339-42.
6. Mélega JM. Cirurgia plástica: fundamentos e arte. Rio de Janeiro: Medsi; 2002.
1. Resident Physician in Plastic Surgery in the Faculdade de Ciências Médicas da Universidade Estadual de Campinas (Faculty of Medical Sciences of the State University of Campinas - UNICAMP), Campinas, SP, Brazil, with technical collaboration between UNICAMP and the Angola Ministry of Health
2. Plastic Surgeon, Head of the Plastic Surgery in Hospital das Clínicas of UNICAMP, Campinas, SP, Brazil
3. Plastic Surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery, Coordinator of Plastic Surgery of the Faculty of Medical Sciences of UNICAMP, Campinas, SP, Brazil
Correspondence to:
Dadi Bucusso Netemo
Rua Hermantino Coelho, 77 - bloco 1 - apto 73 - Mansões de Santo Antonio
Campinas, SP, Brazil - CEP 13087-500
E-mail: medibucusso@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 18, 2010
Article accepted: March 23, 2011
This study was performed at the Josina Machel Hospital, Luanda, Angola.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter