

Original Article - Year 2013 - Volume 28 -
Rehabilitation after partial brachial plexus palsy
Reabilitação na paralisia parcial do plexo braquial
ABSTRACT
A variety of muscle transfer techniques have been proposed to restore motion of the upper extremities following severe brachial plexus palsy. Paralysis of the deltoid and supraspinatus muscles can be treated with transfer of the trapezius muscle. Paralysis of the wrist, hand, and digital extensor muscles can be corrected using the pronator teres, flexor carpi ulnaris, and palmaris longus muscles if the median nerve is preserved. Here we describe the rehabilitation of a patient with an old partial injury to the right brachial plexus that primarily involved the upper trunk from the C6 root to the posterior cord. Weakness of the deltoid muscle, wrist, and digital extensor muscles was observed. Microsurgical repair of the brachial plexus had not been performed. Tendon transfer surgery was performed to improve wrist, hand, and digital extension. One year later, transfer of the trapezius muscle was performed to stabilize the shoulder. The success of muscle transfer in the treatment of the brachial plexus palsy required the surgeon's specialization, the patient's motivation, and a rehabilitation program.
Keywords: Brachial plexus/injuries. Muscle, skeletal/physiopathology. Muscle, skeletal/ transplantation.
RESUMO
Muitas transferências musculares têm sido defendidas para restaurar os movimentos do membro superior após paralisia grave do plexo braquial. A paralisia dos músculos deltoide e supraespinal pode ser tratada por meio de transferência do músculo trapézio. A paralisia dos músculos extensores de punho, mão e dedos, quando o nervo mediano está preservado, pode ser corrigida com emprego dos músculos pronador redondo, flexor ulnar do carpo e palmar longo. Os autores descrevem um caso de reabilitação de paciente portador de lesão parcial antiga do plexo braquial à direita, de predomínio em tronco superior, principalmente da raiz de C6 e de fascículo posterior. Foi evidenciada fraqueza dos músculos deltoide e extensores do punho e dos dedos, sem antecedentes de reparo microcirúrgico do plexo braquial. Foi realizada, inicialmente, cirurgia de transferência tendínea para ganho de extensão de punho, mão e dedos e, após um ano, transferência do músculo trapézio, para estabilização do ombro. O sucesso na transferência para tratamento de paralisia do plexo braquial requereu especialização do cirurgião, motivação do paciente e programa de reabilitação.
Palavras-chave: Plexo braquial/lesões. Músculo esquelético/fisiopatologia. Músculo esquelético/transplante.
Most traumatic lesions of the brachial plexus result from motorcycle accidents. The lesions can be located at the supraclavicular level (affecting roots and trunks) or the infraclavicular level (affecting cords and terminal branches) and may be total or partial.
Surgical exploration may be acute, i.e., performed at the moment of trauma in the case of an open injury, an injury associated with a vascular lesion, or total avulsion (C5-T1). Cases in which recovery of the complete lesion is not observed on electroneuromyography examination between the first 2 to 3 months and 12 months after the injury or in which there is persistent shoulder and elbow paralysis are candidates for investigation. Treatment options include microsurgical exploration with neurolysis, repair, grafting, or nerve transfer, depending on root avulsion. Transfer options include moving the accessory nerve to the suprascapular nerve or the musculocutaneous nerve to the ulnar and intercostal nerves. Good functional results have been reported in the literature1,2.
The primary goals of brachial plexus reconstructive surgery include stabilization of the shoulder, restoration of the ability to hold objects between the arm and the thorax, restoration of active flexion of the elbow against gravity, and recovery of the protective sensitivity of the palm. From a functional point of view, reconstructive surgery of the brachial plexus restores elbow and shoulder function, wrist and digital flexion, and digital and intrinsic muscle extension.
The occurrence of gradual changes in the shoulder joint, which are classified according to Birch3, Pearl4 and Waters et al.5, and, should be noted. These 3 authors classify the injury according to increasing severity of subluxation of the humeral head of the joint. Waters' et al.5 classification describes the following 5 types of injury: normal (type I); deformity of the posterior glenoid cavity (type II); subluxation of the humeral head and glenoid plus dysplasia (type III); development of a false glenoid cavity (type IV); and flattening of both the glenoid cavity and the humeral head (type V). The degree of joint deformity can help the surgeon select the surgical procedure5.
In the case of avulsion, unsuccessful neurorrhaphy, or untreated and late-admitted patients with injuries of the brachial plexus, tendon transfers are indicated for the recovery of upper extremity function1,2,6-8. Although various procedures have been described, rehabilitation continues to be a challenge for surgeons, and the reporting of results remains scarce. However, it is worth noting that the goal of tendon transfer is to improve tendon balance and upper extremity function. Transfer of the trapezius muscle has been described for the treatment of paralysis of the deltoid and supraspinatus muscles1-3,6,7. In the case of paralysis of the forearm extensor muscles in which elbow extension is preserved, transfer of the pronator teres, flexor carpi ulnaris, and palmaris longus muscles yields satisfactory results for shoulder stabilization as well as wrist, hand, and digital function8-15.
In the present report, we describe the surgical techniques and the rehabilitation program that were used in the treatment of a patient with an old brachial plexus injury that involved mainly the upper trunk, in particular from the C6 root to the posterior cord. Weakness of the deltoid muscle, wrist, and digital extensor muscles was observed. No evidence of previous microsurgical repair of the brachial plexus was observed.
CASE REPORT
A 34-year-old man was admitted in 2003 with a lesion of the right brachial plexus caused by a fall from a tree that had occurred 18 months previously. No microsurgical repair had been performed.
On physical examination, the patient presented with hypotrophy and hypoesthesia to deep pressure in the entire right upper extremity from C4 to T1. His inability to abduct the shoulder or actively extend the wrist, hand, and fingers as well as evidence of subluxation revealed the involvement of the scapular region; the deltoid and supraspinatus muscles; and the wrist, hand, and digital extensor muscles (Figures 1 and 2). Elbow flexion-extension was preserved.

Figure 1 - In A and B, preoperative appearance showing shoulder limitation and the inability to extend the wrist, hand, and fingers. In C, D, and E, appearance in the 5th postoperative year with abduction to 70º and wrist, hand, and digital extension.
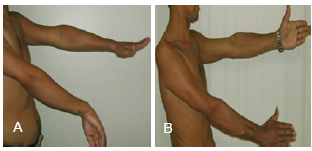
Figure 2 - In A, preoperative appearance. In B, appearance in the 7th postoperative year.
An electroneuromyographic (EMG) study revealed an incomplete axonal injury of the right brachial plexus with severe involvement of the shoulder, wrist, and digital extensor muscles. There were severe signs of recent and chronic denervation, an axonal injury of the lateral cutaneous nerve of the forearm, and a preganglionic injury (radiculopathy) at C6 with signs of moderate to severe denervation intensity.
In 2004, to restore wrist, hand, and digital extension, transfers were performed of the pronator teres muscle to the extensor carpi radialis brevis muscle, the flexor carpi ulnaris muscle to the extensor digitorum communis muscle, and the palmaris longus muscle to the extensor pollicis longus muscle according to the modified Burkhalter13 technique (Figure 3). A physiotherapy program was started on the 30th postoperative day (Table 1).
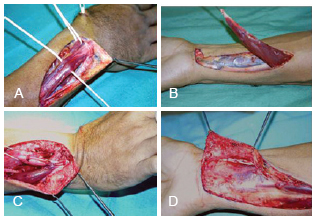
Figure 3 - Intraoperative view of transfer for wrist extension. In A, identification of the pronator teres and extensor carpi radialis brevis muscles. In B, release of the flexor carpi ulnaris muscle. In C, transfer of the flexor carpi ulnaris muscle to the common extensor muscle of fingers. In D, palmaris longus muscle transferred to the long extensor pollicis longus muscle.
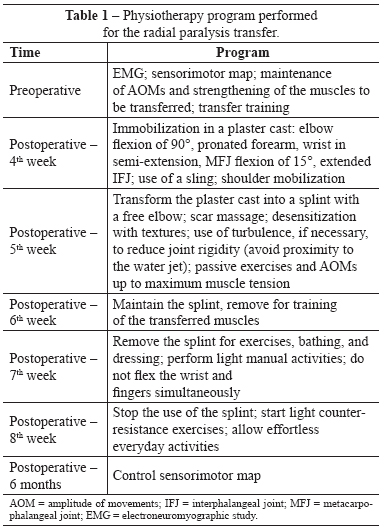
In 2005, a transfer of the trapezius muscle with a segment of the acromionto the lateral surface ofthe humerus usingthe modified Saha technique was performed to stabilize the shoulder and permit arm abduction6,11 (Figure 4). The quality of the glenohumeral j oint was assessed via a radiological exam. Pre -and postoperative physiotherapy programs were conducted (Table 2 and Figure 5). In the evaluation performed 7 years postoperatively, functional improvement and a muscle map with grade 4 wrist, hand, and digital extension; grade 3 thumb extension; and mobility and active elevation of the right shoulder with grade 4 muscle strength (60 degrees of active abduction and 70 degrees of flexion) were seen. The functional result was satisfactory, and the patient was considered rehabilitated and able to independently perform everyday activities and work activities.
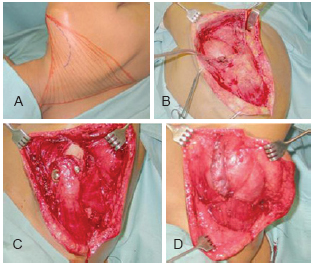
Figure 4 - In A, patient in lateral decubitus position with a free hand and arm. In B, curvilinear incision over the spine reaching the lateral margin of the scapula with exposed trapezius and deltoid muscles, and lateral proximal third of the humerus. In C, release of the trapezius muscle insertion with a segment of the acromion and fixation of the humerus with abduction to 90° using 2 lag screws. In D, suture of the trapezius and deltoid muscles to the fixation.
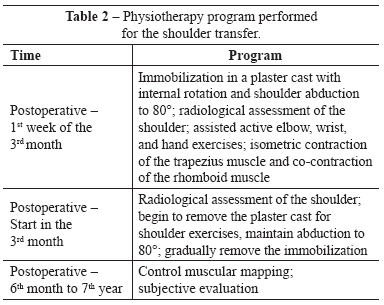
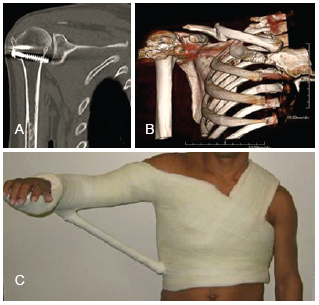
Figure 5 - In A, computed tomography examination. In B, three-dimensional reconstruction. In C, immobilization in a plaster cast with abduction to 80° and internal rotation of the shoulder (used for 4 months).
DISCUSSION
Segmental injuries of the brachial plexus with shoulder paralysis and glenohumeral subluxation associated with the paralysis of the forearm extensor muscles and the inability to extend the wrist, hand, and fingers cause great functional impairment of the upper extremities. According to Malessy et al.1 and Bertelli & Ghizoni2, injuries to the brachial plexus that involve C5 and C6, such as the lesion described in this report, have a poor outcome after nerve reconstruction using grafts or nerve transfer procedures. However, some authors have reported satisfactory results after muscle tendon transfer to the shoulder1-6,11. Indications for surgical intervention in the shoulder include subluxation, persistent internal contracture not resolved by physiotherapy, limited active abduction and external rotation, and a progressive deformity of the gleno-humeral joint. The treatment is based on surgical contracture release, muscle balancing, and joint reduction.
Options for shoulder stabilization via muscle balancing include transfers as described by Saha6 and Bateman7 and shoulder arthrodesis8. Saha6 described a modification of Bateman's7 technique that uses the trapezius muscle to stabilize and restore active function of the shoulder, and variable functional results have been reported. Ruhmann et al.10 described an abduction gain of 70-90º along with functional recovery and subjective improvement, findings that are in accordance with those described in the present report. The requirements for transfer are as follows: passive shoulder abduction to 80º, patient agreement regarding the long immobilization time, and satisfactory preoperative condition of the glenohumeral joints. If these requirements are not met, shoulder arthrodesis must be performed in the functional position, which carries a higher risk of morbidity and is considered the last resort7,8,11.
Satisfactory results have been reported with regard to the use of the modified Burkhalter transfer for the correction of triple paralysis of the radial nerve13. This technique was used in the case described in the present report with excellent functional improvement; however, the importance of preoperative evaluation and training, muscle traction line, and suture tension and immobilization should be noted. Other options have been described, such as the transfer of the flexor carpi radialis muscle or the flexor digitorum muscles to the extensor digitorum communis muscle13-15.
In the present case report, rehabilitation of a patient with an old partial injury of the brachial plexus was achieved after performing a surgical transfer procedure to restore wrist, hand, and digital extension using the pronator teres, flexor carpi ulnaris, and palmaris longus muscles and to stabilize the shoulder using the trapezius muscle. The main factors that contributed to the success of the surgery included the preoperative preparation, including patient training and participation, fixation of the trapezius muscle to the humerus, tension of the transferred muscle, appropriate immobilization for a prolonged period, and the postoperative physiotherapy program.
REFERENCES
1. Malessy MJ, Ruiter GC, Boer KS, Thomeer RT. Evaluation of suprascapular nerve neurotization after nerve graft or transfer in the treatment of brachial plexus traction lesions. J Neurosurg. 2004;101(3):377-89.
2. Bertelli JA, Ghizoni MF. Transfer of the accessory nerve to the suprascapular nerve in brachial plexus reconstruction. J Hand Surg Am. 2007;32(7):989-98.
3. Birch R. Obstetric brachial plexus palsy. J Hand Surg Br. 2002;27(1):3-8.
4. Pearl ML. Arthroscopic release of shoulder contracture secondary to birth palsy: an early report on findings and surgical technique. Arthroscopy. 2003;19(6):577-82.
5. Waters PM, Smith GR, Jaramillo D. Glenohumeral deformity secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 1998;80(5):668-77.
6. Saha AK. Surgery of the paralyzed and flail shoulder. Acta Orthop Scand. 1967;97(Suppl):5-90.
7. Bateman JE. The shoulder and environs. St. Louis: C.V. Mosby; 1955. p. 383-93.
8. Aziz W, Singer RM, Wolff TW. Transfer of the trapezius for flail shoulder after brachial plexus injury. J Bone Joint Surg Br. 1990;72(4):701-4.
9. Mir-Bullo X, Hinarejos P, Mir-Batlle P, Busquets R, Carrera L, Navarro A. Trapezius transfer for shoulder paralysis: 6 patients with brachial plexus injuries followed for 1 year. Acta Orthop Scand. 1998;69(1):69-72.
10. Rühmann O, Schmolke S, Bohnsack M, Carls J, Wirth CJ. Trapezius transfer in brachial plexus palsy. Correlation of the outcome with muscle power and operative technique. J Bone Joint Surg Br. 2005;87(2):184-90.
11. SinghAK, Karki D. Modified trapezius transfer technique for restoration of shoulder abduction in brachial plexus injury. Indian J Plast Surg. 2007;40(1):39-46.
12. Motta Filho GR, Mendes HM, Faria LOM. Transferências tendinosas para tratamento da paralisia radial. Rev Bras Ortop. 1990;25(10):341-8.
13. Burkhalter WE. Early tendon transfers in upper extremity peripheral nerve injury. Clin Orthop Relat Res. 1974;104:68-79.
14. Boyes JH. Tendon transfers for radial nerve palsy. Bull Hosp Joint Dis. 1960;21:97-105.
15. Chuinard RG, Boyes JH, Stark HH, Ashworth CR. Tendon transfers for radial nerve palsy: use of superficialis tendons for digital extension. J Hand Surg Am. 1978;3(6):560-70.
1. Plastic Surgeon at the Hospital Sarah Brasília, Full Member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), President of the Regional do Distrito Federal da SBCP, Brasília, DF, Brazil
2. Plastic Surgeon at the Hospital Sarah Brasília, Full Member of the SBCP, Brasília, DF, Brazil
Correspondence to:
Kátia Torres Batista
SQN, 115 - Bloco I - ap. 205 - Asa Norte
Brasília, DF, Brazil - CEP 70772-090
E-mail: katiatb@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 3, 2010
Article accepted: October 18, 2010
This study was performed at the Rede Sarah de Hospitais de Reabilitação, Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter