

Case Report - Year 2013 - Volume 28 -
Pleomorphic sarcoma in Marjolin 's ulcer
Sarcoma pleomórfico em úlcera de Marjolin
ABSTRACT
Marjolin's ulcer is a malignant transformation of traumatized or chronically inflamed cutaneous tissue that occurs after burns. The most common histological type of carcinoma found in Marjolin's ulcers is squamous cell carcinoma, followed by basal cell carcinoma and malignant melanoma. Sarcomas in Marjolin's ulcers are rare, representing approximately 5% of these malignant degenerations. In this report, we describe the case of a female patient who was burned 42 years prior, with a large ulceration on her back. Biopsy of the ulceration showed a high-grade pleomorphic sarcoma in the Marjolin's ulcer. The patient underwent resection of the ulceration and a skin graft followed by radiation therapy and adjuvant chemotherapy. In 3 years of follow-up, the patient had no tumor recurrence. Marjolin's ulcers are aggressive and have a high rate of regional metastases. It is important that clinicians develop an understanding of their prevention by properly treating burns. Sarcomas in Marjolin's ulcers are rare and few cases have been reported in the literature, which demonstrates the importance of this report.
Keywords: Burns. Sarcoma. Skin ulcer.
RESUMO
Úlcera de Marjolin é uma transformação maligna em tecido cutâneo cronicamente inflamado ou traumatizado, que ocorre especialmente após queimaduras. O carcinoma de células escamosas é o tipo histológico mais encontrado nas úlceras de Marjolin, seguido de carcinoma basocelular e melanoma maligno. Sarcomas em úlcera de Marjolin são raros, correspondendo a aproximadamente 5% dessas degenerações malignas. Neste artigo é descrito o caso de paciente do sexo feminino, vítima de queimadura há 42 anos, com grande ulceração em dorso. A biópsia dessa ulceração evidenciou sarcoma pleomórfico de alto grau em úlcera de Marjolin. A paciente foi submetida a ressecção da ulceração e enxerto de pele no local, seguidos de radioterapia e quimioterapia adjuvantes. Em 3 anos de seguimento, a paciente não apresentou recidiva da neoplasia. Úlceras de Marjolin são neoplasias malignas de comportamento agressivo, com alto índice de metástases regionais. A importância de seu entendimento está na necessidade de prevenção das mesmas, com o tratamento adequado dos pacientes queimados, evitando-se a cicatrização por segunda intenção. Sarcomas em úlcera de Marjolin são considerados raros, com poucos casos relatados na literatura, o que demonstra a importância deste relato.
Palavras-chave: Queimaduras. Sarcoma. Úlcera cutânea.
Marjolin's ulcer is a malignant transformation of traumatized or chronically inflamed cutaneous tissue that occurs most frequently after burns1-6. The term was first employed by Marjolin in 1828 to describe malignant ulcers derived solely from burns1-3,5. The term is currently also used for malignant lesions arising from other tissue injuries, such as vaccinations, snake bites, osteomyelitis, pressure or venous ulcers, fistulas, and other traumatic wounds, although burns are reported as being responsible for approximately 75% of the cases1-3,5.
The genesis of the Marjolin's ulcers remains unknown, but it is believed that chronic irritation of the tissue is one of the main triggers of the malignant transformation process2. Other etiological factors have also been studied, including toxins, immune factors, oncogenes, poor lymphatic regeneration, antibodies, and mutations1,2,5.
In a review of 443 cases, Kerr-Valentic et al.3 reported an average patient diagnostic age of 52 years, with an average period of 29 years between the burn and the diagnosis. These authors observed the development of metastases in 27.5% of the patients.
The lower limbs are the most commonly affected by this disease (53%), followed by the upper limbs (19%) and the torso (12%)3. Additionally, men are more commonly affected by this disease than women with a male:female ratio of 2:11.
The most common histological type of carcinoma observed is squamous cell carcinoma, followed by basal cell carcinoma and malignant melanoma1,7. Sarcomas associated with Marjolin's ulcers, including high-grade pleomorphic sarcoma - also known as malignant fibrous histiocytoma - are extremely rare. Kim et al.7 found only 7 high-grade pleomorphic sarcomas described in ulcers derived from burns and described the first case, which was on a patient's back. It is believed that the rare incidence compared with carcinoma is because of the deeper location of the mesenchymal cells in the dermis or subcutaneous tissue, which makes it less vulnerable to trauma and requires less tissue regeneration than the superficial epidermis7.
In an extensive literature review, Kowal-Vern and Cris-well1 identified that of 412 cases of Marjolin's ulcer, 71% corresponded to squamous cell carcinomas, 12% to basal cell carcinomas, 6% to melanomas, 2% to squamous cell carcinoma associated with basal cell carcinomas, 1% to squamous cell carcinomas associated with melanomas, 5% to sarcomas, and 4% to other tumors. Among the 20 sarcomas, 8 were high-grade pleomorphic sarcomas, 3 were fibrosarcomas, 2 were liposarcomas, and 2 were dermatofibrosarcomas.
In a review of the literature on sarcomas in ulcers caused by burns, Ozyazgan and Kontas6 found 13 cases of sarcomas in Marjolin's ulcers consisting of 4 fibrosarcomas, 3 high-grade pleomorphic sarcomas, 2 liposarcomas, 1 carcinosarcoma, 1 osteosarcoma, 1 malignant schwannoma, 1 leiomyosarcoma, and 1 mesenchymal neoplasm.
CASE REPORT
A 48-year-old Caucasian woman was referred to the Department of Plastic Surgery, St. Joseph Municipal Hospital of Joinville (Joinville, SC, Brazil) for the treatment of a large ulcerovegetative lesion in the left lumbar area approximately 12 cm in diameter, with purulent exudate and necrotic areas, and an onset approximately 6 years ago (Figure 1).
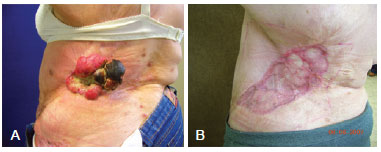
Figure 1 - Marjolin's ulcer on the patient's back. In A, the injured area prior to treatment. In B, the area 5 months after resection and skin grafting.
The patient was a victim of a burn by fire in the anterior and posterior torso when she was 6 years old. Physical examination revealed no axillary or inguinal lymphadenopathies.
The patient underwent resection of the lesion with 2-cm margins and an intermediate thickness skin graft. Pathological analysis of the surgical specimen revealed a tumor measuring 12.6 cm with clear and meager margins lying 1.4 cm from the closest lateral margin and 0.3 cm from the closer deep margin with a histologically confirmed highgrade pleomorphic sarcoma (Figure 2).
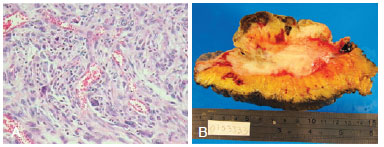
Figure 2 - Histological view of the high-grade pleomorphic sarcoma. In A, microscopic appearance. In B, macroscopic appearance.
The patient was referred for chemotherapy and adjuvant radiotherapy. Isofosfamide (12 mg/m2) and doxorubicin (50 mg/m2) were administered every 3 weeks for 6 months. Radiotherapy was performed with cobalt-60 (60 GY) in 30 fractions concurrently with the chemotherapy.
The patient developed radiodermatitis with ulcerations in the grafted area and underwent new resection and rotation of the left thoracoabdominal fasciocutaneous flap 1 year and 8 months after the first surgery (Figure 3). Pathological examination of this last injury ruled out the presence of neoplasia.
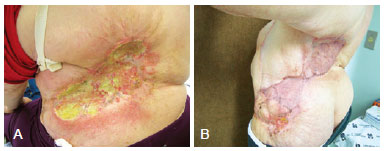
Figure 3 - The patient's back after treatment. In A, radiodermatitis of the treated area. In B, rotation of a local flap and a new skin graft 9 months postoperatively.
The patient remains under regular follow-up of suspicious areas 3 years later, and the disease shows no evidence of recurrence.
DISCUSSION
The incidence of Marjolin's ulcers has decreased due to the prevention and proper management of burns and other wounds, and the performance of debridement of deep areas and adequate coverage1-5. The absence of adequate burn treatment and a healing process consisting of secondary intention are the main risk factors for the development of malignancy1-3.
Close follow-up should be provided for patients from whom biopsies of suspicious areas are taken2-4.
Sarcomas in Marjolin's ulcers should be subjected to the same treatment recommended for the most frequent histological types. There is a need for proper management of these lesions with adequate resection margins and, when required, associated radiotherapy or chemotherapy1,2. The behavior of sarcomas in Marjolin's ulcers is not well established because of the low incidence and paucity of reports in the literature, demonstrating the importance of reporting such findings in an effort to better understand the disease and provide the most appropriate management.
REFERENCES
1. Kowal-Vern A, Criswell BK. Burn scar neoplasms: a literature review and statistical analysis. Burns. 2005;31(4):403-13.
2. Copcu E. Marjolin's ulcer: a preventable complication of burns? Plast Reconstr Surg. 2009;124(1):156e-64e.
3. Kerr-Valentic MA, Samimi K, Rohlen BH, Agarwal JP, Rockwell WB. Marjolin's ulcer: modern analysis of an ancient problem. Plast Reconstr Surg. 2009;123(1):184-91.
4. Agale SV, Kulkarni DR, Valand AG, Zode RR, Grover S. Marjolin's ulcer: a diagnostic dilemma. J Assoc Physicians India. 2009;57:593-4.
5. Alconchel MD, Olivares C, Alvarez R. Squamous cell carcinoma, malignant melanoma and malignant fibrous histiocytoma arising in burn scars. Br J Dermatol. 1997;137(5):793-8.
6. Özyazgan I, Kontas O. Burn scar sarcoma. Burns. 1999;25(5):455-8.
7. Kim GI, Lee JH, Kim HK, Park SH, Kim CH. Malignant fibrous histiocytoma in a chronic burn scar: a rare case report and review of the literature. Burns. 2004;30(7):742-5.
1. Associate member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Plastic Surgeon at St. Joseph Municipal Hospital of Joinville and the Joinville Labiopalatal Injury Rehabilitation Center (Centrinho), Joinville, SC, Brazil
2. General Surgery Resident, St. Joseph Municipal Hospital of Joinville, Joinville, SC, Brazil
Correspondence to:
Gerson de Mattos Ritz Filho
Rua Visconde de Mauá, 1.169 - casa 2 - América
Joinville, SC, Brazil - CEP 89501-204
E-mail: gersonritz@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 30, 2010
Article accepted: January 9, 20
This study was performed at St. Joseph Municipal Hospital of Joinville, Joinville, SC, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter