

Original Article - Year 2013 - Volume 28 -
Improving breast volume assessment in immediate reconstruction using permanent expanders
Aperfeiçoando a mensuração do volume mamário na reconstrução imediata com expansores permanentes
ABSTRACT
BACKGROUND: The accurate determination of breast volume improves the outcome of reconstructive procedures. The aim of the present study is to correlate the preoperative measurement of breast volume using the plastic shells method with the intraoperative application of the Archimedes principle to assess breast volume in immediate breast reconstruction using permanent expanders in patients having breasts with a small volume and mild ptosis grade.
METHODS: Ten patients were enrolled in this retrospective nonrandomized study. Breast volume was measured preoperatively using fixed-volume plastic shells and intraoperatively using the Archimedes method. An appropriate permanent expander was selected and inserted in a retromuscular position. The team classified breast symmetry as poor, good, or very good.
RESULTS: Differences between pre- and intraoperative measurements were statistically significant (P < 0.01, Student's t-test). Preoperative values were lower than intraoperative values by 15% in 70% of the cases.
CONCLUSIONS: Breast volume assessment in immediate reconstruction procedures with permanent expanders can be improved and yield more predictable results by the combined use of different pre- and intraoperative measuring techniques. The method that uses fixed-volume plastic shells tends to underestimate the resected breast volume compared to the intraoperative method that uses the Archimedes principle.
Keywords: Breast. Mammaplasty. Breast implants. Reconstructive surgical procedures. Surgery, plastic.
RESUMO
INTRODUÇÃO: A determinação precisa do volume mamário pode melhorar o resultado dos procedimentos de reconstrução. O objetivo deste estudo é correlacionar a mensuração pré-operatória do volume mamário utilizando o método de conchas plásticas e a aplicação intraoperatória do princípio de Arquimedes para a avaliação volumétrica das mamas, em pacientes submetidas a reconstrução mamária imediata utilizando expansores permanentes, portadoras de mamas de pequeno volume e grau ptótico leve.
MÉTODO: Dez pacientes foram incluídas em um estudo retrospectivo não-randomizado. O volume da mama foi mensurado, no pré-operatório, com conchas plásticas com volumes predeterminados e, no período intra-operatório, com o método de Arquimedes. Expansor apropriado permanente foi selecionado e inserido de maneira retromuscular. A equipe classificou a simetria da mama como pobre, boa ou muito boa.
RESULTADOS: As diferenças entre as medidas pré e intraoperatórias foram estatisticamente significantes (P < 0,01, teste t de Student). Os valores pré-operatórios foram subestimados em 70% dos casos e foram 15% menores que os valores intraoperatórios.
CONCLUSÕES: A avaliação do volume da mama em procedimentos de reconstrução imediata utilizando expansores permanentes pode ser aperfeiçoada pela combinação de diferentes técnicas de mensuração pré e intraoperatórias, levando a resultados mais previsíveis. O método de conchas plásticas de volume preestabelecido tende a subestimar o volume ressecado da mama quando comparado aos valores obtidos com método de mensuração intraoperatória utilizando o princípio de Arquimedes.
Palavras-chave: Mama. Mamoplastia. Implantes de mama. Procedimentos cirúrgicos recons-trutivos. Cirurgia plástica.
Breast reconstruction using implants following mastectomy is an option for women who do not have sufficient subcutaneous tissue available for autologous reconstruction. In addition, many women prefer not to undergo autologous reconstruction due to donor-site morbidity, prolonged recovery periods, and associated muscle weakness. Therefore, muscle and skin tissue expansion has become one of the most popular approaches in breast reconstruction1.
Options for implant-based breast reconstruction include single-stage reconstruction using a standard or adjustable implant, tissue expansion followed by the placement of a permanent implant, or combined autologous tissue/implant reconstruction. The choice of procedure is based on a range of patient variables, including location and type of breast cancer, availability of donor tissue (local, regional, or distant), size and shape of the desired breast, surgical risk, and patient preference2.
The accurate determination of breast volume facilitates reconstructive procedures and helps with the planning of tissue removal in breast reduction surgery. The various methods that are currently used to assess breast size are limited by technical difficulties and unreliable volume determination3.
The aim of the present study is to correlate preoperative measurements of breast volume using the plastic shell method with the intraoperative application of the Archimedes principle to assess breast volume in immediate breast reconstruction using permanent expanders in patients having breasts with small volume and mild ptosis grade.
METHODS
This study was performed according to the principles of the Declaration of Helsinki on medical research involving human subjects and the guidelines and norms regulating research involving human subjects of the Brazilian National Health Council (Resolution CNS 196/96) and was based on the Sociedade Brasileira de Cirurgia Plástica guidelines. Patients signed the informed consent document approved by the Ethics Committee of the Santa Casa de Porto Alegre prior to participating.
Ten private clinic patients were enrolled in this retrospective non-randomized study between 2007 and 2011. Patient inclusion criteria were as follows: women with breast cancer who underwent radical modified mastectomy; an estimated breast volume < 500 mL; and breast ptosis < 2 cm below the inframammary fold. Patient exclusion criteria were as follows: positive lymph node biopsy, adjuvant radiotherapy, and contralateral mastopexy.
The ten patients were diagnosed with breast cancer by the oncology team based on clinical examination and complemented by mammography, mammary ultrasound, and core biopsy findings. Whenever necessary, needle insertion was performed preoperatively to locate the tumor. A preoperative biopsy of the sentinel lymph node was performed in all cases.
Breast volume was measured preoperatively using fixed-volume plastic shells (Figure 1). The surgery procedure was based on a radical modified mastectomy with removal of the skin and fascia covering the muscle. The Archimedes method was applied intraoperatively and involved the total immersion of the mastectomized tissue in a plastic container filled to the top with a 0.9% saline solution (Figure 2). The displaced solution was collected into a second container placed below the first container and was then accurately measured in a 60-mL graduated syringe via needle aspiration.
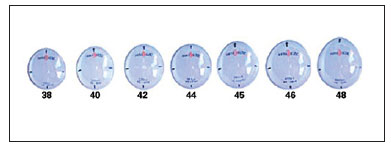
Figure 1 - Mamasizer®: fixed-volume plastic shells used for the preoperative measurement of breast volume. Available at: http://www.sbcp-sc.org.br/anais/42/frame.htm
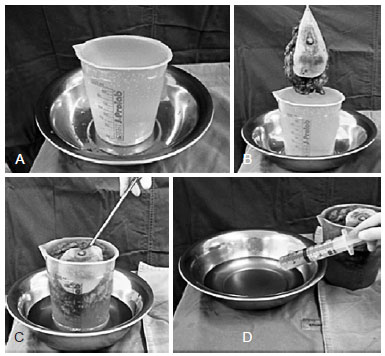
Figure 2 - The Archimedes method. In A, the inner container is filled with 0.9% saline solution and the outer container is ready to receive the displaced liquid when the mastectomized tissue is totally immersed. In B, breast tissue to be immersed within the inner container. In C, mastectomized tissue is immersed in the inner container from which the solution is displaced and collected in the outer container. In D, syringe aspiration for accurate measurement of the liquid displaced after immersion of the breast specimen within the inner container.
A permanent expander was then selected (Menthor® Becker CP 35 permanent expander) and inserted in a retro-muscular position (Figure 3). The filling valve was positioned and final sutures were performed. Suction drains were placed and a small compression dressing was applied.
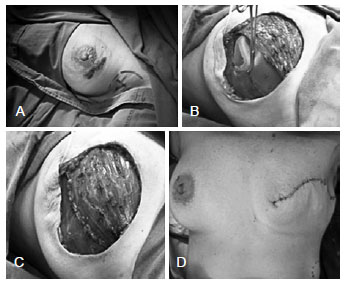
Figure 3 - Intraoperative appearance of the location of the permanent expander in the retromuscular position behind the pectoralis major and serratus muscles. In A, blue dye is injected for sentinel lymph node biopsy. In B, pectoralis major and serratus muscles are mobilized for expander insertion. In C, appearance of the sutured submuscular pocket. In D, final intraoperative appearance.
All cases were documented with photographs and the team classified breast symmetry as poor, good, or very good. Independent evaluators were asked to analyze breast volume and shape as well as the aesthetic appearance of the scar. The analysis was performed 90 days after total filling of the expander and removal of the expander valve prior to reconstruction of the areolar complex.
Pre- and intraoperative breast volumes were compared statistically using the Student's t-test. The relationship between the degree of ptosis and pre- and transoperative volume differences was assessed using the Wilcoxon test.
RESULTS
The mean time for the surgical procedure was 3.5 hours. In all cases, ductal carcinoma in situ was diagnosed based on anatomopathological studies. Use of the Archimedes procedure increased the mean surgical time by approximately 3 minutes.
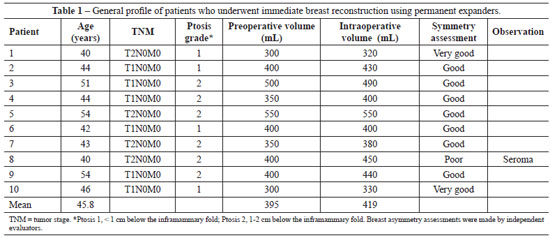
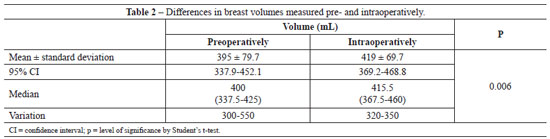
The mean preoperative breast volume measured using the plastic shells method was 395 ml (Table 1). The mean intraoperative breast volume measured using the Archimedes method was 419 ml (Table 1). The difference between the pre- and intraoperative measurements was statistically significant (P < 0.01, Student's t-test). Preoperative values were lower than intraoperative values by approximately 15% in 70% of the cases (Tables 1 and 2). In one case, the preoperative value was 2% higher than the intraoperative value. The difference between the pre- and intraoperative measurements was not related to ptosis grade (breast ptosis < 1 cm below the inframammary fold, P = 0.102; ptosis of 1-2 cm below the inframammary fold, P = 0.078).
The team classified the results as poor, good, or very good in 1, 7, and 2 cases, respectively (Figure 4, Table 1). The results were not related to the degree of ptosis. No serious complications involving loss of the expander were noted. One patient underwent minimal tissue debridement at the scar margin, 1 patient developed recurrent seroma near the axillary lymph node biopsy site, and 1 patient underwent scar revision combined with areolar complex reconstruction. There was no leakage or displacement of the expander during the postoperative follow-up period.

Figure 4 - Aesthetic results of immediate breast reconstruction using permanent expanders and intraoperative volume measurement using the Archimedes method. In A, result classified as very good. In B, result classified as good. In C, result classified as poor.
DISCUSSION
The use of a permanent expander can achieve high levels of patient satisfaction4. However, immediate breast reconstruction using a permanent expander places a great responsibility on the surgeon. The main purposes of the procedure should be to achieve the best possible symmetry and minimize surgical trauma to the patient.
In the present study, we assessed the isolated effect of volume measurement on immediate breast reconstruction using permanent expanders. For this purpose, only patients with small breast volumes and mild ptosis grades who had not undergone contralateral mammaplasty or areolar complex reconstruction were examined. These criteria facilitated the elimination of other variables that could confound the aesthetic results of the transoperative volume assessment using the Archimedes method, and thus, we could optimize single-stage reconstruction using an expander. Patients who underwent radiotherapy or complete axillary node dissection were excluded for the same reason.
Various methods of assessing breast volume in the preoperative period have been described, including plaster casts5, Grossman-Roudner devices6, stereophotogrammetry7,8, three-dimensional imaging9-12, mammography13, and thermoplastic casts14. A method for measuring differences in breast volume based on the Archimedes principle has been described. In this method, a plastic container is placed on the breast of the patient lying in the supine position during the preoperative period. The remaining portion of the container is filled with water and the volume is then measured. This method allows for the measurement of volume differences of asymmetric breasts and helps the surgeon estimate the size of the implant to be used in augmentation mamoplasty15. The same principle has also been used to accurately and intraoperatively calculate the volume of pedicle flaps used in breast reconstruction16.
We believe that the use of the Archimedes principle, as described in the present report, is an accurate method for determining breast volume and leads to more predictable results. Moreover, in procedures in which permanent expanders are used, no additional surgical procedures are required to achieve volume symmetry, thus supporting these findings.
It is generally accepted that a standard method of volume assessment should be used to compare volumes before and after the surgical procedure or between patients and that comparing breast volumes using different methods is not a reliable approach. However, the use of different methods for measuring breast volume pre- and intraoperatively is justified by the suitability of each technique at specific points during treatment. Moreover, plastic shells cannot be used to intra-operatively estimate the volume of the permanent expander. The use of plastic shells is technically more feasible preoperatively and avoids the inconveniences associated with the use of the Archimedes method17. On the other hand, transoperative volume measurements can be made safely and precisely using the Archimedes method without the need for sterilized plastic shells. In addition, the whole surgical sample can be immersed in the liquid.
The results of this study suggest that surgeons should have ready access to permanent expanders in the operating room that are 5-15% larger than the preoperatively measured volume. This difference in volume is probably due to the additional amount of subcutaneous tissue that is removed with the surgical specimen. We suggest that, in patients with a high body mass index, a subcutaneous pinch test can subjectively identify the need to further increase the expander volume. However, further studies are needed to confirm this idea.
The present study has certain limitations, including the lack of a patient satisfaction assessment using a quality-of-life questionnaire.
CONCLUSIONS
Breast volume assessment in immediate reconstruction procedures with permanent expanders can be improved and yield more predictable results by combining different pre- and intraoperative measuring techniques. The method that uses fixed-volume plastic shells tends to underestimate the resected breast volume compared to the intraoperative method using the Archimedes principle.
ACKNOWLEDGEMENTS
The authors thank the plastic surgery resident physicians of the Universidade Federal de Ciências da Saúde, Porto Alegre.
REFERENCES
1. Loustau HD, Mayer HF, Sarrabayrouse M. Pocket work for optimizing outcomes in prosthetic breast reconstruction. J Plast Reconstr Aesthet Surg. 2009;62(5):626-32.
2. Mesbahi AN, McCarthy CM, Disa JJ. Breast reconstruction with prosthetic implants. Cancer J. 2008;14(4):230-5.
3. Sigurdson LJ, Kirkland SA. Breast volume determination in breast hypertrophy: an accurate method using two anthropomorphic measurements. Plast Reconstr Surg. 2006;118(2):313-20.
4. Gui GP, Kadayaprath G, Tan SM, Faliakou EC, Choy C, Ward A, et al. Long-term quality-of-life assessment following one-stage immediate breast reconstruction using biodimensional expander implants: the patient's perspective. Plast Reconstr Surg. 2008;121(1):17-24.
5. Campaigne BN, Katch VL, Freedson P, Sady S, Katch FI. Measurement of breast volume in females: description of a reliable method. Ann Hum Biol. 1979;6(4):363-7.
6. Caruso MK, Guillot TS, Nguyen T, Greenway FL. The cost effectiveness of three different measures of breast volume. Aesthetic Plast Surg. 2006;30(1):16-20.
7. Loughry CW, Sheffer DB, Price TE Jr, Bartfai RG, Morek WM, Lackney MJ, et al. Right and left breast volume and volume distribution comparisons in normal and tumor-containing breasts. Cancer Detect Prev. 1987;10(3-4):215-21.
8. Loughry CW, Sheffer DB, Price TE, Einsporn RL, Bartfai RG, Morek WM, et al. Breast volume measurement of 598 women using biostereometric analysis. Ann Plast Surg. 1989;22(5):380-5.
9. Kovacs L, Eder M, Hollweck R, Zimmermann A, Settles M, Schneider A, et al. New aspects of breast volume measurement using 3-dimensional surface imaging. Ann Plast Surg. 2006;57(6):602-10.
10. Kovacs L, Eder M, Hollweck R, Zimmermann A, Settles M, Schneider A, et al. Comparison between breast volume measurement using 3D surface imaging and classical techniques. Breast. 2007;16(2):137-45.
11. Eder M, Schneider A, Feussner H, Zimmermann A, Höhnke C, Papa-dopulos NA, et al. Breast volume assessment based on 3D surface geometry: verification of the method using MR imaging. Biomed Tech. 2008;53(3):112-21.
12. Tepper OM, Unger JG, Small KH, Feldman D, Kumar N, Choi M, et al. Mammometrics: the standardization of aesthetic and reconstructive breast surgery. Plast Reconstr Surg. 2010;125(1):393-400.
13. Kalbhen CL, McGill JJ, Fendley PM, Corrigan KW, Angelats J. Mammo-graphic determination of breast volume: comparing different methods. AJR Am J Roentgenol. 1999;173(6):1643-9.
14. Bulstrode N, Bellamy E, Shrotria S. Breast volume assessment: comparing five different techniques. Breast. 2001;10(2):117-23.
15. Tezel E, Numanoglu A. Practical do-it-yourself device for accurate volume measurement of breast. Plast Reconstr Surg. 2000;105(3):1019-23.
16. Chang KP, Lin SD, Hou MF, Lee SS, Tsai CC. Measurement of the volume of the pedicled TRAM flap in immediate breast reconstruction. Ann Plast Surg. 2001;47(6):594-601.
17. Schonauer F, Singh S, La Rusca I, Molea G. Preoperative sizing and breast asymmetry. Plast Reconstr Surg. 2011;127(2):1005-6.
1. Plastic Surgeon, full member of Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Managing Associate of Webster Cirurgia Plástica, Invited Professor at the Serviço de Cirurgia Plástica e Microcirurgia da Santa Casa de Misericórdia de Porto Alegre of the Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil
2. Resident Physician of the Serviço de Cirurgia Plástica e Microcirurgia da Santa Casa de Misericórdia de Porto Alegre e da UFCSPA, Aspiring Member in Training of the SBCP, Porto Alegre, RS, Brazil
3. Plastic Surgeon, Full Member of the SBCP, Adjunct Professor at the Serviço de Cirurgia Plástica e Microcirurgia da Santa Casa de Misericórdia de Porto Alegre e da UFCSPA, Porto Alegre, RS, Brazil
Correspondence to:
Ronaldo Webster
Rua Mariano de Mattos, 718
Porto Alegre, RS, Brazil - CEP 90880-250
Email: lwebstercplastica@me.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: October 2, 2012
Article accepted: December 23, 2012
This study was performed at the Serviço de Microcirurgia Reconstrutiva e Cirurgia Plástica da Santa Casa de Porto Alegre - Paulo Roberto Franco Azambuja, Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter