

Original Article - Year 2013 - Volume 28 -
Deepithelialized thoracodorsal flap: a new concept for autologous breast reconstruction
Retalho toracodorsal desepitelizado: um novo conceito para a reconstrução autóloga da mama
ABSTRACT
BACKGROUND: The association the thoracodorsal muscular flap with a thoracic fascio-cutaneous extension results in a large flap, that allowed to cover the mastectomy residual skin defect. The purpose of this study is to share 11 year experience with a new concept in autologous breast reconstruction using a deepithelialized thoracodorsal skin flap pedicle with the latissimus dorsi muscle as vector.
METHODS: A retrospective study of 247 operated patients from 1999 to 2009 was performed. Parameters of interest included age, body mass index, smoking, radiation and chemotherapy histories, breast size, flap dimensions, operative time, breast tissue expansion and complication rates. The thoracodorsal flap design under an ellipse shape extends from near the mid dorsal line extended up to the mid-infra-mammary line with maximal width at the mid axillary line. The deepithelialized fascio-cutaneous extension is lumped together with the latissimus dorsi as its vehicle and blood supply pedicle, together are brought to the neo-mammary previous dissected skin area. Gradual as a tissue expansion the breast shape and projection are restored.
RESULTS: Immediate and delayed breast reconstructions were done in 14.5% and 85.5%, respectively. Bilateral breast reconstruction was done in 9% of the patients. Implants were not used for reconstruction purposes in any of the 77% of the patients received breast radiotherapy. The average operative time was 2 hours and 20 minutes. Expansion of non irradiated breast skin occurred over a three months period, whereas that of irradiated skin took an average of five months following delayed reconstruction. The complication rate was 11.4%. No total flap loss was reported. The seroma rate was 7% after the drains had been removed. The mean hospital stay was 3 days. Contra lateral breast remodeling was performed in 92% of the cases and fat grafting in 14% of the cases. With an average follow-up of 4 years, patient satisfaction was rated high by the patients.
CONCLUSIONS: The thoracodorsal flap is a safe and reliable surgical option for autologous breast reconstruction. Its main advantages achieving large breast volumes circumventing the use of prosthetic material, avoiding the patch look on the reconstructive breast, achieving tissue expansion, while insuring acceptable donor site morbidity.
Keywords: Breast/surgery. Mammaplasty/methods. Surgical flaps.
RESUMO
INTRODUÇÃO: A associação de retalho muscular toracodorsal com uma extensão fasciocutânea resulta em um amplo retalho, que permite recobrir o defeito cutâneo residual da mastectomia. O objetivo deste estudo é compartilhar 11 anos de experiência com um novo conceito em reconstrução autóloga da mama, utilizando um retalho cutâneo toracodorsal desepitelizado pediculado com músculo grande dorsal como vetor.
MÉTODO: Foi realizado um estudo retrospectivo com 247 pacientes operadas de 1999 a 2009. Os parâmetros de interesse incluíram idade, índice de massa corporal, história de tabagismo, radioterapia e quimioterapia, tamanho da mama, dimensões do retalho, tempo cirúrgico, expansão do tecido mamário e índice de complicações. O desenho do retalho toracodorsal em formato de elipse se estende da região da linha dorsal média até a linha inframamária média, com largura máxima na linha axilar média. A extensão fasciocutânea desepitelizada é colocada dissecada juntamente com o músculo grande dorsal como seu veículo e pedículo responsável pelo suprimento sanguíneo, que são levados em monobloco até a área de pele da nova neomama previamente dissecada. O formato e a projeção da mama são restaurados gradualmente como uma expansão de tecido.
RESULTADOS: Reconstruções imediata e tardia da mama foram realizadas em 14,5% e 85,5% das pacientes, respectivamente. A reconstrução bilateral da mama foi realizada em 8,9% das pacientes. Nenhuma das pacientes submetidas a radioterapia mamária (76,7%) recebeu implantes para reconstrução. O tempo cirúrgico médio foi de 2 horas e 20 minutos. A expansão da pele mamária não irradiada foi realizada em um período de 3 meses, enquanto a expansão da pele irradiada levou um período médio de 5 meses após a reconstrução tardia. A taxa de complicações foi de 11,3%. Não houve perda total do retalho. A taxa de seroma foi de 7% após a remoção dos drenos. O tempo de hospitalização médio foi de 3 dias. Foi realizado remodelamento da mama contralateral em 92% dos casos e enxerto de gordura em 14% das pacientes. Em um período médio de acompanhamento de 4 anos, a taxa de satisfação das pacientes foi elevada.
CONCLUSÕES: O retalho toracodorsal é uma opção cirúrgica segura e confiável para a reconstrução autóloga da mama. As principais vantagens são a obtenção de grandes volumes de mama contornando o uso de material protético, evitando-se a aparência de retalho na mama reconstruída, obtendo-se expansão tecidual e, ao mesmo tempo, garantindo morbidade aceitável no sítio doador.
Palavras-chave: Mama/cirurgia. Mamoplastia/métodos. Retalhos cirúrgicos.
Following the first description of the latissimus dorsi flap by Tansini, in 1896, its use fluctuated with renewed enthusiasm in the 1970s after the improved understanding of cutaneous-muscle flaps1,2. The latissimus dorsi remained the workhorse flap in breast reconstructive surgery until the introduction of the transverse rectus abdominus myocutaneous (TRAM) flap in 1982, couplet with the increased exploitation of free and perforator flaps3-6. Becoming a secondary choice for breast reconstruction, modifications of the latissimus dorsi muscle flap, in order to revive its use, reemerged over the last three decades5-17. Despite different modifications that were brought to the latissimus dorsi muscle flap, major limitations included the persistence of patch look, in delayed reconstructions, due to the restricted amount and pliability of available skin over the treated breast. Moreover, the limited bulk volume provided by harvested flap dictated the need for alloplastic implants in order to achieve the desired volumes. Based in this context, combining the thoracodorsal muscular flap with a thoracic fascio-cutaneous extension, a large flap allowed to cover the mastectomy residual skin defect. The major key point is to avoid the use of addition implant.
The purpose of this study is to share 11 year experience with a new concept in autologous breast reconstruction using a deepithelialized thoracodorsal skin flap pedicle with the latissimus dorsi muscle as vector.
METHODS
We performed a retrospective review of the database to identify patients who underwent thoracodorsal flap reconstruction following mastectomy between 1999 to 2009. All cases were performed by the same senior surgeon. Parameters of interest included age, body mass index (BMI), smoking as well as radiation and chemotherapy history, breast size, flap dimensions, operative time, breast tissue expansion and different complications were considered and evaluated.
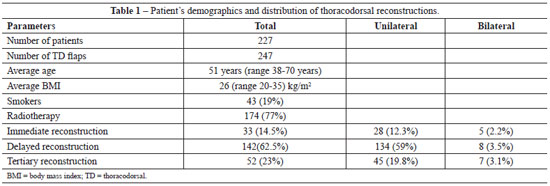
The patients ranged from 38 to 70 years old, with an average of 51 years, the BMI varied between 20 kg/m2 to 3 5 kg/m2 (average 26 kg/m2). Forty three (19%) of the patients were active smokers.
The main indications for the thoracodorsal muscular flap included patients' preference for autologous reconstruction with contraindications for abdominal flap, patients' rejection for the patch look over the reconstructed breast, failed previous treatment modalities including other types of autologous reconstruction in addition to prosthetic implants.
Patient population included those who underwent immediate or delayed, uni or bilateral reconstruction in addition to prosthetic implants, with or without radiotherapy and or breast implants.
Exclusion criteria included severe skin damage secondary to breast radiotherapy, whereby damaged breast skin had to be excised, and lost follow-up before one year postoperatively. Data was integrated and analyzed in a computerized database (Table 1).
Flap Skin Demarcation
The flap is designed in an elliptical transverse shape with the patient standing. The ellipse extends two to three centimeters lateral to the back midline up to the mid infra-mammary fold. The upper half segment of the skin demarcations remains on the latissimus dorsi projection and the lower half at the serratus and oblique muscles projections. The largest flap dimension is at the mid axillary line (Figure 1). The pinch test is used to estimate the width of the flap.
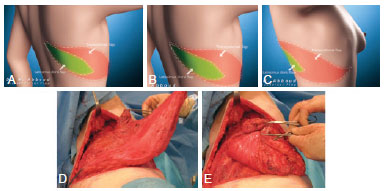
Figure 1 - In A, B and C, schematic aspects of the demarcation of the latissimus dorsi muscle flap and latissimus dorsi integrated into a monoblock. The cutaneous flap is deepithelialized along its entire length, about 35 cm in length, and the "pinch test" in the transverse direction varies between 12 cm and 15 cm. In D and E, extent of resection of the latissimus dorsi muscle near the neck of the humerus to its mobilization.
The neurovascular supply to the cutaneous and latissimus dorsi flaps receives from the terminal branch of the sub-scapular artery, which itself is a branch of the third portion of the sub-scapular artery. This sub-scapular artery also divides into the scapular circumflex and thoracodorsal arteries. The last one, once penetrate the muscle and run parallel to the muscle fibers and their perforating vessels, supply the entire skin over it. The tendon insertion of the latissimus can be sectioned at the humerus insertion without damage of the bundle.
Surgical Technique
The patients are operated on lateral position with the upper-arm abducted 90 degrees, under general anesthesia with tracheal intubation. Skin incision is performed all along the previous demarcations and deepitheliazation in all its extension, except in the cases of immediate breast reconstruction in order to preserve a small skin segment for the nipple areola complex reconstruction in the same stage.
Skin dissection expose the latissimus dorsi witch is dissected in all the extension and in all cases its tendon is sectioned. Latissimus dorsi muscle and the deepithelialized skin flap remain connected with the vascular frame preserved and the nerve also intact. The two dermal flap extremities and the latissimus dorsi segments containing its tendon are sutured together by two to three isolated non absorbable stitches in a lumped aspect and rotated 180 degrees. From the same donor site incision, access dissection to the breast is performed and the pocket created for the flap be inserted. Scoring of the scar tissue and or capsulectomy is performed when necessary at this stage. The flap is then inserted into the pocket and fixed to the inframammary fold using simple suture. The apex of the flap containing the muscular tendon is also pulled towards and fixed at the tail of the breast to avoid possible tension. Three suction drains are placed at the thorax, axillary and thoracic regions. The donor wound edges are sutured by isolated stitches in multilayer planes. The patients are turned to supine position and the flap skin paddle is exteriorized to reconstruct the nipple areola complex. Final skin suture is applied at the lateral aspect of the beast, and a sterile dressing covers it. Patients are asked to wear a compressive bra 48 hours following the surgery and a usual type for 1 to 3 months.
Figures 2 to 7 illustrate the technique described in the present article.
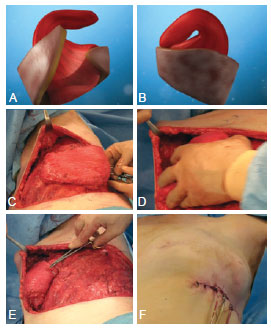
Figure 2 - In A and B, schematic and anatomical aspect of the dermo-muscular flap and the free segment of the dorsal muscle in monobloc, sutured the edges. In C, aspect of the flap rotated 180º, followed by its inclusion in the region of cutaneous pocket of the neomama previously dissected in its entire area. In D, introduction offlap mobilized in the recipient bed. In E, isolated points with non-absorbable thread set to dermal face of the flap to the serratus muscle. In F, the appearance of cutaneous suture and placement of 3 suction drains, one in the axilla and the other two in the dissected chest region.

Figure 3 - Case of breast cancer on the left, 4 years after reconstruction with TRAM flap for treatment of cancer of the right breast. In A, preoperative appearance of a patient underwent to reconstruction with TRAM flap on right breast, front view. In B, postoperative aspect 1 year after the procedure, front view. In C to H, postoperative aspect of patient underwent to reconstruction with thoracodorsal flap in left breast in the 5-year follow-up, front view (C), with raised arms (D), in right profile (E), in left profile (F, G), and oblique left position (H).

Figure 4 - In A to C, preoperative aspect of a patient underwent to bilateral delayed breast reconstruction using implants with history of radiation therapy in both breasts. In D to F, appearance 3 years after removal of 2 implants and breast reconstruction with bilateral thoracodorsal flaps, without implants. In G and H, intraoperative aspect showing the volume provided by the flap doubling the size of the implant.
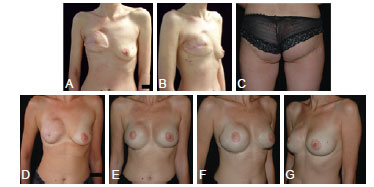
Figure 5 - In A and B, preoperative aspect of patient that had failure of the right breast reconstruction with free bilateral gluteal flaps, prosthetic reconstruction with secondary capsular contracture. Patient underwent to radiotherapy to the right breast. In C, appearance of the donor site for first reconstruction. In D to G, aspect 4 years after implant removal and right breast reconstruction with thoracodorsal flap, followed by bilateral increase with prosthesis subsequently performed.

Figure 6 - In A to E, preoperative aspect of patient underwent to delayed reconstruction of the right breast with thoracodorsal flap in breast cancer previously treated with radiotherapy. In F to J, 5 years postoperative aspect. In K to M, comparison between preoperative (K) and postoperative (L and M) aspects, demonstrating that the donor site scar is hidden in the bra line.
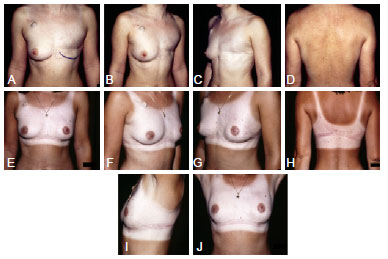
Figure 7 - In A to D, preoperative aspect of patient underwent to delayed reconstruction of the left breast with thoracodorsal flap. The patient had undergone radiotherapy to the left breast. In E to J, 2 years postoperative aspect.
RESULTS
The total number of thoracodorsal flaps was 247 performed for 227 patients, after excluding lost follow-up before the first postoperative year (9 patients, 3.9%) , as well as patients with severe skin problems by secondary breast radiotherapy, whereby damaged skin had to be excised (7 patients, 3.1%). The patients' population was a combination of those who underwent immediate reconstruction (14.5%), delayed reconstruction (85.5%), unilateral (91%) or a total of 20 (8.8%) bilateral breast reconstruction. 52 patients had been previously reconstructed with breast implants. The latter were removed in all the cases and replaced by the thoracodorsal flaps. A total of 174 (77%) patients had received breast radiotherapy.
The flap dimensions ranged between 11 cm to 16 cm for the vertical with and 32 cm to 43 cm for the horizontal lengthening, with an average of 13 and 38 respectively. The majority of the obtained breasts were of cup C, ranging from B to D. The average time of the surgery was 2 hours and 20 minutes, ranging 2 hours to 3 hours (Table 2).
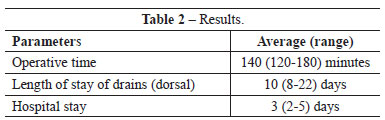
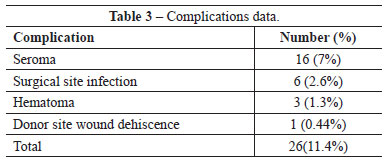
The overall complication rate was 11.4% in this series. No flap losses were recorded. The complications comprised 16 (7%) seroma, 6 (2.6%) wounds infection, 3 (1.3%) hematomas and one (0.44%) donor wound dehiscence, all treated conservatively (Table 3). The hospital stay duration varied between two and five days with a mean of three days. The thoracic and axillary drains were removed between day 3 and 7 post operatively (average 4 days). The dorsal drain was kept for 8 days to 22 days postoperatively (average 10 day). The average follow-up period was 4 years, ranging between 1 to 10 years. Contra lateral breast remodeling in the form of mastopexy, reduction or simple breast liposuction was performed in 92% of the cases, lipo-filing of the reconstructed breast was done in 14% of the cases.
No prosthesis was used for reconstructive purposes. However bilateral breast implants were placed for 41 (18%) patients upon patients' desire, only to augment their breast volumes as a secondary cosmetic procedure after autologous reconstruction.
DISCUSSION
The latissimus dorsi flap remains a versatile tool in breast reconstructive surgery, nonetheless the limited bulk as well as the persistence of the patch effect over the reconstructed breast constitute its main pitfalls. Many authors tried to resolve this by bringing modifications to the latissimus dorsi flap6-18. In 1983, a procedure was described with the latissimus dorsi total flap muscle was harvested with a large skin paddle8. Completely or partially detaching the latissimus dorsi tendon from its humeral attachment facilitates the rotation and position of the flap with less bulkiness at the axilla9,13,19,20. We have observed that by lumping the muscle together intra-operatively using simple stitches; we do not only insure a bulkier breast but also decrease the forces of muscular contractions. We agree with others authors who have advocated for fixing the flap to the chest wall to decrease the tension on the pedicle13,20. In fact, we didn't observe any sequels such as twisting or excessive tension affecting the viability of the flap. Pitfalls to this maneuver certainly exist and comprise bothersome muscular contraction, that will however decrease with time13,19,21.
Our seroma rate was low compared to that of the literature9,10,11,13. This is explained by the fact that seroma we recorded when occurring after removal of the drains. Despite the use of several known maneuvers to decrease the seroma rate, including quilting sutures and multilayer tension free closure of the donor site, the drains had to be kept for an average of 10 days, and seroma still occurred.
Similar to other surgical techniques, the latissimus dorsi flap presents its own drawbacks. The extended donor site scar and the slight back contour deformity constitute the main limitations to this surgical modality. In addition, burial of the totality of the flap in delayed reconstruction hampered monitoring of parameters such as venous congestion among other short term complications. This did not constitute a major obstacle, since there weren't any total flap losses in the study group. Contraindications to this technique include previous thoracotomy at the side of reconstruction, as well as severely damaged skin secondary to considerable radiation doses hampering proper tissue expansion.
CONCLUSIONS
The thoracodorsal flap is a safe and reliable surgical technique with a wide range of applications in breast reconstruction following mastectomy with or without radiation. Besides it imposing as a salvage flap when other treatment modalities fail, its main advantages include achieving adequate breast volumes avoiding the use of prosthetic material, improving the skin quality mainly following radiation and achieving considerable tissue expansion without the need of expanders while insuring minimal donor site mobility. The thoracodorsal flap is a good surgical option for breast reconstruction following mastectomy mainly for the irradiated breast.
REFERENCES
1. Mathes SJ, Nahai F. Clinical atlas of muscle and musculocutaneous flaps. St Louis: Mosby; 1980.
2. Schneider WJ, Hill HL Jr., Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg. 1977;30(4):277-81.
3. Fujino T, Harashina T, Enomoto K. Primary breast reconstruction after a standard radical mastectomy by a free flap transfer. Case report. Plast Reconstr Surg. 1976;58(3):371-4.
4. Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989;42(6):645-8.
5. Marshall DR, Anstee EJ, Stapleton MJ. Soft tissue reconstruction of the breast using an extended composite latissimus dorsi myocutaneous flap. Br J Plast Surg. 1984;37(3):361-8.
6. Barnett GR, Gianoutsos MP. The latissimus dorsi added fat flap for natural tissue breast reconstruction: report of 15 cases. Plast Reconstr Surg. 1996;97(1):63-70.
7. Hokin JA. Mastectomy reconstruction without a prosthetic implant. Plast Reconstr Surg. 1983;72(6):810-8.
8. Hokin JA, Silfverskiold KL. Breast reconstruction without an implant: results and complications using an extended latissimus dorsi flap. Plast Reconstr Surg. 1987;79(1):58-66.
9. Papp C, Zanon E, McCraw J. Breast volume replacement using the de-epithialized latissimus dorsi myocutaneous flap. Eur J Plast Surg. 1988;11(3):120-5.
10. McCraw JB, Papp CT. Latissimus dorsi myocutaneous flap: "fleur-de-lis" reconstruction. In: Hartrampf CR, ed. Breast reconstruction with living tissue. Norfolk: Hampton Press; 1991. p.221.
11. Aitken ME, Mustoe TA. Why change a good thing? Revisiting the fleur-de-lis reconstruction of the breast. Plast Reconstr Surg. 2002;109(2):525-38.
12. Germann G, Steinau HU. Breast reconstruction with the extended latissimus dorsi flap. Plast Reconstr Surg. 1996;97(3):519-26.
13. Chang DW, Youssef A, Cha S, Reece OR Autologous breast reconstruction with the extended latissimus dorsi flap. Plast Reconstr Surg. 2002;110(3):751-61.
14. Rifaat MA, Amin AA, Bassiouny M, Nabawi A, Monib S. The extended latissimus dorsi flap option in autologous breast reconstruction: a report of 14 cases and review of the literature. Indian J Plast Surg. 2008;41(1):24-33.
15. Heitmann C, Relzer M, Kuentscher M, Menke H, Oermann O. The extended latissimus dorsi flap revisited. Plast Reconstr Surg. 2003;111(5):1697-701.
16. Hudson DA, Ndobe E. Using two flaps to achieve aesthetic autologous breast mound reconstruction. Ann Rlast Surg. 2002;49(2):189-92.
17. Delay E, Jorquera F, Pasi P, Gratadour AC. Autologous latissimus breast reconstruction in association with the abdominal advancement flap: a new refinement in breast reconstruction. Ann Plast Surg. 1999;42(1):67-75.
18. Menke H, Erkens M, Olbrisch RR. Evolving concepts in breast reconstruction with latissimus dorsi flaps: results and follow-up of 121 consecutive patients. Ann Rlast Surg. 2001;47(2):107-14.
19. Delay E, Gounot N, Bouillot A, Zlatoff P, Rivoire M. Autologous latissimus breast reconstruction: a 3-year clinical experience with 100 patients. Rlast Reconstr Surg. 1998;102(5):1461-78.
20. McCraw JB, Papp C, Edwards A, McMellin A. The autogenous latissimus breast reconstruction. Clin Rlast Surg. 1994;21(2):279-88.
21. Slavin SA. Improving the latissimus dorsi myocutaneous flap with tissue expansion. Rlast Reconstr Surg. 1994;93(4):811-24.
1. Plastic surgeon, head of the Plastic Surgery Department of the Centre Hospitalier Universitaire de Tivoli, La Louvière, Belgium
2. Plastic surgeon of the American University of Beirut, Surgery Department, Division of Reconstructive and Aesthetics Plastic Surgery, Beirut, Lebanon
3. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery, editor-in-chief of the Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery, Campinas, SP, Brazil
Correspondence to:
Marwan Abboud
Rue du Magistrat, 7
Bruxelles, Belgique - 1000
E-mail: info@maclinic.eu
Article submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 8, 2013
Article accepted: March 22, 2013
This study was performed at private clinics of the principal author, Brussels, Belgium.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter