

Original Article - Year 2013 - Volume 28 -
Breast reconstruction procedures: a 10-year retrospective study
Reconstruções mamárias: estudo retrospectivo de 10 anos
ABSTRACT
INTRODUCTION: Breast cancer is a major global health problem with a gradually increasing incidence. Mastectomy and adjuvant therapies may result in physical complications and psychological disorders that lead several women to consider surgical reconstruction in order to reduce negative feelings, improve self-esteem, and be provided with a new breast. The aim of this study is to analyze a series of breast reconstruction procedures performed over a period of 10 years in the first author's private clinic in patients who underwent mastectomy for breast cancer removal.
METHODS: We analyzed the medical records of patients who underwent breast reconstruction between January 2002 and December 2011.
RESULTS: In the period considered, 428 breast reconstruction procedures were performed in patients who underwent mastectomy for breast cancer removal. The average patient age was 52.77 years. With regard to the type of reconstruction, 134 procedures were performed using the rectus abdominis muscle flap (TRAM); 105, using conservative techniques; 87, using the latissimus dorsi muscle flap (LDMF); 76, using prostheses; and 26, in secondary procedures. Before October 2007, the percentage of bilateral surgeries, including the use of TRAM and LDMF, was 30%. After October 2007, this percentage increased to 84%. The complication rate was 33.41%.
CONCLUSIONS: Breast reconstruction procedures are safe with limited complications that increase according to the presence of risk factors. The increased incidence of bilateral surgeries performed during recent years was attributed to the increased incidence of prophylactic mastectomy performed on the contralateral breast to reduce the risk of cancer and facilitate mammary symmetrization.
Keywords: Mammaplasty. Breast/surgery. Breast neoplasms. Surgical flaps.
RESUMO
INTRODUÇÃO: O câncer de mama é um dos principais problemas de saúde do mundo e sua incidência vem aumentando gradativamente. A mastectomia e as terapias adjuvantes contribuem para o desenvolvimento de complicações físicas e transtornos psicológicos. Na tentativa de reduzir os sentimentos negativos, melhorar a autoestima e suprir a falta da mama, pode-se optar pela reconstrução cirúrgica. O objetivo deste estudo foi analisar os casos de reconstrução mamária pós-mastectomia por câncer de mama, realizados em um período de 10 anos, na clínica privada do autor principal.
MÉTODO: Foi realizada revisão dos prontuários de pacientes submetidas a reconstrução mamária, no período de janeiro de 2002 a dezembro de 2011.
RESULTADOS: No período analisado, foram realizadas 428 reconstruções mamárias em pacientes mastectomizadas por câncer de mama. A média de idade das pacientes foi de 52,77 anos. Quanto ao tipo de reconstrução, 134 procedimentos foram realizados com retalho do músculo reto abdominal (TRAM), 105 com técnicas conservadoras, 87 com retalho do músculo grande dorsal (RGD), 76 com próteses e 26 secundárias. Previamente a outubro de 2007, a porcentagem de cirurgias bilaterais, somando-se TRAM e RGD, era de 30%; a partir desse período, a porcentagem passou para 84%. A taxa de complicações foi de 33,41%.
CONCLUSÕES: As técnicas de reconstrução mamária são alternativas seguras, com taxas de complicação aceitáveis. A presença de fatores de risco resultou em maior taxa de complicações e evidenciou-se aumento da incidência de cirurgias bilaterais nos últimos anos, fato atribuído ao aumento das mastectomias profiláticas na mama contralateral ao tumor, o que pode reduzir o risco da neoplasia e facilitar a simetrização mamária.
Palavras-chave: Mamoplastia. Mama/cirurgia. Neoplasias da mama. Retalhos cirúrgicos.
Currently, breast cancer is a major global health problem, with a gradual increase in incidence in Brazil. This neoplasia primarily affects women. There were a total of 1.4 million new cases of breast cancer in 2008, accounting for 23% of all cancer cases. In 2012, a study estimated that 52 women in every 100,000 are at risk of developing breast cancer. Every year, approximately 22% of new cancers that develop in women occur in the breast1.
Mastectomy is among the more common treatments for breast cancer. However, surgery and adjuvant therapies may cause physical complications2 and psychological disorders3, thereby negatively affecting a patient's quality of life4. Mastectomy, that is, surgical breast removal, alters the female body image and causes feelings of mutilation as well as loss of femininity and sensualitity5. Such feelings lead several women to consider surgical reconstruction in an attempt to reduce negative feelings, improve self-esteem, and be provided with a new breast6. Breast reconstruction is a safe procedure that does not increase the risk of disease recurrence and does not interfere or delay the detection of cancer due to adjuvant therapies. The reconstruction procedures described so far involve the use of conservative techniques, neighboring flaps, alloplastic materials, and pedicled and microsurgical myocutaneous flaps7,8.
With the advent of genetic testing for the BRCA1 and BRCA2 genes for the purpose of risk stratification, contralateral prophylactic mastectomy is frequently performed in patients who have previously undergone mastectomy for unilateral cancer removal9,10. In addition, other factors may contribute to the performance of prophylactic mastectomy, such as multiple mammaplasty alterations, multicenter precursor lesions, difficulty in screening dense breast tissue, and high levels of patient anxiety11.
The aim of this study is to analyze a series of breast reconstruction procedures performed over a period of 10 years in the first author's private clinic in patients who underwent mastectomy for breast cancer removal. The patients were classified according to age, type of surgery performed (technique used and unilateral vs. bilateral procedure), complications, correlation between risk factors and increased complication rates, and technique improvement.
METHODS
Were analyzed the medical records of patients who underwent breast reconstruction between January 2002 and December 2011. We collected information on patient age, breast reconstruction type (unilateral or bilateral), and postoperative complications. Moreover, information about which risk factors may increase the complication rate (comorbidities, smoking, obesity, and radiotherapy) was also obtained by analyzing the medical records of the patients who underwent reconstruction after October 2007.
RESULTS
Between January 2002 and December 2011, 428 breast reconstruction procedures were performed in patients who underwent mastectomy for breast cancer removal. The average patient age was 52.77 years (range, 27-79 years).
A total of 134 breasts were reconstructed using a myocutaneous rectus abdominis muscle flap (TRAM); 105, using conservative procedures (local and neighboring flaps); 87, using a myocutaneous latissimus dorsi muscle flap (LDMF); 76, using prostheses (pectoralis major muscle flap extended with an inferior-based dermal-fat pedicle flap to cover the implant); and 26, in secondary procedures in cases requiring further reconstruction due to an unsuccessful outcome after the first procedure (Figures 1-6).
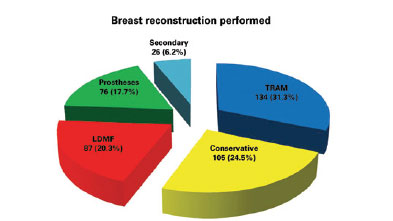
Figure 1 - Number of breast reconstruction procedures performed between January 2002 and December 2011 according to procedure type. LDMF = myocutaneous latissimus dorsi muscle flap; TRAM = myocutaneous rectus abdominis muscle flap.
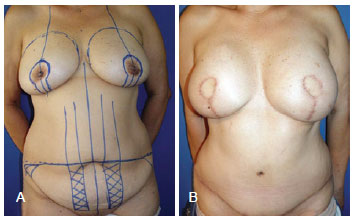
Figure 2 - Breast reconstruction performed using a myocutaneous rectus abdominis muscle flap. In A, preoperative surgical marking. In B, postoperative appearance.
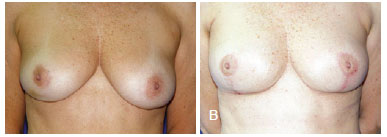
Figure 3 - Breast reconstruction performed using a conservative procedure (mammaplasty technique). In A, preoperative appearance. In B, postoperative appearance.
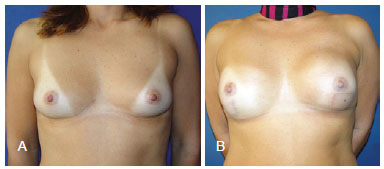
Figure 4 - Breast reconstruction performed using a latissimus dorsi myocutaneous flap. In A, preoperative appearance. In B, postoperative appearance.
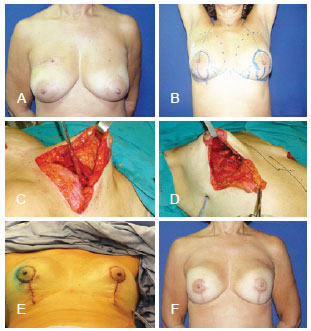
Figure 5 - Breast reconstruction performed using prostheses. In A, preoperative appearance. In B, preoperative surgical marking. In C and D, intraoperative appearance of the pectoralis major muscle extended with the inferior-based dermal-fat pedicle flap to cover the implant. In E, immediate postoperative appearance. In F, late postoperative appearance.
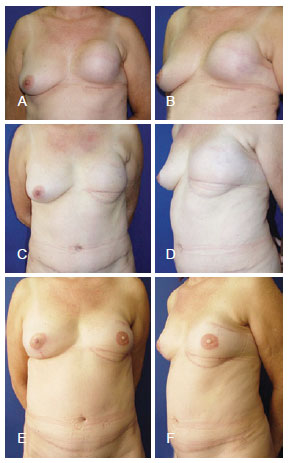
Figure 6 - Secondary breast reconstruction. In A and B, postoperative appearance 6 months after left mastectomy with prostheses reconstruction had an unsatisfactory outcome. In C and D, postoperative appearance 9 months after a secondary breast reconstruction was performed using a myocutaneous rectus abdominis muscle flap. In E and F, appearance 1 year and 2 months after a secondary reconstruction was performed to achieve nipple reconstruction and contralateral mammary symmetrization.
Among the TRAM procedures performed, 70 were unilateral (42 immediate and 28 late) and 64 were bilateral (50 immediate, 5 late, and 9 immediate on one side and late on the other). Among the LDMF procedures, 25 were unilateral (15 immediate and 10 late) and 62 were bilateral (56 immediate, 2 late, and 4 immediate on one side and late on the other) (Figure 7).
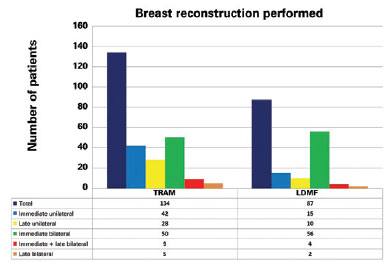
Figure 7 - Different types of breast reconstruction procedures performed between January 2002 and December 2011. LDMF = myocutaneous latissimus dorsi muscle flap; TRAM = myocutaneous rectus abdominis muscle flap.
Before October 2007, the percentage of bilateral surgeries involving the use of TRAM and LDMF was 30%. Thereafter, the percentage increased to 84% (Figure 8). During the period analyzed in this study, 57.01% of the TRAM and LDMF procedures were bilateral, whereas 42.99% were unilateral.
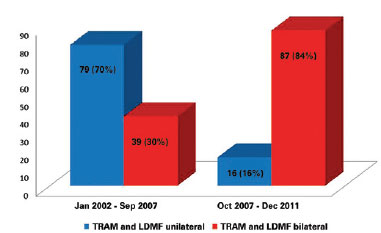
Figure 8 - Analysis of procedures using TRAM and LDMF (unilateral or bilateral) performed during the study period.
A total of227 complications were encountered, associated with 143 of the 428 reconstruction procedures (33.41%) (Table 1). The assessment of risk factors in the latter 135 reconstructions (performed from October 2007 to December 2011) revealed that 19 patients were obese (body mass index > 30), 18 were smokers, 10 had previously undergone radiotherapy, and 50 had comorbidities (diabetes, hypertension, or hypothyroidism). In this group, 56 (41.4%) patients experienced several complications. The presence of at least 1 risk factor was observed in 41 (73.2%) patients (Figure 9). Twelve of the 18 (67%) smokers experienced complications.
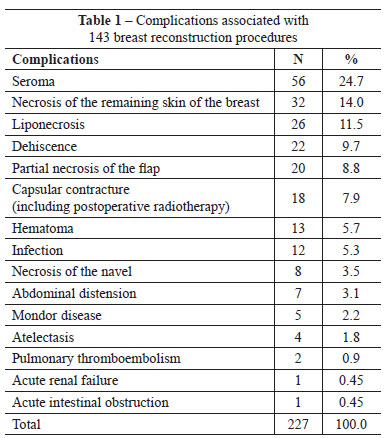
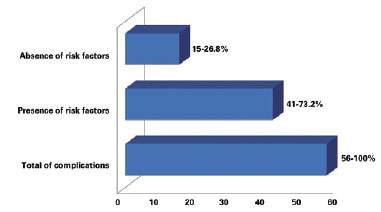
Figure 9 - Number of complications in the latter 135 breast reconstruction procedures classified according to the presence or absence of risk factors.
DISCUSSION
Breast reconstruction plays an important role in the management of patients with breast cancer. Taking a decision on the necessity of breast reconstruction, the appropriate procedure, and best time for this intervention requires a multi-disciplinary approach involving patients, plastic surgeons, and mastology and oncology teams12.
The incidence ofbilateral surgeries was higher in the last 4 years of the analyzed period than in the prior years, although in cases of unilateral cancer, the high incidence of bilateral surgeries was attributed to patient interest in contralateral prophylactic mastectomy. In this study, between January 2002 and September 2007, the percentage of bilateral TRAM and LDMF procedures was 30%, whereas this percentage increased to 84% between October 2007 and December 2011. It is estimated that more than 10% of women who are treated for primary cancer will develop contralateral breast cancer up to 30 years later13. The efficacy of prophylactic mastectomy depends on the ability to remove most of the breast tissue and leave a flap with minimal thickness. According to previous studies, the incidence of cancer development in the residual tissue is 1-9%14. The efficacy of contralateral prophylactic mastectomy in patients with breast cancer is estimated to be 96%15. In a study by Hartmann et al.15, prophylactic mastectomy reduced the risk of breast cancer by almost 90%.
Secondary or saving reconstruction, defined as the complete revision of a prior reconstruction, is performed in cases of unsatisfactory outcomes or failure of the first surgery16. Secondary procedures were performed in 26 patients. It is worth noting that myocutaneous flaps, TRAM and LDMF, were used in 96.15% of the secondary procedures, which demonstrates the capacity of these flaps to provide healthy and well-vascularized tissue in an area that was previously manipulated.
The complication rate observed in this study (33.41%) is in agreement with those in the literature and varied (15-45%) according to the type of surgery performed. As observed in this study, this percentage increases with the number of risk factors (obesity, smoking, comorbidities, and radiotherapy)11. It is important to note that not all of the encountered complications compromised the final surgical outcome or led to further interventions. For example, seroma, which accounted for almost 25% of the detected complications, could be treated in outpatient clinics and rarely led to permanent complications. However, smoking is associated with a significant increase in the rate of flap necrosis as well as other complications17. In the latter 135 analyzed reconstruction procedures, the complication rate in smokers was 67%, well above the overall complication rate of 33.41%.
CONCLUSIONS
Breast reconstruction is becoming increasingly popular and important to many women undergoing breast cancer treatment. Procedure selection depends on surgeons' experience and their relationship with the mastology team as well as the views of the patients and their families.
Breast reconstruction is safe, with limited complications. The presence of risk factors such as obesity, smoking, comorbidities, and radiotherapy increase the complication rate. Therefore, the surgeon should collect all necessary information, including whether the patient was properly prepared for surgery, had adequate indications for it, and was rigorously monitored after the procedure.
Moreover, the higher incidence of bilateral surgeries performed in the latter study years was attributed to the increased interest in prophylactic mastectomy of the contralateral breast to reduce the risk of cancer and facilitate mammary symmetrization.
REFERENCES
1. Instituto Nacional de Câncer. Estimativa 2012: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2011. 118p.
2. Cheville AL, Tchou J. Barriers to rehabilitation following surgery for primary breast cancer. J Surg Oncol. 2007;95(5):409-18.
3. Parker PA, Youssef A, Walker S, Basen-Engquist K, Cohen L, Gritz ER, et al. Short-term and long-term psychosocial adjustment and quality of life in women undergoing different surgical procedures for breast cancer. Ann Surg Oncol. 2007;14(11):3078-89.
4. Rietman JS, Dijkstra PU, Debreczeni R, Geertzen JH, Robinson DP, De Vries J. Impairments, disabilities and health related quality of life after treatment for breast cancer: a follow-up study 2.7 years after surgery. Disabil Rehabil. 2004;26(2):78-84.
5. Sheppard LA, Ely S. Breast cancer and sexuality. Breast J. 2008;14(2):176-81.
6. Keith DJ, Walker MB, Walker LG, Heys SD, Sarkar TK, Hutcheon AW, et al. Women who wish breast reconstruction: characteristics, fears, and hopes. Plast Reconstr Surg. 2003;111(3):1051-9.
7. Malata CM, McIntosh SA, Purushotham AD. Immediate breast reconstruction after mastectomy for cancer. Br J Surg. 2000;87(11):1455-72.
8. Hu E, Alderman AK. Breast reconstruction. Surg Clin North Am. 2007;87(2):453-67.
9. Tuttle TM, Jarosek S, Habermann EB, Arrington A, Abraham A, Morris TJ, et al. Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol. 2009;27(9):1362-7.
10. Stucky CC, Gray RJ, Wasif N, Dueck AC, Pockaj BA. Increase in contralateral prophylactic mastectomy: echoes of a bygone era? Surgical trends for unilateral breast cancer. Ann Surg Oncol. 2010;17(Suppl 3):330-7.
11. Cosac OM, Costa LA, Barros APGSH. Reconstrução mamária bilateral com retalhos pediculados. In: Melega JM, Viterbo F, Mendes FH, eds. Cirurgia plástica: os princípios e a atualidade. Rio de Janeiro: Guanabara Koogan; 2011. p. 732-42.
12. Rozen WM, Ashton MW, Taylor GI. Defining the role for autologous breast reconstruction after mastectomy: social and oncologic implications. Clin Breast Cancer. 2008;8(2):134-42.
13. Broet P, de la Rochefordiere A, Scholl SM, Fourquet A, Mosseri V, Durand JC, et al. Contralateral breast cancer: annual incidence and risk parameters. J Clin Oncol. 1995;13(7):1578-83.
14. van Geel AN. Prophylatic mastectomy: the Rotterdam experience. Breast. 2003;12(6):357-61.
15. Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Myers JL, Arnold PG, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340(2):77-84.
16. Hamdi M, Casaer B, Andrades P, Thiessen F, Dancey A, D'Arpa S, et al. Salvage (tertiary) breast reconstruction after implant failure. J Plast Reconstr Aesthet Surg. 2011;64(3):353-9.
17. Knobloch K, Gohritz A, Reuss E, Vogt PM. Nicotine in plastic surgery: a review. Chirurg. 2008;79(10):956-62.
1. Plastic Surgeon, full member of Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Regent of the Plastic Surgery Service of the Armed Forces Hospital, Brasilia, DF, Brazil
2. Plastic Surgery Resident at the Daher Lago Sul Hospital, Brasilia, DF, Brazil
3. Plastic Surgeon, Associate Member of SBCP, Brasilia, DF, Brazil
Correspondence to:
Ognev Meireles Cosac
Condominio Villages Alvorada - cjto. 17 - casa 10 - Lago Sul
Brasilia, DF Brazil - ZIP 71680-351
E-mail: ognev@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 3, 2012
Article accepted: January 20, 2013
This study was performed at CIRPLAS Clinic, Brasilia, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter