

Original Article - Year 2013 - Volume 28 -
Nautilus-shaped dynamic craniotomy: a new surgical technique and preliminary results
Nautilus: craniotomia dinâmica - nova técnica cirúrgica e resultados preliminares
ABSTRACT
INTRODUCTION: Considering that craniosynostosis is a suture-related condition, the main challenge for its treatment is the fact that the brain is located in a closed compartment that does not have the required adaptability to accommodate its growth. The goal of treatment is to restore stenotic suture adaptability and correct the compensatory cranial deformity. This paper proposes the combined use of spiral osteotomy with distraction osteogenesis by the use of distracting springs to remodel craniofacial defects caused by craniosynostosis.
METHODS: Between July 2010 and July 2012, 10 patients with craniosynostosis were treated: 5 with oxycephaly, 3 with scaphocephaly, 1 with turricephaly, and 1 with trigonocephaly. The treatment consisted of the application of Lauritzen springs to correct the primary craniosynostosis defect in combination with a nautilus-shaped spiral craniotomy at the secondary deformation sites without dural detachment.
RESULTS: Resolution of cranial deformity and remission of the clinical signs of intracranial hypertension were observed. None of the patients had complications such as cerebrospinal fluid fistula, local infection, seroma, or hematoma.
CONCLUSIONS: The combined use of spiral osteotomy with spring-mediated distraction or contraction enables active reshaping of the skull and facilitates accommodation of the brain by the cranial cavity. (clinicaltrials.gov identifier: NCT01672619)
Keywords: Craniosynostoses. Osteogenesis, distraction. Craniotomy.
RESUMO
INTRODUÇÃO: Considerando-se que as craniossinostoses são afecções basicamente suturais, o fato de o cérebro estar aprisionado em um compartimento fechado, que não possui a complacência necessária para acompanhar seu crescimento, se constitui no desafio principal de seu tratamento. O objetivo do tratamento é restabelecer a complacência da sutura estenótica e corrigir a deformidade craniana compensatória. Este trabalho propõe a associação de osteotomía helicoide à distração osteogênica proporcionada pelo uso das molas distratoras para remodelar defeitos craniofaciais causados por craniossinostoses.
MÉTODO: Entre julho de 2010 e julho de 2012, foram tratados 10 pacientes portadores de craniossinostoses, sendo 5 oxicefalias, 3 escafocefalias, 1 turricefalia e 1 trigonocefalia. O tratamento consistiu na aplicação de molas de Lauritzen, para corrigir a deformidade primária da craniossinostose, com a associação de craniotomia helicoide em forma de Nautilus nos sítios de deformação secundária do crânio, sem descolamento dural.
RESULTADOS: Foi observada resolução da deformidade craniana e remissão dos sinais clínicos de hipertensão intracraniana. Nenhum paciente apresentou complicações, como fístula liquórica, infecção local, seroma ou hematoma.
CONCLUSÕES: A associação da osteotomia helicoide com a distração ou contração promovida pelas molas permitiu remodelar ativamente o crânio, facilitando a acomodação do conteúdo cerebral no continente craniano. Clinical trials.gov Identifier: NCT01672619.
Palavras-chave: Craniossinostoses. Osteogênese por distração. Craniotomia.
Craniosynostoses, known and described since the times of ancient Greece, were so clearly studied and classified by Virchow that his concepts remain as the basis of all understanding of this disease to this day1,2.
Since the first attempts to treat skulls deformed by craniosynostoses, restoration of the stenotic line expandability (primary defect) and remodeling the areas of compensatory deformation (secondary defect) have been the main concerns. In the evolutionary history of the treatment of craniosynostoses, we reviewed extensive and morbid craniectomies and suturectomies that possibly involved the interposition of materials or caustic substances in an attempt to inhibit the recurrence of early suture closure3,4 through distraction osteogenesis using external distractors5 and skullcap remodeling1. Such remodeling, the preferred practice still today, follows various types of osteotomies, but all involve craniotomy using dural detachment, back table remodeling of the osteotomized cap, and its return as a graft fixed with varied materials.
However, these procedures have high morbidity, with the possibility of several complications related to dead space between the dura mater and cap grafts6. Furthermore, static remodeling causes cavity expansion that does not always adequately meet the actual requirement. Therefore, Lauritzen et al.7 proposed dynamic cranial remodeling using expander springs in 1998. They applied the principles of osteotomy and interposition of metal springs, without detaching the dura, by inserting expansive forces on the stenotic lines that are distributed throughout the dura around the whole brain content/cavity to reshape the skull7.
Because of the ideal characteristics of the spiral shape for modeling convex surfaces, Salyer and Bardach8 proposed its use in modeling osteotomies in scaphocephaly. They advocated extensive posterior biparietal craniotomy in which they performed a back-table spiral osteotomy of the cap; after being remodeled, the cap is attached to the skull as a graft. Tullous et al.9 and Solis-Salgado and Anaya-Jara10 advocated the use of spiral osteotomies for scaphocephaly treatment but performed them bilaterally to the sagittal line. Back-table remodeling was performed for the 2 large craniotomy plates through spiral osteotomies. The expanded form was secured with absorbable plates, and the pieces were returned to the skull as a graft.
As demonstrated by the authors cited above, the curved shape of the spiral adapts perfectly to the remodeling of a surface curve like the skullcap. However, in the absence of fixation, the spiral shape of the osteotomy can turn bone into a spring that is able to expand or contract according to the direction of the force it receives (Figure 1). This form of osteotomy was therefore chosen by the authors to induce compliance in the areas of bone with secondary defects, which must indirectly compress or expand during the process of dynamic remodeling of the primary defect using springs.
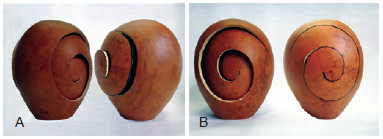
Figure 1 - Representation of the shape of the osteotomy and its possibilities for expansion (A) or contraction (B) using the fruit of Lagenaria siceraria ("gourd") as a model of rigid structure.
The objective of this study is to demonstrate the usefulness of nautilus-shaped spiral osteotomy for inducing indirect remodeling of skulls deformed by craniosynostoses associated with dynamic remodeling using implantable springs.
METHODS
Patients treated at the Plastic Surgery Department of the Advanced Plastic Surgery Center from July 2010 to July 2012 with a diagnosis of craniosynostosis were eligible to participate in this prospective study.
The inclusion criteria for the study were presence of residual cranial deformity after previous treatment, complex (involving more than one suture) or syndromic craniosynostosis, and trigonocephaly. Furthermore, patients with cranial deformities that required complex surgery involving cranial remodeling were included. The study excluded patients with simple craniosynostosis or for which treatment could be achieved through suturectomies, expansion with springs, or video-assisted minimally invasive surgery.
Ten cases of craniosynostosis were treated, including 5 of oxycephaly, 3 of scaphocephaly, 1 of turricephaly, and 1 of trigonocephaly. The patients were aged 5-160 months (Table 1). Each patient underwent preoperative clinical, laboratory, and imaging testing. All procedures were performed with the permission and consent of the patients' parents or guardians. The study protocol was approved by the Ethics and Research Council of the Hospital da Real e Benmérita Associação Portuguesa of Sao Paulo (Protocol number 777-12 dated March 30, 2012), the hospital where the surgeries were performed.

All patients underwent surgery under general anesthesia, received intraoperative blood transfusion to replace blood loss (decreases in hemoglobin of 3-5 points), mean blood pressure control, and immediate postoperative follow-up in the intensive care unit (ICU). The surgeries were performed by collaborating pediatric neurosurgery and craniofacial surgery teams.
As described by Lauritzen et al.7, the procedure involved 2 surgical steps: first, spring placement for nautilus-shaped dynamic osteotomy; and second, spring removal performed 6-12 months after the initial procedure. The timing of spring removal was determined according to the degree of ossification of the osteotomy and evaluated by 3-dimensional tomography of the skull. If consolidated osteotomies were observed, the springs were removed; presence of open osteotomies signaled ongoing remodeling and resulted in delay of spring removal. Spring removal was not delayed only in the presence of complications such as infection or exposure of the spring through the skin or scalp.
The cranial shape was evaluated postoperatively by 4 independent surgeons who used the following scale to grade the results: insufficient, no attenuation of the pre-operative deformity existed; partial, correction did occur but did not include all features of the deformity; and appropriate, total remission of the cranial deformity was obtained.
Surgical Technique
A broken-line coronal incision was made in the temporal regions with subperiosteal detachment of the scalp flaps.
The springs were used in osteotomies performed to correct the primary defect (caused by sutural stenosis), whereas nautilus-shaped spiral osteotomies were used in the areas with secondary defects (caused by indirect remodeling).
In areas containing a compensatory hump, a nautilus-shaped osteotomy was performed to enable collapsing, and the osteotomy traces were widened with a wear drill to decrease surface area. Gains in intracranial space were induced by the expansion springs applied according to craniosynostosis type.
In areas of compensatory fossa (flattening), a nautilus-shaped osteotomy was performed for expansion, and a centrifugal bevel was used to induce progressive increase in surface area. The combined action of the contracting springs to reduce excessively elongated regions was responsible for the ejection of the contents toward the area of fragility created by the expander.
If the area to be expanded included the insertion of the greater wing of the sphenoid bone, this was released. A craniotomy hole was created using a wearing drill after the zygomaticofrontal suture. This enabled osteotomy of the wing of the sphenoid bone using a curved chisel without requiring craniotomy cap detachment and with minimal dural detachment.
All osteotomies were performed with minimal dural detachment without the removal of any skullcap segment for back-table modeling.
RESULTS
In the first 12 postoperative hours, all patients had moderate pain that was controlled by non-opioid analgesics. Edema of the operated region, including major eyelid expansion and chemosis, peaked on the second day postoperatively, and full resolution was seen in 8-15 days.
Length of ICU stay was 1-3 days, and the overall hospitalization time was 3-6 days. In the second stage of the procedure, the patients were hospitalized for 1 day only, and the use of an ICU bed or blood transfusion was unnecessary.
All patients had an uneventful postoperative period, and those who showed neuropsychomotor impairment related to intracranial hypertension had signs suggestive of clinical improvement (parental reports of improvement in concentration, gain of motor skills, and remission of headache). No patients experienced a CSF fistula, seroma, hematoma, signs of infection, spring externalization, or other complications.
The desired cranial remodeling was obtained in all cases (Figures 2-8). The 4 surgeons who evaluated the postoperative cranial shape considered the results partial in 40% of cases and appropriate in 60%.
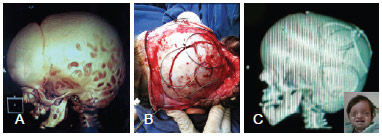
Figure 2 - Patient with turricephaly. In A, lateral preoperative computed tomography of the skull. In B, intraoperative detail. In C, computed tomography of the skull performed in the seventh postoperative month revealed remission of the "beaten silver sign."

Figure 3 - Patient with oxycephaly. In A, C, and E, preoperative appearance on frontal, lateral, and left oblique views. In B, D, and F, appearance in the fifth postoperative month: frontal view in frontal, lateral, and left oblique views.

Figure 4 - Oxycephaly. In A and C, preoperative computed tomography (CT) of the skull. In B and D, CT of the skull in the fifth postoperative month revealing remission of the fingerprint-like patterns observed on preoperative CT.

Figure 5 - Patient with turricephaly. In A, D, G, preoperative appearance from the frontal, right lateral, and right oblique views. In B, E, H, appearance in the eighth postoperative month from the frontal, lateral right, and right oblique views. In C, F, and I, appearance in the first month after removal of springs in the frontal, right lateral, and right oblique views.

Figure 6 - Turricephaly. In A and C, preoperative computed tomography (CT) of the skull. In B and D, CT of the skull in the eighth postoperative month revealing remission of fingerlike prints observed on preoperative CT.

Figure 7 - Scaphocephaly. In A, preoperative 3-dimensional skull computed tomography (CT), lateral view. In B, postoperative 3-dimensional skull CT.

Figure 8 - Scaphocephaly. In A and B, preoperative computed tomography of the skull of the same patient as in Figure 7. Axial section at the level of the lateral ventricles showing enlargement of the lateral-lateral diameter and anterior posterior shortening.
DISCUSSION
Realizing the compensatory effect of skull growth in the presence of stenosis, Virchow postulated that the direction of growth of the cranial vault is always parallel to the axis of the compromised suture by compensatory expansion of sutures perpendicular to the stenosis1.2. Therefore, deformation of the skull occurs because of not only growth cessation in the area of stenosis but also compensatory growth of the unaffected sutures, which do not always fulfill the function of providing sufficient intracranial space for undamaged brain growth. This indirect compensatory remodeling determines the final shape of skulls with stenosis.
These concepts by Virchow led us to conclude that the skulls affected by craniosynostosis have 2 types of defects: primary, the synostosis itself; and secondary, the deformation or compensatory remodeling of the skull. Therefore, there are 2 methods for classifying craniosynostoses: one that refers to the affected suture and pointing toward the primary defect, such as sagittal craniosynostosis and coronal cra-niosynostosis; and the other referring to the final skull shape, i.e., pointing toward the secondary defect (scaphocephaly or turricephaly).
Because craniosynostosis is a suture-related condition, the main challenge in its treatment is the fact that the brain is located inside a closed compartment that does not have the required adaptability to accompany brain growth. All techniques proposed and performed since the dawn of medical science to this day have aimed to provide space for the expansion of the brain in order to prevent or minimize compression damage11.
The consensus is that treatment should be performed as early as possible because the longer it occurs after the first year of life, the greater are the neurological sequelae observed12-14. It is believed that after 2 years of age, the brain no longer needs sutural expansion to finish its growth because it can be achieved by simple cap remodeling alone. However, this hypothesis is not supported by clinical findings: a group of children with craniosynostosis who were treated for decompression within the first year of life and showed good development began to show symptoms of intracranial hypertension, such as headache, hyperactivity, and cognition disorders, by 4 or 5 years of age. If such results can be found in patients in whom surgery is completed early, then much more obvious and dramatic adverse events will occur in children who have lost the opportunity to receive decompression treatment in early childhood. Therefore, it is necessary to have the means to treat older children with an unexpanding and ossified skull cap that does not respond to indirect or secondary remodeling in cranial areas not affected by surgical remodeling.
This necessity leads to another very common problem in craniofacial surgery, i.e., the progressive stabilization of dural elasticity with age. The longer surgery is delayed after the first 2 years of life, the more difficult it is for brain tissue and the dural sheath to occupy the space offered, leading to the maintenance of dead space, seroma, infection, osteomyelitis, and loss of the cap's remodeled area15.
The treatment of older skulls (after 2 years of age) through distraction osteogenesis with expansion springs allows for dynamic and progressive remodeling since it maintains adherence of the dura to the moving cap and the cap need not be removed to be reused as a graft. The bone remains vascularized and inserted, drastically decreasing trans- and postoperative morbidity. Moreover, expansion is not controlled by external forces but rather by spring elasticity, and the need for brain expansion causes cessation of the expansion to be modulated by the cap ossification and the homeostasis between pressure and intracranial space. Offering the tissues the opportunity to occupy the required space is a safer and more precise technique than just creating a pre-designed and static gain in space as in conventional remodeling16.
A nautilus-shaped spiral osteotomy in the areas of secondary defect, where an indirect response to compression or spring-induced distraction is sought, produces great plasticity in the bone of the cap and keeps it adhered to the dura mater because there is no detachment or removal of the cap from its position. The bone spring created by spiral osteotomy allows the cap to respond to expansion within skulls that were being contracted by springs and with flattening (retraction) in skulls that were being dynamically expanded with springs (Figure 1). Maintaining continuity between the cap and the dura guarantees the absence of dead space. This extends the indication of cranial remodeling for any age, even in adults, where dural inextensibility does not usually allow for detachment and increases to the cavity without the burden of collections of dead space.
The minimally invasive feature of the procedure described here provides greater safety and lower morbidity, opening a wide range of treatment options for craniosynostosis. The only drawback is the need for 2 surgical procedures (one for spring placement and another for spring removal), even considering that the former is much less invasive than conventional surgery and that the latter is of very short duration and can be performed in an outpatient setting.
The remission of indirect signs of cranial hypertension, such as the disappearance of fingerlike impressions of the skull that are present on CT intraoperatively and the improvement in symptoms (headache), suggests that osteotomy effectively reduced intracranial pressure. However, as this variable was not evaluated preoperatively (for example, determination of papilledema), the extension of this study could be a future perspective.
The limitations of the short postoperative follow-up and the small number of patients in the present study are offset by the novelty of the nautilus-shaped dynamic osteotomy. The spiral shape of these osteotomies adds elasticity to the bone and transforms the cap itself into a spring to enable global reshaping of the skull with low morbidity, thus enabling the use of dynamic expansion at any age.
Spring forces act and spread throughout the dura mater to interfere with the content/cavity ratio of the brain. Therefore, spiral osteotomies provide indirect skull remodeling by inducing retraction of the secondary humps associated with the use of expanding springs and inducing expansion of the zones of flattening associated with the use of contracting springs (Figures 7 and 8).
CONCLUSIONS
We successfully induced indirect remodeling of synostotic skulls that were subjected to dynamic remodeling with implantable springs using nautilus-shaped spiral osteotomies.
REFERENCES
1. Persing JA, Jane JA, Shaffrey M. Virchow and the pathogenesis of craniosynostosis: a translation of his original work. Plast Reconstr Surg. 1989;83(4):738-42.
2. Mark ES, Persing JA, Christopher I, Shaffrey JAJ. Craniosynostosis. In: Rengachary SS, Wilkins RH, eds. Principles of neurosurgery. 2nd ed. London: Wolfe; 2004. p.8.2-8.15.
3. Guimarães-Ferreira J, Miguéns J, Lauritzen C. Advances in craniosynostosis research and management. Adv Tech Stand Neurosurg. 2004;29:23-83.
4. Greensmith AL, Holmes AD, Lo P, Maxiner W, Heggie AA, Meara JG. Complete correction of severe scaphocephaly: the Melbourne method of total vault remodeling. Plast Reconstr Surg. 2008;121(4):1300-10.
5. Cardim VLN, Dornelles RFV. Craniossinostoses. In: Carreirão S, Carneiro Jr. LVF, eds. Cirurgia plástica para a formação do especialista. São Paulo: Atheneu; 2011. p.297-308.
6. Ortiz-Monasterio F, del Campo AF, Carrillo A. Advancement of the orbits and the midface in one piece, combined with frontal repositioning, for the correction of Crouzon's deformities. Plast Reconstr Surg. 1978;61(4):507-16.
7. Lauritzen C, Sugawara Y, Kocabalkan O, Olsson R. Spring mediated dynamic craniofacial reshaping. Case report. Scand J Plast Reconstr Surg Hand Surg. 1998;32(3):331-8.
8. Salyer KE, Bardach J. Salyer & Bardach's atlas of craniofacial & cleft surgery. Philadelphia: Lippincott-Raven; 1999.
9. Tullous MW, Henry MN, Wang PTH, Vollmer DG, Auber AE, Mancuso PA. Multiple-revolution spiral osteotomy for cranial reconstruction. Technical note. J Neurosurg. 2001;94(4):671-6.
10. Solís-Salgado O, Anaya-Jara M. Remodelación craneal para craneosi-nostosis sagital mediante osteotomía en forma de espiral usando sistema de fijación con miniplacas y tornillos absorbibles. Arch Neurocien. 2009;14(4):224-30.
11. Panchal J, Uttchin V. Management of craniosynostosis. Plast Reconstr Surg. 2003;111(6):2032-48.
12. Renier D. Intracranial pressure in craniosynostosis pre and postoperative recordings: correlation with functional results. In: Persing JA, Edger-ton MT, Jane JA, eds. Scientific foundation and surgical treatment of craniosynostosis. Baltimore: Williams & Wilkins; 1989. p.263-9.
13. Arnaud E, Meneses P, Lajeunie E, Thorne JA, Marchac D, Renier D. Postoperative mental and morphological outcome for nonsyndromic brachycephaly. Plast Reconstr Surg. 2002;110(1):6-12.
14. Cohen MMJ. Craniosynostosis: diagnosis, evaluation and management. New York: Raven Press; 1986.
15. David DJ, Sheen R. Surgical correction of Crouzon syndrome. Plast Reconstr Surg. 1990;85(3):344-54.
16. Cardim VLN, Silva AS, Salomons RL, Dornelles RFV, Lima e Silva A, Blom JOS. Remodelagem de crânios maduros utilizando molas expansoras.Rev Bras Cir Craniomaxilofac. 2012;15(2):57-63.
1. Full Member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), PhD in General Surgery by the Faculty of Medical Sciences of Santa Casa de São Paulo, Coordinator of the Advanced Plastic Surgery Center (NPA), São Paulo, SP, Brazil
2. Full Member of the SBCP, Assistant Plastic Surgeon at the NPA, São Paulo, SP, Brazil
3. Full Member of the SBCP, MSc in Plastic Surgery by the University of São Paulo, Assistant Plastic Surgeon at the NPA, São Paulo, SP, Brazil
4. Associate Member of the SBCP, Assistant Plastic Surgeon at the NPA, São Paulo, SP, Brazil
5. Full Member of the Brazilian Society of Neurosurgery, MSc and PhD in Neurosurgery by the Federal University of São Paulo, Pediatric Neurosurgeon, Coordinator of the Center for Pediatric Neurosurgery (CENEPE), São Paulo, SP, Brazil
Correspondence to
Vera Lucia Nocchi Cardim
Rua Augusta, 2709 - cj. 41 - Jardim América
São Paulo, SP Brazil - CEP 01413-000
E-mail: vera@npa.med.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 1, 2012
Article accepted: January 20, 2013
This study was performed at the Beneficência Portuguesa Hospital of São Paulo, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter