

Original Article - Year 2013 - Volume 28 -
Evaluation of plastic surgery residency programs in Distrito Federal
Avaliação dos programas de residência médica em Cirurgia Plástica no Distrito Federal
ABSTRACT
INTRODUCTION: The residency period is an important step in the medical training of plastic surgeons in Brazil. However, there are few qualitative studies about the existing residency programs. Thus, the aim of this study was to conduct a qualitative research of the medical residency programs of the accredited services of the Brazilian Society of Plastic Surgery in Distrito Federal.
METHODS: This cross-sectional study was performed through individual structured questionnaires, which were self-administered by residents training in the accredited services of Distrito Federal, in 2012.
RESULTS: Eighteen residents (age range, 25-52 years; 13 [72.2%] men and 5 [27.8%] women) agreed to participate. Of them, 61.1% reported that the hospital had complementary services necessary to meet patients' continuous care and the minimum requirements of the program, 66.7% thought that the bibliographic archive was only partially adequate or inadequate, and 72.2% reported to participate in 2 or more hours of weekly scientific meetings. Participation in 5 to 10 surgeries per week was reported by 88.8% of participants. Most residents said that they participate for up to 4 hours/week as a surgeon and 11-20 hours/week as an assistant. Most (66.7%) of residents had made presentations at scientific meetings, and 72.2% had no articles published in the Brazilian Journal of Plastic Surgery. With respect to the workload of the residency program, 80% were assigned to outpatient, infirmary, and surgical center activities, and 20% were assigned to theoretical activities. Among the suggestions mentioned to improve the medical residency programs were the need to increase the scope and the interchange between services, as well as the encouragement of scientific research output.
CONCLUSIONS: The perception of plastic surgery residents in the accredited services of Distrito Federal, about the curriculum, program structure and teaching performance, was positive. The negative aspects mentioned were the range and distribution of the curriculum, lack of emergency care, inadequate training in reconstructive procedures, and compact training in other areas, as well as an unsatisfactory bibliographic archive and lack of incentive for researchers. Among the suggestions especially mentioned for the improvement of the medical residency programs were the need to increase the scope and the exchange between services, as well as the encouragement of scientific research output.
Keywords: Plastic surgery. Teaching. Education. Education, medical. Internship and residency.
RESUMO
INTRODUÇÃO: A residência médica é um passo importante no treinamento dos médicos residentes de Cirurgia Plástica no Brasil; entretanto, são poucos os estudos que avaliam os programas de residência sob o ponto de vista qualitativo. Assim, este artigo objetiva realizar pesquisa qualitativa dos programas de residência médica dos serviços credenciados da Sociedade Brasileira de Cirurgia Plástica no Distrito Federal.
MÉTODO: Foi realizado estudo transversal, com a aplicação de questionário individual estruturado, autoaplicado aos residentes em treinamento nos serviços credenciados do Distrito Federal, no ano de 2012.
RESULTADOS: Dezoito médicos residentes, com idade entre 25 anos e 52 anos, 13 (72,2%) homens e 5 (27,8%) mulheres, concordaram em participar da pesquisa. Desses, 61,1% relataram que o hospital dispunha de serviços complementares necessários ao atendimento ininterrupto dos pacientes e aos requisitos mínimos do programa, 66,7% consideraram que o acervo bibliográfico era parcialmente adequado ou inadequado, e 72,2% referiram ter 2 ou mais horas de reuniões científicas semanais. A participação em 5 a 10 cirurgias por semana foi reportada por 88,8% dos participantes; a maioria dos residentes afirmou participar de até 4 horas/semana como cirurgião e de 11 a 20 horas/semana como auxiliar. A maioria (66,7%) dos residentes já havia realizado apresentações em eventos científicos e 72,2% não tinham artigos publicados na Revista Brasileira de Cirurgia Plástica. Com relação à carga horária do programa de residência, 80% eram destinados a atividades em ambulatório, enfermaria e centro cirúrgico e 20%, a atividades teóricas. Dentre as sugestões de melhoria dos programas de residência médica, foram apontados, principalmente, a necessidade de aumentar a abrangência e o intercâmbio entre os serviços e o incentivo à produção científica.
CONCLUSÕES: A percepção dos residentes em cirurgia plástica dos serviços credenciados do Distrito Federal foi positiva no que se refere a grade curricular do programa, estrutura para atendimento e desempenho da preceptoria. Quanto aos pontos negativos, foram apontados abrangência e distribuição da grade curricular, falta de atendimento de emergência, menor treinamento em procedimentos de natureza reparadora e reduzido em estágios de outras áreas, além de acervo bibliográfico insatisfatório e pouco incentivo à pesquisa. Dentre as sugestões de melhoria dos programas de residência médica, foram apontados, principalmente, a necessidade de aumentar a abrangência e o intercâmbio entre os serviços e o incentivo à produção científica.
Palavras-chave: Cirurgia plástica. Ensino. Educação. Educação médica. Internato e residência.
The plastic surgery residency is based on 3 main components: surgical, scientific, and among professionals training. There is concern among coordinators and tutors that the training in the surgical practice may not be adequate for professional qualification1,2.
The impact of the acquisition and understanding of plastic surgery training has been poorly assessed among the medical residency programs in Brazil, especially from the perspective of residents.
In the national literature, there are few studies that focused on the teaching of plastic surgery. Lima et al.3 emphasized the need for teaching augmentation gluteoplasty in the current batch of residents in order to increase demand, and Monteiro et al.4 conducted a study among undergraduate students who participated in the training program of the Bahian League of Plastic Surgery, under the supervision of the Plastic Surgery Service at the Hospital das Clínicas of the University of Bahia. Pochat et al.5 highlighted the importance of cadaveric dissection activities in anatomy studies during medical residency training, and Ruiz et al.6 proposed a methodology for training in the nonsurgical treatment of the nasolabial fold area and perioral region. Finally, Dias et al.7 described a practical training course of microsurgery in plastic surgery.
In Brazil, residency programs are regulated by Law Nº 11.381, enacted on December 1, 20068; Resolution Nº 2 of the National Medical Residency Committee (CNRM), enacted on May 17, 20069; and the Regulations of the Department of Accredited Services of the Brazilian Society of Plastic Surgery (BSPS)10. The BSPS has 86 accredited residency programs, which require 6 years of medical training, 2 years of residency in general surgery, and 3 years in plastic surgery. The Federal District has 3 affiliated services through which an average of 20 residents train per year, distributed in R3, R2, and R1. The Internal Regulations of the Department of Education of the Accredited Services (DESC) of the BSPS of 1997 consists of 23 articles, which cover various areas of expertise required for acquiring the medical specialty.
The aim of this study was to perform a qualitative assessment of the medical, BSPS accredited, residency programs from Distrito Federal, Brazil.
METHODS
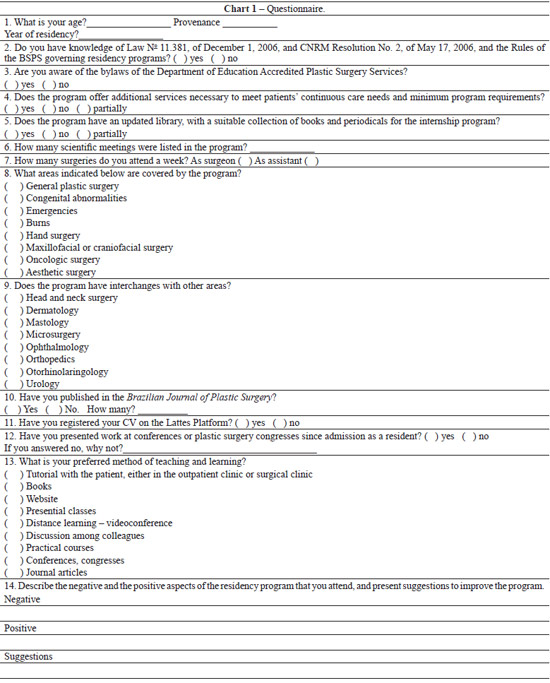
This is a descriptive, qualitative, cross-sectional study, using individual structured questionnaires that were self-administered to training residents in the accredited services of Distrito Federal, in the year 2012 (Table 1).
Data were analyzed using the Statistical Package for Social Sciences (SPSS) program, version 15.0, and compared with the mandatory requirements for the programs established by the CNRM and BSPS.
Data from the open questions were analyzed using a content analysis technique, by defining categories and identifying their frequency, and excerpts were selected from accounts that exemplified them.
The study was approved by the ethics committee of the Sarah Hospital Network.
RESULTS
In Distrito Federal, there are 3 residency programs accredited by the BSPS.
The plastic surgery residency programs are present in public, private, and mixed hospitals, and have a duration of 3 years, with 2880 hours distributed in 8-hour daily shifts.
In 2012, there were 19 registered residents, on average, 2 residents per year of training. Eighteen residents (age range, 25-52 years; 13 [72.2%] men and 5 [27.8%] women), mostly from other states, agreed to participate of the study (Table 1).
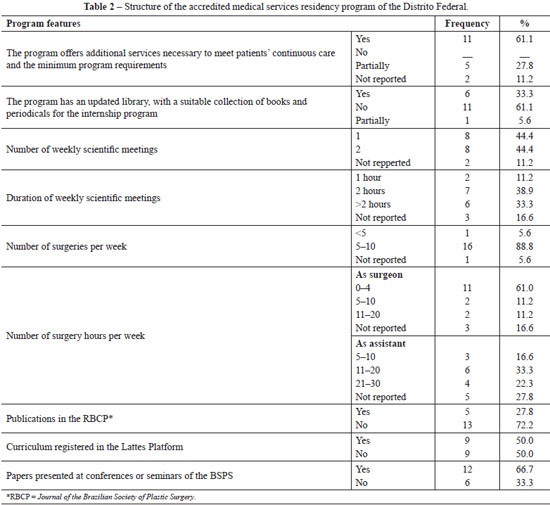
From questions related to the knowledge about the regulation of plastic surgery residencies in Brazil, it was found that 70% of participants were unaware of the directive. Concerning the prerequisites of the programs, 61.1% reported that the hospital had additional services required for continuous care of patients and the minimum requirements of the program; 66.7% thought that the bibliographic archive, including books and periodicals, was only partially adequate or inadequate; and 72.2% reported to participate in 2 hours or more of weekly scientific meetings (Table 2).
Participation in 5 to 10 surgeries per week was reported by 88.8% of participants. Most residents stated that they participate for up to 4 hours/week as a surgeon and 11-20 hours/week as an assistant (Table 2). With respect to the workload of the residency program, 80% were assigned to outpatient, ward, and surgical center activities, whereas 20% were assigned to theoretical activities.
The majority (66.7%) of the residents had made presentations at scientific meetings, and 72.2% had no articles published in the Brazilian Journal of Plastic Surgery (Table 2).
The most common surgical procedures were of a cosmetic nature (breast lift, abdominoplasty, and liposuction). The coverage of the residency program included topics on general plastic surgery, burns, surgical oncology, and aesthetics (Figure 1).
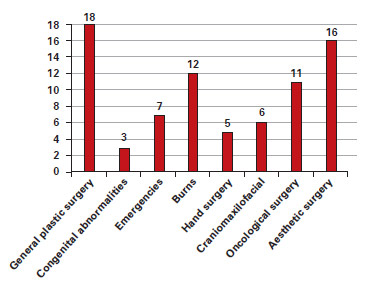
Figure 1 - Scope of the residency program.
With respect to interchange with other areas, dermatology and mastology were the most common services interchanged (Figure 2).
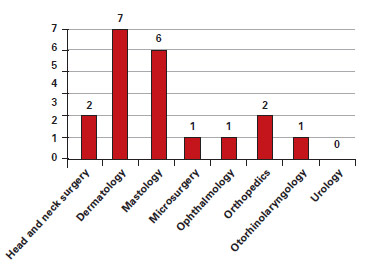
Figure 2 - Interchange with other areas.
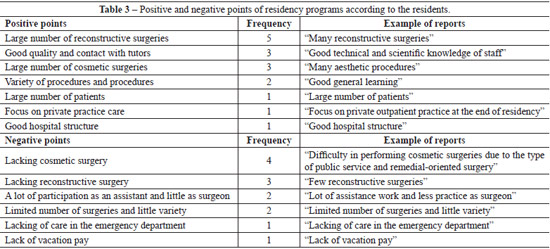
The positive and negative aspects of the residency programs mentioned by the participants are shown in Table 3.
The results about the preferred teaching and learning methods are summarized in Figure 3.
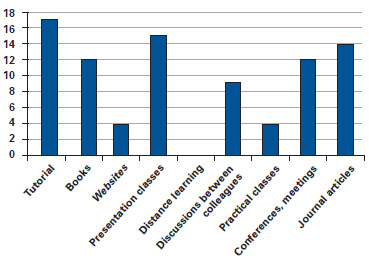
Figure 3 - Preference for the teaching and learning method.
The distribution of the activities required by the residency program according to the CNRM9 and the data obtained from the questionnaires are presented in Figure 4.
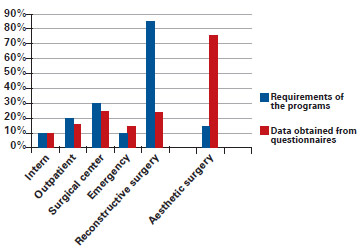
Figure 4 - Distribution of the activities required of the residency program according to the National Medical Residence Committee9 and data obtained from questionnaires.
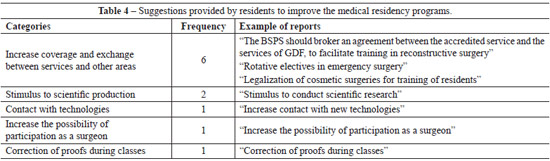
The need to increase the scope and the interchange between the services, and the encouragement of scientific research output were among the suggestions for the improvement of the medical residency programs, according to the residents' evaluation (Table 4).
DISCUSSION
The central focus of this study was to assess the perception of residents about the programs developed in services accredited by the BSPS, in Distrito Federal.
The questionnaire was developed on the basis of the Internal Regulations of the BSPS and CNRM. The limitations of this study include the impossibility of obtaining quantitative data relating to the process of the residency training programs, thus limiting the application of statistical tests. This is, therefore, an initial qualitative overview that can guide future research in assessing specific aspects.
Most of the respondents were unaware or had insufficient knowledge of the laws governing the medical residency programs8, of the CNRM Resolutions,9 and of the Rules of the BSPS10. The resolution of the CNRM foresees the following distribution of the annual minimum workload: 10% in the intern unit, 20% in the outpatient unit, 30% in the operating room, 10% in the emergency unit, and 10% in the burn unit, besides the required internships in craniofacial surgery, hand surgery, burn unit, reconstructive surgery of the face and limbs, breast surgery, reconstructive microsurgery, cosmetic surgery, and surgical oncology. The resolution also suggests optional internships in dermatology, orthopedics and traumatology, otorhinolaryngology, ophthalmology, obstetrics, and others, at the discretion of the institution. Finally, the resolution proposes at least 85% of reconstructive surgeries and at most 15% of strictly cosmetic surgeries. This regulation is being fulfilled in the services of Distrito Federal. However, the most common surgical procedures in the services are of a cosmetic nature, such as breast lift, liposuction, and abdominoplasty, in accordance with the study by Noone et al.11 and an evaluation of American medical undergraduates12, which found that the number of reconstructive surgery training programs is lower than that of other specialties. This situation has been experienced by plastic surgeons that have already been trained. In a study performed by the American Society of Plastic Surgery, 1250 plastic surgeons alleged that the number of reconstructive plastic surgeries has decreased during the past 10 years, as a result of personal choice and increased competitiveness with other surgical areas. Pinder et al.13 observed a change in training residency programs at the expense of reducing the number of working hours in the operative field, due to the reduction in emergency care and reconstructive surgery activities during training.
The assessment of the effectiveness of the plastic surgeon's training in a practical point of view is still difficult. Rinard and Mahabir14 described the result of a study conducted at the Scott & White Healthcare and the Texas A&M Health Science Center, applying the Electronic Residency Application Service questionnaire to 5 specialties, including plastic surgery. Those authors emphasized the criteria for approval and entry into residency programs. Carol et al.15 emphasized the need to teach basic skills in plastic surgery at an early stage, in order to maximize the quality of patient care, clinical evaluation, and surgical practice training. These authors published an instrument dedicated to the assessment of plastic surgeons' practical skills, the Objective Structured Assessment of Technical Skills (OSATS), used to evaluate the surgeons' education, practice, and surgical skills15. The authors proposed to develop a more objective and reliable tool, and they found reliable and significant findings with their method, which consisted of performance assessment in the repair of simple lacerations.
The European Working Time Directive16 published a guide for doctors in training. The policies contained in the document were developed by the Department of Medical Education and Training Group, and the Medical Council, and aimed at assessing the quality of medical education and training of doctors. The National Resident Matching Program17 provides data on the residency programs in the United States and their evolution over the years. Jalali et al.18 published results of interviews of 20 plastic surgery trainees in the United Kingdom, after a practical course, in order to analyze the impact of trust, understanding, and skills in the training of doctors. The need for practical training services in plastic surgery was underscored. This study also showed the positive impact of the course, as 95% of the participants felt more confident in performing procedures as surgeons and assistants. It is noteworthy that in Brazil, the CNRM Resolution suggests that the residency programs should allocate at least 10% and at most 20% of their workload on theoretical and practical activities, in the form of update sessions, seminars, clinical-pathological correlations, or others, whereas the rest of the workload should be used for practical activities.
The conflict between high-quality training and service demand was seen when the residents reported a lack of aesthetic surgery in some services, reconstructive care and first aid in others, and the need to interchange with other areas. This difficulty of reconciling the program with demand is a recurring theme. Wong et al.2 reported that the lack of surgical practice among plastic surgeons in the United Kingdom was a known problem. These authors provided suggestions to improve the practice, including courses and demonstrations, which are considered important but insufficient, because practice is developed through participation in the decision-making and performance in the operative field. As an example of these courses, microsurgery practical training, lasting a week, was held at various universities. As described by Dias et al.7, the routine microsurgery course and the use of the microscope must start with training on performing sutures by using nonliving tissue, followed by live models for vascular anastomoses and transplantation. Nevertheless, the challenge for preceptors to reconcile training with the need of health services remains.
Another aspect that stands out is the bibliographic archive, publications, and research incentive. These factors play an important role in the residency, physician's education, and ethics and professional training. Rinardi and Mahabir14 stressed that the research experience can influence, although not guarantee, career success.
The positive aspects of the residency programs included good involvement of preceptors, the number of hours of theoretical activities, and surgical experience, although with a lower workload as an acting surgeon. The preceptors play a vital role in preparing the residents: they transmit experience and confidence, and seek to provide opportunities to develop the students' skills during training. The services also presented a suitable structure for the program, in contrast to the reported insufficient bibliographic archive.
Davis et al.19 published a study conducted at the meeting of the British Association of Plastic, Reconstructive and Aesthetic Surgeons, which was attended by 93 physicians in a course that addressed the following topics: knowledge in plastic surgery, plastic surgeon's work, technical skills to perform basic plastic surgery procedures, and interest in the specialty. The authors verified a positive impact of the course on students.
Experience in the specialty is derived from reading, lectures, surgical performance, and clinic exposure8. Some of the options to improve the training are practices in reconstructive surgery and emergency care, because the surgical demand in these areas is large and increasing. In the Emergency Plastic Surgery Clinic of the Sisli Etfal Training and Research Hospital20, 10,732 attendances were recorded in a 4-year period, which facilitated training in upper extremity, burns, head and neck, and soft tissue surgery, with the practical application of the principles of plastic surgery, reconstruction, and microsurgery. Multidisciplinary care is ideal in the emergency ward, although there was a lack of action of plastic surgery teams in daily emergency services. Most emergency cases are referred to the orthopedics, oral and maxillofacial surgery, ophthalmology, and otolaryngology teams.
In some training centers, microsurgery has been, for the past 3 years, the basis for the development of practice in plastic surgery. The most common procedures are digital replantation, reconstruction of thumb and jaw, and repair of peripheral nerve injuries. Tanna et al.21 reasoned that this reality reflects the changing role of the plastic surgeon in reconstructive procedures, and also affects the curriculum of medical residency specialty programs. The growing demand for aesthetic procedures and greater economic attractiveness of cosmetic surgeries are among the factors that reduce the training in reconstructive procedures.
Suggestions for improving residency programs provided by the doctors interviewed included exchanges with other services that complement the curriculum, and encouraging research19,21,22. Other strategies for practical training were described by Wong et al.2, including laboratory training, use of the Internet and telemedicine, intensive short courses, conferences, and observation in the surgical specialty. Obviously, these activities do not replace the experience of surgical practice, but they form the basis required for the development of technical skills that often exist in surgeon training. The risk of a surgical rotation to increase the interchange results in a surgeon not wanting to attend the best organization in favor of a greater number of hours, and thus, the training and safety associated with surgical procedures is not improved.
CONCLUSIONS
The perception of plastic surgery residents in accredited services in the Distrito Federal was positive about the curriculum of the program, attendance structures, and preceptors performance. The negative aspects mentioned were the scope and distribution of the curriculum, lack of emergency care, inadequate training in reconstructive procedures, and less training in other areas, as well as an unsatisfactory bibliographic archive and lack incentive to perform research. Among the suggestions for the improvement of the medical residency programs, the need to increase the scope and the interchange between the services and the encouragement of scientific research output were especially mentioned.
REFERENCES
1. Zetrenne E, Kosins AM, Wirth GA, Bui A, Evans GR, Wells JH. Academic plastic surgery: a study of current issues and future challenges. Ann Plast Surg. 2008;60(6):679-83.
2. Wong M, Jones S, Sheikh H, James N. The effect of the new deal on the operative experience of plastic surgical SHOs. J Plast Reconstr Aesthet Surg. 2006;59(3):311-2.
3. Lima DA, Minakami DA, Pereira LC, Grando MC, Cruz RS, Braga AR, et al. Gluteoplastia de aumento: a importância do ensino na formação atual do residente frente à demanda crescente. Rev Bras Cir Plást. 2011;26(1):127-33.
4. Monteiro LLF, Cunha MS, Oliveira WL, Bandeira NG, Menezes JV. Ligas acadêmicas: o que há de positivo? Experiência de implantação da Liga Baiana de Cirurgia Plástica. Rev Bras Cir Plást. 2008;23(3):158-61.
5. Pochat VD, Mendes RRS, Figueredo AA, Alonso N, Cunha MS, Meneses JVL. Atividades de dissecção de cadáveres e residência médica: relato da experiência do Serviço de Cirurgia Plástica do Hospital Universitário Professor Edgard Santos da Universidade Federal da Bahia. Rev Bras Cir Plást. 2011;26(4):561-5.
6. Ruiz RO, Londono ERO, Barbosa MAA, Orgaes FS, Gonella HA. Metodologia do ensino para o treinamento do tratamento não cirúrgico da área de sulco nasogeniano e região peribucal para residentes de cirurgia plástica. Rev Bras Cir Plást. 2007;22(2):67-75.
7. Dias IS, Pessoa SGP, Benevides NA, Macêdo JE. Treinamento inicial em microcirurgia. Rev Bras Cir Plást. 2010;25(4):595-9.
8. Brasil. Lei Nº 11.381, de 1º de dezembro de 2006 que dispõe sobre as atividades do médico residente. Disponível em: www.planalto.gov.br/ccivil_03/_...2006/2006/Lei/L11381.htm Acesso em: 1/3/2012.
9. Brasil. Comissão Nacional de Médicos Residentes. Disponível em: portal.mec.gov.br/index.php?id=12233&option=comcontent Acesso em: 20/3/2012.
10. Brasil. Sociedade Brasileira de Cirurgia Plástica. Regulamento interno do Departamento de Ensino dos Serviços Credenciados da SBCP. Disponível em: http://www2.cirurgiaplastica.org.br/images/Docs/regimentos/regimentoDESC.pdf. Acesso em: 21/3/2012.
11. Noone RB, Goldwyn RM, McGrath M, Spear S, Evans GR. 50th Anniversary Plastic Surgery Research Council Panel on the Future of Academic Plastic Surgery. Plast Reconstr Surg. 2007;120(6):1709-21.
12. Graduate Medical Education. Disponível em: http://www.amaassn.org/ama/pub/education-careers/graduate-medicaleducation/freida-online.shtml Acesso em: 1º/3/2011.
13. Pinder RM, Urso-Baiarda F, Knight SL. Decades of change in plastic surgery training. J Plast Reconstr Aesthet Surg. 2010;63(8):e662-3.
14. Rinard JR, Mahabir RC. Successfully matching into surgical specialties: an analysis of national resident matching program data. J Grad Med Educ. 2010;2(3):316-21.
15. Carol SM, Kennedy AM, Traynor O, Gallagher AG. Objective assessment of surgical performance and its impact on a national selection program of candidates for higher surgical training in plastic surgery. J Plast Reconstr Aesthet Surg. 2009;62(12):1543-9.
16. The European Working Time Directive. Disponível em: http://www.nhsemployers.org/planningyourworkforce/MedicalWorkforce/ewtd/Pages/EWTD.aspx Acesso em: 20/3/2012.
17. National Resident Matching Program. Disponível em: http://www.nrmp.org/data/index.html Acesso em: 5/4/2013.
18. Jalali M, Abood A, Flint LA, Pinder RM, Majumder S. Skills courses in plastic surgery: impact of enhancing confidence, skills and understanding amongst junior doctors. J Plast Reconstr Aesthet Surg. 2011;64(7):976-8.
19. Davis CR, O'Donoghue JM, McPhail J, Green AR. How to improve plastic surgery knowledge, skills and career interest in undergraduates in one day. J Plast Reconstr Aesthet Surg. 2010;63(10):1677-81.
20. Hacikerim Karşidağ S, Ozkaya O, Uğurlu K, Baş. L. The practice of plastic surgery in emergency trauma surgery: a retrospective glance at 10,732 patients. Ulus Travma Acil Cerrahi Derg. 2011;17(1):33-40.
21. Tanna N, Boyd JB, Kawamoto HK, Miller TA, Da Lio AL, Azhar H, et al. Reconstructive surgery training: increased operative volume in plastic surgery residency programs. Plast Reconstr Surg. 2012;129(3):781-8.
22. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-8.
1. Plastic Surgeon at the Sarah Brasilia Hospital, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), President of the Regional Section, Distrito Federal of the SBCP, Brasília, DF, Brazil
2. Plastic Surgeon, full member of the SBCP, Member of the Scientific Committee of the Regional Section, Distrito Federal of the SBCP, Brasília, DF, Brazil
3. Plastic Surgeon, full member of the SBCP, Member of the Scientific Committee of the Regional Section, Distrito Federal of the SBCP, Preceptor of the accredited service at the Hospital Regional da Asa Norte, Brasília, DF, Brazil
Correspondence to:
Kátia Torres Batista
SQN, 115 - Bloco I - ap. 205 - Asa Norte
Brasília, DF Brazil - CEP 70772-090
E-mail: katiatb@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article submitted: August 5, 2012
Article accepted: December 10, 2012
This study was performed at the Regional Section Distrito Federal of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter