

Original Article - Year 2012 - Volume 27 -
Augmentation mastoplasty with silicone implant associated with mastopexy through an initial periareolar approach (safety pocket)
Mastoplastia de aumento com inclusão de implante de silicone associado a mastopexia com abordagem inicial periareolar (safety pocket)
ABSTRACT
BACKGROUND: Mastopexy with breast implant surgery is a challenging and highly complex surgical procedure. In Brazil, there is growing interest in larger breast volumes, although in certain cases, the sole addition of silicone implants is not sufficient for constructing a conical breast with a full upper pole. To obtain this result, it is necessary to correct sagging breasts by removing excess skin.
METHODS: The initial approach was made with an inferior semicircular periareolar incision, which provided subfascial access to the breast pocket for inclusion of the implant. After implant placement, the excess skin was marked using simple stitches and staining with methylene blue prior to resection. Longitudinal spindle marking was preferred whenever possible. However, "L" or inverted "T" markings were also used when excess skin amounts were greater.
RESULTS: We analyzed 49 patients aged 20-68 years, of whom 28 were undergoing primary breast surgery and 21 were undergoing secondary breast surgery. The surgeries for breast pexia included L-shaped scars in 23 patients, T-shaped scars in 8 patients, and vertical scars in 18 patients. Six complications were observed in this group of patients: hematoma (n = 2), scar retraction (n = 2), severe ecchymosis (n = 1), and steatonecrosis (n = 1).
CONCLUSIONS: The conservative skin removal approach after prosthesis implantation, periareolar access, and use of the subfascial plane are the differential and relevant points of this technique. This technique is also considered safer because the periareolar incision caused the only loss of continuity in the tissues. Therefore, the prosthesis was not exposed during mastopexy.
Keywords: Mammaplasty. Breast/surgery. Breast implantation.
RESUMO
INTRODUÇÃO: A mastopexia com inclusão de implante mamário é uma cirurgia desafiadora e de alta complexidade. No Brasil, observa-se crescente interesse pelo volume mamário maior; entretanto, em certos casos, apenas a inclusão do implante de silicone não é suficiente para confecção de uma mama cônica e de polo superior cheio. Para obtenção desse resultado é necessária a correção da flacidez cutânea mamária, com retirada do excesso de pele.
MÉTODO: A abordagem inicial foi realizada com incisão periareolar semicircular inferior, que serviu como acesso à loja mamária em plano subfascial para inclusão do implante. Após o posicionamento do implante, o excedente de pele foi analisado com pontos simples e marcação com azul de metileno previamente à secção cutânea. Sempre que possível, a marcação em fuso longitudinal foi preferida, mas também foi utilizada a marcação em "L" ou "T" invertido, quando o excesso de pele era maior.
RESULTADOS: Foram analisadas 49 pacientes, com idades entre 20 anos e 68 anos, sendo 28 mamas primárias e 21 mamas secundárias. As cirurgias para pexia de mamas com cicatriz resultante em "L" foram realizadas em 23 pacientes, em "T", em 8 casos, e cicatriz vertical, em 18. Foram observadas 6 complicações nesse grupo de pacientes: hematomas (n = 2), retração cicatricial (n = 2), equimose intensa (n = 1) e esteatonecrose (n = 1).
CONCLUSÕES: A conduta conservadora da retirada de pele após o implante das próteses, a via de acesso periareolar e a utilização do plano subfascial são pontos diferenciais e relevantes dessa técnica. Essa técnica é considerada também mais segura, pois a única perda da solução de continuidade do meio com os tecidos se dá pela incisão periareloar. Dessa forma, não há exposição da prótese ao ser confeccionada a mastopexia.
Palavras-chave: Mamoplastia. Mama/cirurgia. Implante mamário.
The correction of different degrees of breast ptosis includes resection of excess skin as well as repositioning of the nipple-areolar complex (NAC) at the apex of the breast cone1.
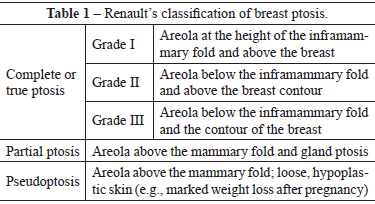
The most widely adopted classification of breast ptosis was described by Regnault2 in 1976. This classification has 3 distinct degrees based on NAC height in relation to the inframammary fold. Two intermediate forms, namely, partial ptosis and pseudoptosis, were also described (Table 1).
In Brazil, there is growing interest in the association of silicone prosthesis implant surgery with the correction of pre-existing breast ptosis because of the inability of augmentation mastoplasty to correct sagging skin and the patients' demand for a larger breast volume. Moreover, the use of surgical correction of ptosis simply repositions the pre-existing tissues and cannot restore the texture of a young breast.
Several authors have reported the presence of breast ptosis in patients who wish to undergo prosthesis implantation in combination with breast pexia surgical techniques because augmentation mastoplasty for the correction of breast ptosis tends to increase the degree of ptosis1,3-5.
This article proposes a surgical maneuver that provides greater safety for breast implants and lower visibility and palpation of the edges of breast implants in the lower pole of the breast. The prosthesis remains protected because of the breast tissue (glands and subcutaneous tissue) integrity within the lower pole of the breast, where only skin is removed.
METHODS
Marking of the breast skin was performed with the patient in an orthostatic position. The points of the sternal notch and acromion were tagged, and the midpoint between these 2 points and the midclavicular line was set.
The median of the breast was drawn and Pitanguy point A, the apex of the future NAC, was marked. The excess skin was marked so that it could be removed in the perioperative period after insertion of the mammary prosthesis. The patient was then positioned on the operating table in the supine position with the arms parallel and juxtaposed to the body.
Under sedation assisted by the anesthesiologist, strict asepsis with 4% chlorhexidine digluconate solution and 2% alcoholic chlorhexidine was performed, followed by placement of sterile surgical fields. These fields allow visualization of the shoulders and cervical region as reference anatomical elements determined by the breasts.
The breast boundaries and incision sites in the periareolar regions were marked with methylene blue. The areolae were marked with a 4.5-cm-diameter areola cutter. The breast was infiltrated with saline solution comprising 0.9% sodium chloride combined with 1% lidocaine and epinephrine (1:500,000 IU).
A semicircular skin incision was made in the lower portion of the areola, and access to the mammary pocket was accomplished through the lower portion of this incision (Webster). Skin, subcutaneous tissue, and breast glandular tissue were incised in this sequence in a 90º inclination to reach the fascia of the pectoralis major muscle (Figure 1).
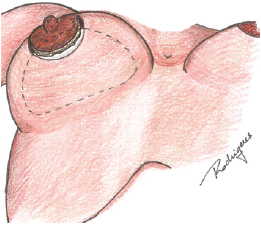
Figure 1 - Periareolar incision and inclusion of the prosthesis.
The retromammary pocket was constructed in the upper pole of the breast. The plane was retrofascial in the lower pole. The breast implant was included after hemostasis and cavity review. During pocket construction, emergence of the neurovascular pedicle in the fourth intercostal space was observed in the outer lower quadrant. This pedicle should not be damaged because it is responsible for innervation of the NAC. Suturing was performed using poliglecaprone 3.0 in the anatomical planes.
A vertical suture of the skin was completed to adjust the excess skin in the area between the nipple and the inframammary fold using a 3.0 nylon monofilament suture (Figure 2). After the necessary tension was checked, the stitches were removed and methylene blue was used to mark the excess skin to be removed (Figures 3 and 4). Thus, the excess skin observed after inclusion of the breast implant can be safely removed (Figure 5). Whenever possible, longitudinal markings were preferred. We also used "L" or "T" markings when there were greater amounts of excess skin.
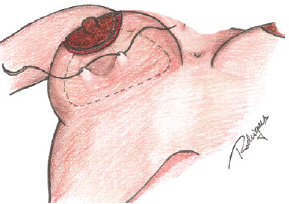
Figure 2 - Vertical suture of the skin to adjust for excess skin in the area between the areola and the inframammary fold.
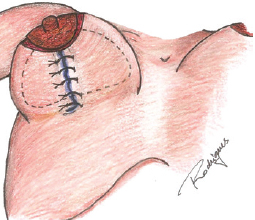
Figure 3 - Marking with methylene blue after the vertical skin suture.
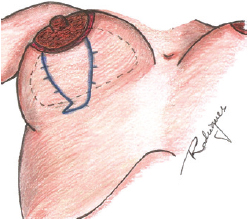
Figure 4 - Skin marking with methylene blue after suture removal.
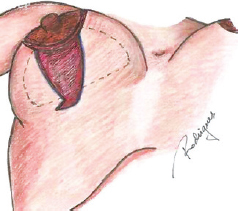
Figure 5 - Surgical appearance after skin decortication.
The neoareola was marked to maintain a distance of 4.5-6.5 cm between the lower portion of the NAC and the inframammary fold. The areola cutter was used to correct possible sagging periareolar skin. The NAC was repositioned with simple poliglecaprone 5.0 sutures in the subdermal plane and 4.0 polypropylene sutures in the intradermal plan.
RESULTS
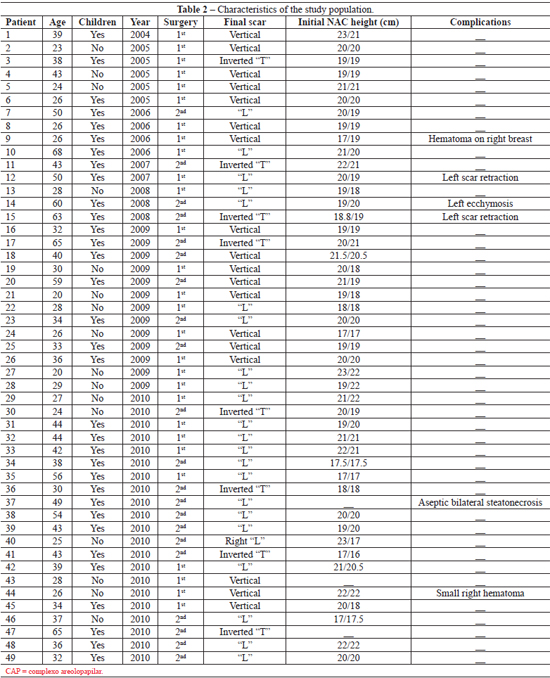
We analyzed 49 patients aged 20-68 years. Of these, 28 were undergoing primary breast surgery and 21 were undergoing secondary breast surgery (Table 2).
The prostheses used were textured cohesive gel implants that varied in volume as needed for each patient, with a mean volume of 155 ± 20 mL. Patients were followed for at least 48 months. The surgeries for breast pexia included L-shaped scars in 23 patients, T-shaped scars in 8 patients, and vertical scars in 18 patients.
Six complications were observed in this group of patients: hematoma (n = 2), scar retraction (n = 2), severe ecchymosis (n = 1), and steatonecrosis (n = 1). The most serious complication occurred in a smoker aged 49 years who had undergone a prior mammoplasty. This patient reported that she was not smoking currently. On the 10th day after surgery, intense bilateral aseptic steatonecrosis was observed and then confirmed by culture and antibiogram. Ten sessions of hyperbaric oxygen therapy were performed. Closure of the periareolar dehiscence was possible without a major aesthetic impact.
Figures 6 to 9 illustrate some cases in this series.
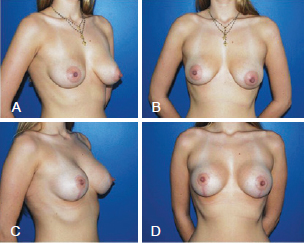
Figure 6 - Patient who underwent augmentation mastoplasty with the inclusion of silicone implants associated with the initial periareolar approach mastopexy. In A and B, preoperative appearance. In C and D, 1 year postoperative appearance.
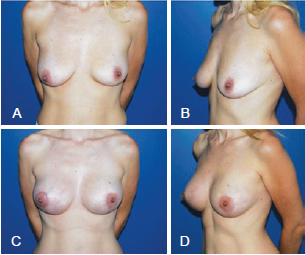
Figure 7 - Patient who underwent augmentation mastoplasty with the inclusion of silicone implants associated with the initial periareolar approach mastopexy. In A and B, preoperative appearance. In C and D, 1 year postoperative appearance.
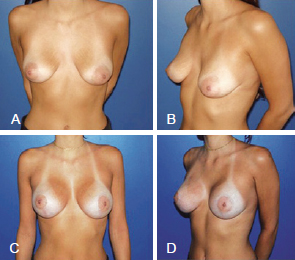
Figure 8 - Patient who underwent augmentation mastoplasty with the inclusion of silicone implants associated with the initial periareolar approach mastopexy. In A and B, preoperative appearance. In C and D, 1 year postoperative appearance.
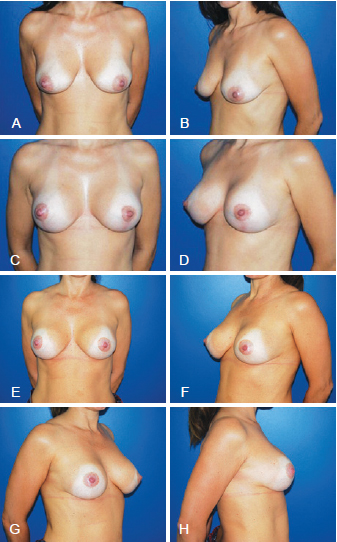
Figure 9 - Patient who underwent augmentation mastoplasty with the inclusion of silicone implant associated with the initial periareolar approach mastopexy. In A and B, preoperative appearance. In C and D, 1 year postoperative appearance. In E, F, G, and H, 5 years postoperative appearance.
DISCUSSION
Augmentation mastoplasty associated with mastopexy, which has always been a controversial issue, has been discussed by several authors5-8 since its initial description in 1960 by Gonzalez-Ulloa9.
In 2003, Carramashi & Tanaka4 found that the combination of pexia and prosthesis provided adequate volume and shape for the treatment of the sequelae of reductive mastoplasty.
In 2008, Sanchez et al.10 suggested the use of an inferior pedicle to protect breast implants. Soares et al.11 proposed the construction of a dual space consisting of an upper subglandular space and a lower submuscular space for placing the implant. In 2008, Gomes7 described a mastopexy technique with breast augmentation that used a superior pedicle flap surrounding the implant.
In 2009, Mansur & Bozola12 reported the use of an inferior breast pedicle to protect and support the breast implant and prevent it from sliding down the mammary fold and emptying the bosom. These authors12 also observed alleviation in patient discomfort on palpation of the implants in the lower pole.
In 2003, Graf et al.13 described a new approach to breast augmentation in which the prosthesis was positioned in the subfascial plane. These authors observed lower visibility of the prosthesis with greater protection because the new structure was added between the skin, subcutaneous tissue and the implant. In these operations, the anatomical planes of the inferior pedicle are sectioned; this may expose the prosthesis in the case of dehiscence.
Preservation of the tissue integrity of the lower pole was a relevant factor in this study because the only communication between the breast pocket and the skin lies in the lower periareolar region. The implants are protected from the external environment and are not supported on flaps or surgical incisions.
A decrease in palpation of the prosthesis and external evidence of its edges occurred due to the placement of the implants in the retrofascial plane only in the inferior pole of the breast. Preservation of the neurovascular pedicle of the fourth intercostal space maintains NAC sensitivity and vascularization. The choice to not use flaps to cover the lower breast implant was considered positive because it avoids glandular lesions that predispose the breast to infection and the prosthesis to extrusion or exposure.
In the patient who presented with aseptic steatonecrosis, protection of the prosthesis by the unexposed glandular tissues was crucial for a favorable prognosis. We believe there was no dehiscence increase nor implant compromise in this case because we preserved the tissues intact without breaking the skin in the lower breast pole.
CONCLUSIONS
The inclusion of silicone implants followed by mastopexy using the initial periareolar approach (safety pocket) is a good option in cases of augmentation mastoplasty associated with the correction of pre-existing ptosis.
The conservative skin removal approach after implantation of the prosthesis, the vertical periareolar access, and the use of a subfascial plane are the differential and relevant points that characterize this technique.
REFERENCES
1. Regnault P. The hypoplastic and ptotic breast: a combined operation with prosthetic augmentation. Plast Reconstr Surg. 1966;37(1):31-7.
2. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
3. Pitanguy I, Carreirão S, Mazzarone F, Fróes LB, Cló TT. Mastopexia associada à inclusão de prótese. Rev Bras Cir. 1991;81(2):101-11.
4. Carramaschi FR, Tanaka MP. Mastopexia associada à inclusão de prótese mamária. Rev Soc Bras Cir Plást. 2003;18(1):25-36.
5. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67.
6. Spear S. Augmentation/mastopexy: "surgeon, beware". Plast Reconstr Surg. 2003;112(3):905-6.
7. Gomes RS. Mastopexia com retalho de pedículo superior e implante de silicone. Rev Bras Cir Plást. 2008;23(4):241-7.
8. Chem RC. Plástica mamária estética de aumento com a utilização de próteses. Rev Soc Bras Cir Plást. 1991;6(1/2):28-32.
9. Gonzalez-Ulloa M. Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg. 1960;25(1):15-40.
10. Sanchéz J, Carvalho AC, Erazo P. Mastopexia com prótese: técnica em "D" espelhado. Rev Bras Cir Plást. 2008;23(3):200-6.
11. Soares AB, Franco FF, Rosim ET, Renó BA, Hachmann JOPA, Guidi MC, et al. Mastopexia com uso de implantes associados a retalho de músculo peitoral maior: técnica utilizada na Disciplina de Cirurgia Plástica da Unicamp. Rev Bras Cir Plást. 2011;26(4):659-63.
12. Mansur JRB, BozolaAR. Mastopexia e aumento das mamas com proteção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24(3):304-9.
13. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8.
1. Plastic Surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Tutor at the Plastic Surgery Training Center, Hospital Mater Dei (Mater Dei Hospital), Belo Horizonte, MG, Brazil.
2. MSc in Surgery, Universidade Federal de Minas Gerais (Federal University of Minas Gerais), full member of the SBCP, member of the Plastic Surgery Medical Team, Hospital Mater Dei (Mater Dei Hospital), Belo Horizonte, MG, Brazil.
3. Specialist in Plastic Surgery, Associate Member of the SBCP, Member of the Plastic Surgery Medical Team, Hospital Mater Dei (Mater Dei Hospital), Belo Horizonte, MG, Brazil.
4. Aspiring member of the SBCP, member of the Plastic Surgery Medical Team, Hospital Mater Dei (Mater Dei Hospital), Belo Horizonte, MG, Brazil.
Correspondence to:
Ataliba Ronan Horta de Almeida
Rua Gonçalves Dias, 1.181 - 1º andar - Funcionários
Belo Horizonte, MG, Brazil - CEP 30140-091
E-mail: ronan@ronanhorta.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 6, 2011
Article accepted: October 15, 2011
This work was performed at the Hospital Mater Dei (Mater Dei Hospital), Belo Horizonte, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter