

Original Article - Year 2012 - Volume 27 -
Evaluation of the L-shaped scar-reducing mastoplasty technique for breast hypertrophies
Avaliação de técnica de mastoplastia redutora com cicatriz em
ABSTRACT
BACKGROUND: Many surgeons have attempted to develop techniques to reduce the scarring resulting from mastoplasty, particularly in cases undergoing nonreducing mastopexy. The aim of this study was to evaluate an L-shaped scar-reducing mastoplasty technique used for grade II or higher mammary hypertrophies, according to the rating system of Berrocal Revueltas.
METHODS: We conducted a retrospective study of 70 patients who underwent L-shaped scar-reducing mastoplasty between April 2007 and March 2011. We included patients with Berrocal Revueltas grades II and III breast hypertrophy and gigantomastia. The surgical technique involved marking of the skin both at the beginning of surgery as well as during the surgery after the formation of the new breast cone. We evaluated the complications encountered. The quality of the results was assessed by 4 full members of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery). Statistical analysis was performed using SPSS.
RESULTS: The mean patient age was 32.9 years and 62.9% of patients were overweight. The average weight of resected tissue was 718.7 g in the right breast and 713.5 g in the left breast. Among the patients, hematoma (1.4%), seroma (2.9%), epidermolysis (1.4%), keloids (1.4%), hypertrophic scar (2.9%), and excess skin (5.7%) were noted, and the surgical reoperation rate was 8.6%. The evaluators assessed breast shape, breast symmetry, elevation of the nipple-areola complex, and scar appearance, which were considered very good (rating of 9-10) in 78.6%, 82.1%, 96.4%, and 67.9% of cases, respectively.
CONCLUSIONS: The L-shaped scar-reducing mastoplasty technique was effective for the treatment of large breast hypertrophy.
Keywords: Mammaplasty. Surgery, plastic. Breast/surgery.
RESUMO
INTRODUÇÃO: A preocupação com o aspecto das cicatrizes nas mastoplastias levou diversos cirurgiões a explorar técnicas com cicatrizes reduzidas, preferencialmente nas mastopexias não-redutoras. O objetivo deste estudo é avaliar uma técnica de mastoplastia redutora com cicatriz em "L" nas hipertrofias mamárias grau II ou maiores pela classificação de Berrocal Revueltas.
MÉTODO: Foi realizado estudo descritivo e retrospectivo, com 70 pacientes submetidas a mastoplastia redutora com cicatriz em "L", entre abril de 2007 e março de 2011. Foram incluídas pacientes portadoras de hipertrofia mamária graus 2, 3 e gigantomastia, pela classificação de Berrocal Revueltas. A técnica cirúrgica preconizou a marcação de pele em dois tempos, no início da cirurgia e no intraoperatório, após formação do novo cone mamário. Foram avaliadas as complicações encontradas. A qualidade dos resultados foi avaliada por 4 membros titulares da Sociedade Brasileira de Cirurgia Plástica. A análise estatística foi realizada com auxílio do programa SPSS.
RESULTADOS: A média de idade das pacientes foi de 32,9 anos e 62,9% apresentavam sobrepeso. A média de peso do tecido ressecado foi de 718,7 g na mama direita, e de 713,5 g na mama esquerda. Foi evidenciada taxa de 1,4% de hematoma, 2,9% de seroma, 1,4% de epidermólise, 1,4% de queloide, 2,9% de cicatriz hipertrófica e 5,7% de excesso de pele, sendo a taxa de reabordagem cirúrgica de 8,6%. Os avaliadores consideraram forma, simetria, ascensão do complexo areolopapilar e cicatriz das mamas muito boa (9 a 10) em 78,6%, 82,1%, 96,4% e 67,9% dos casos, respectivamente.
CONCLUSÕES: A mastoplastia redutora com cicatriz em "L" se mostrou eficaz para o tratamento das grandes hipertrofias mamárias.
Palavras-chave: Mamoplastia. Cirurgia plástica. Mama/cirurgia.
Various techniques have been described for the treatment of hypertrophy of the breast, which is commonly associated with physical and emotional distress in females. The first breast hypertrophy surgery was performed in the 19th century by Dieffenbach1. Since then, several techniques have been described for reducing breast volume2-10, correcting breast ptosis11-13, and minimizing scarring14-20. The "L"-shaped scar technique, first described by Hollander14, has since received contributions from several other surgeons in its evolution to the technique used at present. The main concern of the surgeons who perform these procedures is minimizing the resultant scarring, which is associated with good aesthetic results. Aspects such as resulting breast shape, procedural safety, and technical difficulties that hamper its reproduction by other surgeons are its main limitations.
The L-scar mastoplasty has been used for many years, particularly in cases requiring mastopexy without breast volume reduction. The aim of this study was to evaluate L-scar reducing mastoplasty technique for the treatment of breast hypertrophy grade II or higher according to the rating system of Berrocal Revueltas21.
METHODS
Study Sample
We conducted a retrospective study involving 70 female patients who underwent L-scar reduction mastoplasty between April 2007 and March 2011. All patients signed an informed consent form.
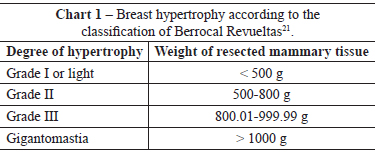
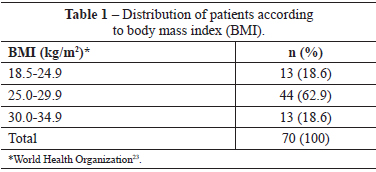
The following inclusion criteria were established: age > 16 years, body mass index (BMI) < 35 kg/m2, and the presence of grades II and III breast hypertrophy and gigantomasty according to the classification of Berrocal Revueltas21 (Table 1).
The exclusion criteria included BMI > 35 kg/m2, previous diagnosis of breast malignancy, prior breast surgery, and decompensating systemic diseases.
The patients were operated by the same surgical team using a standard technique. The surgeries were preceded by anamnesis, physical examination, laboratory evaluations, cardiac evaluations, screening of breast disorders by ultrasonography, and mammography in patients aged > 35 years.
Surgical Technique
After anesthesia, antisepsis, and asepsis, Aufricht22 thoracic markings were made. The Pitanguy7 point A was then marked (Figure 1). Points B and C were marked by bidigital clamping of the excess skin to be resected in an attempt to place point A in the future apex of the breast (Figure 2). Points B and C were then joined by a semicircular line with the concavity facing the nipple-areolar complex (NAC).

Figure 1 - Marking of point A.

Figure 2 - Marking of points B and C.
The skin incision was performed based on the marking, and de-epithelialization of the NAC was then performed using the Schwartzmann2 maneuver. The lower pole of the breast was detached from the skin up to the internal inserts of the submammary groove and extended medially and laterally (Figure 3). The breast was then detached to the level of the pectoral fascia and separated from the chest wall. Resection of the inferior pole and a keel-shaped resection of the medial part of the remaining breast was performed to create 2 pillars, one medial and one lateral. Resection of the pillar base was performed to make them regular and symmetrical (Figure 4).
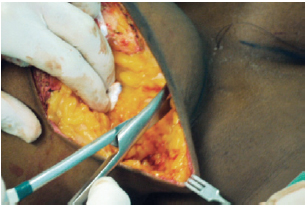
Figure 3 - Detachment of the upper pole.

Figure 4 - Resection of the pillar base.
The upper pole was then fixed in the upper third fascia of the pectoral muscle. The medial and lateral pillars were approached and a temporary suture of the skin was created by connecting points B and C, thereby forming the new breast cone (Figure 5).

Figure 5 -Temporary skin suture used to form the new breast cone.
Thereafter, the excess skin was marked and resected on the vertical line of the L-shaped scar. The NAC was subsequently released using a Skoog lateral flap5. The breast cone was then reassembled.
We made intraoperative markings of the inferolateral right point to preserve the minimum possible distance of B to C from the new submammary groove and accommodate the excess skin on the horizontal line of the L-shaped scar. Resection of the excess skin and a final intradermal suture were subsequently performed (Figure 6).
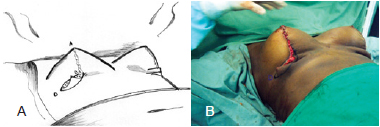
Figure 6 - Marking of point D to remove the excess skin. In A, schematic drawing. In B, intraoperative appearance.
The location of the new areola was marked at the apex of the breast, with complementary de-epithelialization and transposition of the markings to the contralateral breast. The NAC was fixed at 4 cardinal points using nylon 5.0 sutures. Intradermal suturing was performed using absorbable monofilament 4.0 sutures (Figure 7). A separate sterile micropore dressing was used for each breast and then a bra was placed and maintained for 60 days.

Figure 7 - Final suture appearance.
Postoperative follow-up was conducted at 24 hours for surgical drain removal and a dressing change. The second dressing change was performed on the fourth postoperative day. Weekly evaluations were made in the first month and then monthly until the third postoperative month. After the incisions healed, the dressings were replaced with silicone strips.
We assessed each patient's nutritional status and degree of preoperative breast hypertrophy. The postoperative presence of surgical wound complications, infection, and healing abnormalities was also analyzed.
To evaluate the quality of the results, pre- and postoperative photographs were analyzed by 4 full members of the Brazilian Society of Plastic Surgery (Figures 8 to 11). Shape, symmetry, and elevation of the NAC as well as appearance of the scar were classified as bad (0-3), regular (4-6), good (7-8), or very good (9-10).
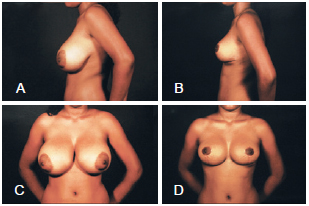
Figure 8 - In A and C, lateral and frontal preoperative view, respectively. In B and D, lateral and frontal postoperative views, respectively.
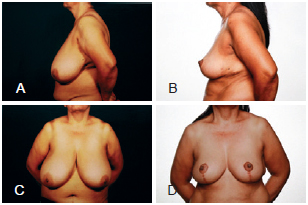
Figure 9 - In A and C, lateral and frontal preoperative views, respectively. In B and D, lateral and frontal postoperative views, respectively.
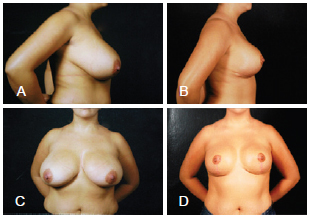
Figure 10 - In A and C, lateral and frontal preoperative views, respectively. In B and D, lateral and frontal postoperative views, respectively
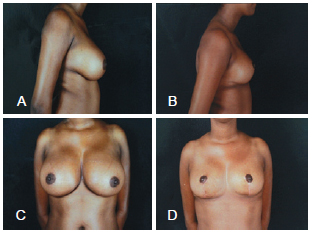
Figure 11 - In A and C, lateral and frontal preoperative views, respectively. In B and D, lateral and frontal postoperative views, respectively.
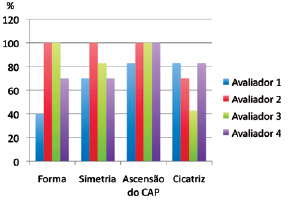
Figure 12 - Evaluation of results by 4 independent raters according to the following parameters: breast shape, breast symmetry, nipple-areolar complex (NAC) elevation, and scar appearance.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) for Windows version 15.0.
RESULTS
We analyzed the medical records of 70 female patients who underwent L-scar reduction mastoplasty from April 2007 to March 2011. The mean patient age was 32.9 ± 10.6 years (range, 16-61 years). The mean BMI was 27.3 ± 2.9 kg/m2 (range, 20.9-33.1 kg/m2). The patient distribution according to BMI is shown in Table 1. Three (4.3%) patients were smokers.
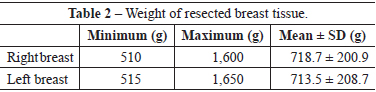
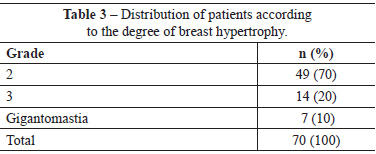
An average of 718.7 ± 200.0 g and 713.5 ± 208.7 g of breast tissue was resected from the right and left breasts, respectively (Table 2). Forty-nine (70%) patients had grade II breast hypertrophy according to the classification of Berrocal Revueltas21 (Table 3).
The major complications presented by this group of patients are listed in Table 4. Among these complications, only 6 (8.6%) patients required surgical reoperation (Table 5).
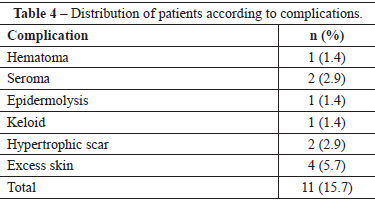
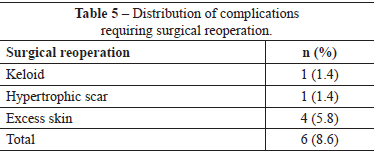
Figure 12 presents the results of the evaluation conducted by 4 independent raters according to breast form, breast symmetry, and NAC elevation as well as scar appearance.
DISCUSSION
Surgical procedures involving reduced scarring mastoplasty have the benefit of eliminating or drastically reducing the horizontal component of the scar and are gaining popularity in Brazil and other countries24. The L-shaped scar techniques, such as those described by Sepúlveda16, Bozola17, Chaves et al.18, Chiari19, and D'Assumpção20, result in good projection of the breast and avoid the premature emptying of the upper breast pole. These techniques are reproducible, although they are associated with a long learning curve. The technique described in this study indicates that preoperative skin marking does not need to be completely defined at the beginning of surgery, as recommended by Wise6, since point D is marked intraoperatively only after defining the new inframammary fold.
We evaluated all patients with grade II or higher breast hypertrophy (according to the classification of Berrocal Revueltas21) who underwent surgery between 2007 and 2011; at this time, the described technique had already been used by the surgeon for 7 years and, therefore, the surgical parameters were well defined.
The Berrocal Revueltas classification21 was used because it is an objective method for classifying breast hypertrophy and is based on the weight of the resected breast tissue. Glandular tissue resection was performed considering the needs of each patient, according to the symptoms presented, the patient's desire, and the anatomy of the thoracic region, to avoid compromising the final aesthetic result.
Overweight and obesity are commonly associated with breast hypertrophy since the amount of fatty tissue surrounding the mammary gland is primarily responsible for its volume25. Most of the patients in this study were overweight, which a finding similar to that observed a study by Rocha et al.26, in which 57.6% of patients had a BMI > 25 kg/m2.
Patients who met the exclusion criteria were not operated upon due to lack of safety, as decided by the surgical the team. Smokers were not excluded, although this factor can influence the safety of the described technique.
The breast markings were performed in 2 stages, at the beginning of surgery with the patient already anesthetized as well as intraoperatively. The initial marking included only points A, B, and C, as defined by Pitanguy7, and an arched line connecting points B and C. This type of simplified marking does not increase the surgical time. Additional marking was performed intraoperatively after the new inframammary fold was identified, and consisted of point D, which corresponded to the inferolateral extreme of the horizontal line of the L-shaped scar. Thus, the surgeon was not required to predict the location of the new inframammary fold at the height of the thorax and the L-shaped scar prior to the surgery. This maneuver differs from that proposed by Chiari19, who used preoperative geometric marking based on a value X, which corresponded to the distance between the right and left axillary grooves divided by 4. It also differs from the technique proposed by Bozola17, which adjusted the skin and subcutaneous tissue starting from the inferolateral edge of the horizontal line of the L-shaped scar toward the apex of the cone, where the compensation was made in the periareolar region. D'Assumpção20 proposed the use of molds and Wolf et al.27 proposed marking by means of single intersecting horizontal and vertical spindles. These authors made their markings at the beginning of the surgical technique.
A keel-shaped resection of the breast was performed as recommended by Pitanguy7. We used Skoog's superolateral flap5 to elevate the NAC because of the safety associated with its use, due to its vascularization by the external mammary artery.
In order to accurately mark point D, we emphasize that it is essential to remove any excess skin on the vertical line of the L-shaped scar. The excess inferolateral skin can then be resected with greater accuracy.
Individual micropore sterile dressings were used for each breast in an attempt to provide greater patient comfort. The dressings and subsequent wearing of the bra that accompanies the retraction of the breast skin were performed, as described by Peixoto15.
The complication rate was 15.7%. The most frequent complications were excess skin and hypertrophic scarring. Dabbah et al.28 conducted a retrospective study of different T-shaped scar techniques and found that the most frequent complications were infection and lipolysis. The absence of infection in this study may be due to the fact that all patients were operated on in a day hospital specializing in plastic surgery, in which no other types of surgeries are performed.
Patients with hypertrophic scars and keloids as well as those who had remnant excess skin underwent surgical resection of the affected scar segment under local anesthesia; the surgical reoperation rate was 8.6%. Beer et al.29 reported a reoperation rate of 11.1% in 153 patients, whereas Davis et al.30, in a study that included 406 patients, noted the need for surgical reoperation in 5% of cases.
Beer et al.29, studying the technique of reducing mastoplasty with a vertical scar, reported major complications of breast asymmetry in 26% and suture dehiscence in 12.6% of cases. In the present study, 4 independent observers rated the breast shape and symmetry as very good (rating of 9-10) in 78.6% and 82.1% of subjects, respectively. This may be due to the fact that the L-shaped scar is longer than the vertical scar and allows for greater correction of asymmetry.
Seroma, which was observed in 2.9% of patients, can be attributed to the absence of breast liposuction in the technique described. Beer et al.29, who also rarely perform breast liposuction, observed an incidence of 0.7% of seroma in these cases. However, Lejour32, who use liposuction in their technique, observed a 5% seroma rate. In the present study, 2 (2.9%) patients with seroma underwent ambulatory drainage with a syringe to treat the complication.
Only 1 (1.4%) patient exhibited hematoma in the present study, and this condition was evident on the first postoperative day and was treated with ambulatory drainage.
NAC transposition was achieved in all cases without any evidence of necrosis, and the observers rated the obtained elevation as very good in 96.4% of cases. This can be explained by the fact that the sample comprised the surgeon's most recent cases, after 7 years of experience with the technique. Furthermore, the rate of smokers among the patients was only 4.3%.
The one (1.4%) patient who presented with epidermolysis was treated conservatively using collagenase ointment. A similar frequency (1.7%) was described by Rocha et al.26 in a retrospective study of the inferior vascular pedicle technique.
A change in the surgical planning including the need for T-shaped incisions, due to technical difficulties or to accommodate the skin, was not required. This finding is consistent with that observed by Vendette et al.32, who showed that L-shaped breast mammoplasty may be indicated for breasts with different characteristics, as long as a breast cone of proportional dimensions is used in breast modeling.
In this study, adequate shape and symmetry were achieved, which allowed for good NAC elevation, as well as similar complication and surgical reoperation rates to those noted in other studies. However, additional prospective studies are needed to better assess the long-term outcomes of this technique.
CONCLUSIONS
This L-shaped scar-reducing technique was effective for the treatment of breast hypertrophy rated as grade II or higher, according to the classification of Berrocal Revueltas21.
REFERENCES
1. Dieffenbach JF. Die operative chirurgie. apud Jones G. Breast reduction. In: Mathes S, ed. Plastic surgery. Philadelphia: Elsevier; 2006.
2. Schwarzmann E. Die technik der mammapiklast. apud Jones G. Breast reduction. In: Mathes S, ed. Plastic surgery. Philadelphia: Elsevier; 2006.
3. Biesenberger H. Eine neue methode der mammaplastik. apud Jones G. Breast reduction. In: Mathes S, ed. Plastic surgery. Philadelphia: Elsevier; 2006.
4. Strombeck JO. Mammaplasty: report of a new techniques based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79-90.
5. Skoog T. A technique of breast reduction, transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453-65.
6. Wise RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg. 1956;17(5):367-75.
7. Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20(1):78-85.
8. Weiner DI, Aiache AE, Silver L, Tittiranonda T. A single dermal pedicle for nipple transposition in subcutaneous mastectomy, reduction mammaplasty, or mastopexy. Plast Reconstr Surg. 1973;51(2):115-20.
9. Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55(3):330-4.
10. Lejour M, Abboud M. Vertical mammaplasty without inframmamary scar and with breast liposuction. Perspect Plast Surg. 1990;4:67-90.
11. Pousson M, Michel X. Sur un cas de mastopexia. apud Jones G. Breast reduction. In: Mathes S, ed. Plastic surgery. Philadelphia: Elsevier; 2006.
12. Guinard M. Rapport de l'ablation estetique des tumeurs du sein par M.H. Morestin. apud Jones G. Breast reduction. In: Mathes S, ed. Plastic surgery. Philadelphia: Elsevier; 2006.
13. Lassus C. A technique for breast reduction. Int Surg. 1970;53(1):69-72.
14. Hollander E. Die operation der mamma hypertrophy und der hagebrust. Deutsch Med. Wochenschr. 1924;50:1400.
15. Peixoto G. Reduction mammaplasty: a personal technique. Plast Reconstr Surg. 1980;65(2):217-26.
16. Sepúlveda A Tratamento das assimetrias mamárias. RevBras Cir. 1981;71(1):11-8.
17. Bozola AR. Mamoplastia em L: contribuição pessoal. Rev AMRIGS. 1982;26(3):207-14.
18. Chaves L, Ceceau MA, Magalhães HGA. Mastoplastia em "L": um novo desenho. Rev Soc Bras Cir Plást. 1988;3(1):40-8.
19. Chiari Junior A. The L short-scar mammaplasty: a new approach. Plast Reconstr Surg. 1992;90(2):233-46.
20. D'Assumpção EA. Contribuição à mamaplastia redutora em L. Rev Bras Cir Plást. 1998;13(1):51-60.
21. Berrocal Revueltas M. Mamoplastia reductora con incisión mínima en J: una alternativa ideal en el manejo de las gigantomastias. Rev Co Cir Plást. 2000;4(1):15-9.
22. Aufricht G. Mammaplasty for pendulous breasts: empiric and geometric planning. Plast Reconstr Surg. 1949;4(1):13-29.
23. Organização Mundial de Saúde. Obesity: preventing and managing the global epidemic. Genebra: Organização Mundial de Saúde; 1997.
24. Jones G. Breast reduction. In: Mathes S, ed. Plastic surgery. Philadelphia: Elsevier; 2006. p.539-84.
25. Moore KL, Dalley AF. Anatomia orientada para clínica. Rio de Janeiro: Guanabara Koogan; 2001.
26. Rocha ACJ, Costa CS, Campos H. Técnica de Costa Lima nas hipertrofias mamárias associada ao retalho de pedículo vascular inferior. Rev Bras Cir Plást. 2010;25(1):154-67.
27. Lobo AL, Caixeta RM, Tannus ED, Hernandez CHT, Maester DJ. Mamoplastia em "L": contribuição pessoal. In: Tournieux AAB, ed. Atualização em cirurgia plástica. São Paulo: Robe Editorial;1999. p. 245-9.
28. Dabbah A, Lehman JA Jr, Parker MG, Tantri D, Wagner DS. Reduction mammaplasty: an outcome analysis. Ann Plast Surg. 1995;35(4):337-41.
29. Beer GM, Spicher I, Cierpka KA, Meyer VE. Benefits and pitfalls of vertical scar breast reduction. Br J Plast Surg. 2004;57(1):12-9.
30. Davis GM, Ringler SL, Short K, Sherrick D, Bengtson BP. Reduction mammaplasty: long-term efficacy, morbidity, and patient satisfaction. Plast Reconstr Surg. 1995;96(5):1106-10.
31. Lejour M. Vertical mammaplasty: early complications after 250 personal consecutive cases. Plast Reconstr Surg. 1999;104(3):764-70.
32. Vendette FGV, Ota AS, Rebello CM, Brandão LP, Reis SR. Mamoplastia em "L": revisão de pacientes operadas no Serviço de Cirurgia Plástica do Hospital Municipal Barata Ribeiro - Rio de Janeiro. Disponível em: http://www.sbcp-sc.org.br/anais/paginas/55.htm Acesso em: 18/6/2011.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, Medical director of the Clínica Self Day (Self Day Clinic), Salvador, BA, Brazil.
2. Physician, Member of the medical staff of the Clínica Self Day (Self Day Clinic), Salvador, BA, Brazil.
3. Full professor, Escola Bahiana de Medicina e Saúde Pública (Bahia School of Medicine and Public Health), full member of the SBCP, Salvador, BA, Brazil.
Correspondence to:
João Batista Portocarrero Costa Sobrinho
Rua Monte Conselho, 742 - ap. 202 - Rio Vermelho
Salvador, BA, Brazil - CEP 41940-360
E-mail: jportocarrero@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 28, 2012
Article accepted: November 24, 2012
This study was performed at the Clínica Self Day (Self Day Clinic), Salvador, BA, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter