

Ideas and Innovation - Year 2012 - Volume 27 -
Optimization of incision marking in abdominoplasty using a standardized template
Otimização da marcação da incisão na dermolipectomia abdominal com emprego de molde padronizado
ABSTRACT
Preoperative marking of the incision in abdominoplasty plays a key role in the shape and position of the resulting scar. The undermining, traction, and resection of redundant tissue also influence these outcomes. After observation and statistical analysis of 36 abdominoplasty procedures, a preoperative marking template, which reproduces the incision shape that is considered the most suitable from an aesthetic point of view, was developed. The most suitable incision shape has 3 line segments: one central segment that is 11 cm ± 0.4 cm in length and 2 lateral segments that are 16.5 ± 2.3 cm in length at an angle of 155º. The template provides a quick, inexpensive, and consistent technique for reliably reproducing the suitable incision shape.
Keywords: Abdominoplasty. Abdomen/surgery. Cicatrix.
RESUMO
A marcação pré-operatória da incisão na dermolipectomia abdominal tem papel fundamental na forma e no posicionamento da cicatriz resultante. Além da marcação, o descolamento, a tração e a ressecção dos tecidos excedentes também contribuem para esse desfecho. Após observação e análise estatística de 36 abdominoplastias, foi desenvolvido um molde de marcação pré-operatória que reproduz a forma das incisões consideradas adequadas do ponto de vista estético. A forma de incisão considerada adequada apresenta 3 segmentos de reta: um central, de 11 ± 0,4 cm, e 2 laterais angulados em 155 graus, com 16,5 ± 2,3 cm. O molde consegue reproduzir a forma das incisões consideradas adequadas de modo rápido, barato e reprodutível.
Palavras-chave: Abdominoplastia. Abdome/cirurgia. Cicatriz.
Abdominoplasty alone, or in combination with liposuction, leaves a scar in the lower abdominal region that is primarily the result of 3 factors: incision marking; undermining and traction of the dermoadipose flap; and size and shape of the redundant tissue resection1,2.
Depending on the selected type of marking, transoperative adjustments are occasionally necessary for the creation of a suitable final scar3. In addition to the technical challenge involved, this procedure tends to increase the surgical time and the associated morbidity. Moreover, minor deviations in the marks made on a patient in the upright position may be accentuated once the patient is supine.
Although various preoperative marking routines have been described in the literature, there is no record of the systematic use of a standard template for that purpose4,5. The use of a template to standardize preoperative markings likely shortens the surgical planning time and reduces the possibility of unintentional deviations from the original drawing.
The aim of this study was to standardize and optimize the marking and incision shapes in abdominoplasty surgery with the use of a preoperative marking template.
METHODS
Thirty-six patients who underwent abdominoplasty with or without liposuction were enrolled from July 2009 to March 2011. All patients were operated on using the same technical approach.
A study of the enrolled patients' scars resulting from the was conducted using digital photographs taken after a minimum period of 6 months postoperatively. The analysis was divided into 2 parts:
1. analysis of digital photographs using Mirror software version 6.0;
2. analysis of digital photographs using the Strasser scale6 for aesthetic outcomes.
Based on the standardized measures obtained after analysis of the resulting scars, a malleable polyurethane template was manufactured to allow for scar reproducibility.
The Template
The original template is shown in Figure 1. The dimensions of the polyurethane template are presented in Figure 2. The template was manufactured using polyurethane because it is a malleable, easily reproduced, and inexpensive material. A liquid-filled leveling device was added to ensure that the template could be positioned such that the central line segment was always parallel to the ground.
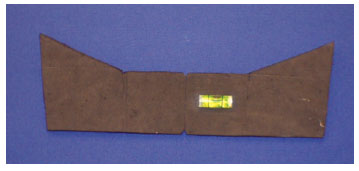
Figure 1 - Original preoperative marking template.
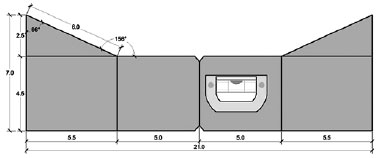
Figure 2 - Dimensions of the polyurethane preoperative marking template.
In addition, the template has 2 central marks that allow for alignment with the vulva and the umbilicus, further improving the positioning and symmetry of the resultant marking.
Once the template was positioned, the preoperative marking was executed using a dermographic pen (Figures 3 to 5). The lateral extensions of the template are 7 cm in length, which yields an overall compact size for use and portability. In fact, the size of these lateral extensions can be increased according to the surgeon's needs, but the angles should always be similar to those of the master template. Moreover, the correct leveling should also be maintained.

Figure 3 - Marking performed during the preoperative period of the abdominoplasty using the proposed template and a dermographic pen.
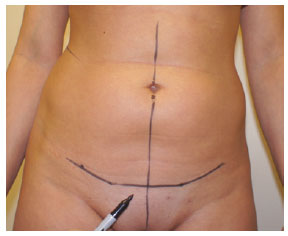
Figure 4 - Marking performed during the preoperative period of the abdominoplasty consisting of 3 line segments: one lower central segment parallel to the ground that is connected to 2 angled line segments.
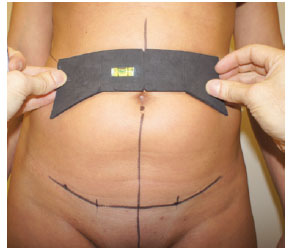
Figure 5 - Marking performed during the preoperative period of the abdominoplasty using the proposed template.
RESULTS
Strasser Scale
The Strasser scale6 was applied to the photographs and enabled the identification of a suitable scar pattern according to current aesthetic standards.
According to this evaluation, the scars that were considered the most suitable had 3 line segments: one lower central segment, parallel to the ground, that connects to 2 angled line segments (Figure 4). The angles varied, ranging from well-defined angles to nearly the full curvature of the incision.
Mirror Software
Analysis of the digital photographs using the Mirror software revealed a pattern for the measures of the segments that were most suitable, according to the results of the Strasser scale for aesthetic outcomes. Statistical analysis of the measures yielded the following results:
1. a central line segment that is 11 ± 0.4 cm in length;
2. oblique lateral line segments that are 16.5 ± 2.3 cm in length;
3. an angle between the central segment and the oblique lateral extensions that measures 155º ± 2º.
A template was manufactured based on these statistical results.
DISCUSSION
The preoperative marking, the dermoadipose undermining, and the resection shape and size all contribute to the shape and positioning of the final scar7,8. These elements, together with scar tissue quality, contribute to the satisfactory aesthetic outcome of the surgery. A well-planned cutaneous marking still often results in an asymmetrical, distorted, or poorly positioned scar. The main causes for this outcome are as follows: insufficient or inadequate undermining; asymmetrical traction; and resection of various dermoadipose portions.
Minor deviations in the marking made on a patient in an upright position can be accentuated when the patient is in a supine position. Tissue movement that results from sagging can change the marking and the anatomical references, leading to an inappropriate incision that differs from the planned incision. Scars in the abdominal or supra-pubic regions, such as the Pfannenstiel scar, can provide misleading reference points since they often do not precisely follow the anatomical boundaries9. In addition, a study conducted by Rohrich et al.10 showed that the umbilicus (an important anatomical reference) is not always precisely located in the midline. It is not uncommon for a surgeon to perform additional resections and adjustments to create symmetry or improve the positioning of the scar at the end of the procedure.
Although the scar's final aspect and position are determined by multiple factors, it is essential to attempt to reduce the risk of distortion in the final result. Thus, standardizing the marking procedure can contribute to at least 2 important surgical aspects: reducing the marking and adjusting time; and creating reproducible results. The development of a flexible template will likely address these requirements. Moreover, the template is applicable to all cases, inexpensive, and easily reproduced.
The fact that the standard template is based on the evaluation of the satisfactory aesthetic results increases its external applicability since it uses clinical parameters instead of only geometrical measures.
In the marking process, the presence of existing scars as well as deviations or asymmetries, such as scoliosis, shortened lower limbs, and umbilicus deviation from the midline, can change important anatomical references. This is why the leveling device included in the template presented here is important, since it allows the marking to be adjusted to a patient's anatomical characteristics and facilitates the perception and treatment of such distortions.
CONCLUSIONS
The template described here provides a preoperative marking standard, and is an inexpensive and easy-to-manufacture device. Further studies of the use of this device are necessary to confirm the reproducibility of its results.
REFERENCES
1. Nahas FX. A pragmatic way to treat abdominal deformities based on skin and subcutaneous excess. Aesthetic Plast Surg. 2001;25(5):365-71.
2. Pitanguy I. Abdominal plastic surgery. Hospital (Rio J). 1967;71(6):1541-56.
3. Pechter EA. Instant identification of redundant tissue in abdominoplasty with a marking grid. Aesthet Surg J. 2010;30(4):571-8.
4. Momeni A, Heier M, Bannasch H, Torio-Padron N, Stark GB. The "rising-sun-technique" in abdominoplasty. Ann Plast Surg. 2008;60(4):343-8.
5. Sozer SO, Agullo FJ, Santillan AA, Wolf C. Decision making in abdominoplasty. Aesthetic Plast Surg. 2007;31(2):117-27.
6. Strasser EJ. An objective grading system for the evaluation of cosmetic surgical results. Plast Reconstr Surg. 1999;104(7):2282-5.
7. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93.
8. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
9. El-Khatib HA, Bener A. Abdominal dermolipectomy in an abdomen with pre-existing scars: a different concept. Plast Reconstr Surg. 2004;114(4):992-7.
10. Rohrich RJ, Sorokin ES, Brown SA, Gibby DL. Is the umbilicus truly midline? Clinical and medicolegal implications. Plast Reconstr Surg. 2003;112(1):259-63.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), preceptor at the Department of Plastic Surgery of the Santa Casa de Porto Alegre - Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil.
2. Plastic surgeon, full member of the SBCP, head of the Department of Plastic Surgery of the Irmandade Santa Casa de Misericórdia de Porto Alegre - UFCSPA, Adjunct Professor of Plastic Surgery at the UFCSPA, Porto Alegre, RS, Brazil.
Correspondence to:
Rafael Netto
Av. Iguaçu, 165 - ap. 304 - Petrópolis
Porto Alegre, RS, Brazil - CEP 90470-430
E-mail: rafael@rafaelnetto.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 26, 2012
Article accepted: July 23, 2012
This study was performed at the Irmandade Santa Casa de Misericórdia de Porto Alegre - Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter