

Original Article - Year 2012 - Volume 27 -
Complications in breast reconstruction using a transverse rectus abdominis myocutaneous flap
Complicações em reconstrução de mama com retalho pediculado do músculo reto abdominal transverso
ABSTRACT
BACKGROUND: Breast cancer is the leading cause of death in the female population. The treatment for breast cancer is primarily surgical, which has a great psychosocial impact on women. To reduce this trauma, reconstructive surgery offers different options including the use of a retail transverse rectus abdominis (TRAM) flap. This is an alternative reconstruction that has been widely used worldwide over the last 30 years. Although reconstruction using the TRAM flap is the most widely used technique that yields the best aesthetic and functional results, it is associated with certain complications. The aim of this study is to present the main complications of reconstruction using the TRAM flap according to its variants (ipsilateral, contralateral, and bilateral) and reconstruction time.
METHODS: We evaluated 30 patients who had a mastectomy and breast reconstruction using the TRAM flap, including 25 immediate reconstructions and 5 late reconstructions, and analyzed the complications of the donor and recipient areas.
RESULTS: Among the identified complications, fat necrosis in the breast was the most frequent, but we also observed cases of infection, seroma, abdominal hernia, skin injury at the donor and recipient areas, and deep vein thrombosis. Complications were more frequent in patients who underwent late reconstruction with a bilateral TRAM flap.
CONCLUSIONS: Thus, similar to other types of surgery, breast reconstruction using the TRAM flap is associated withvarious postoperative complications, even 30 years after it was first introduced.
Keywords: Breast/surgery. Mammaplasty/adverse effects. Reconstructive surgical procedures. Surgical flaps. Abdominal muscles.
RESUMO
INTRODUÇÃO: O câncer de mama é a afecção que mais causa mortes na população feminina. Seu tratamento é principalmente cirúrgico, o que causa grande impacto psicossocial na mulher. Para diminuir esse abalo, a cirurgia reconstrutiva oferece diferentes opções, como o retalho do músculo reto abdominal transverso (TRAM). Essa é uma alternativa de reconstrução que tem sido bastante utilizada nos últimos 30 anos, mundialmente. Embora seja a mais aplicada e a técnica que possibilita melhores resultados estéticos e funcionais, não deixa de apresentar complicações. O objetivo deste estudo é apresentar as principais complicações do TRAM de acordo com suas variantes (ipsilateral, contralateral e bilateral) e com o tempo da reconstrução.
MÉTODO: Foram avaliadas 30 pacientes submetidas a mastectomia e reconstrução mamária com TRAM pediculado, sendo 25 reconstruções imediatas e 5 tardias. Foram analisadas as complicações das áreas doadora e receptora.
RESULTADOS: Dentre as complicações identificadas, a necrose gordurosa na mama foi a mais incidente, mas também foram verificados casos de infecção, seroma, hérnia abdominal, sofrimento da pele em áreas doadora e receptora, e trombose venosa profunda. As complicações foram mais frequentes nas pacientes que realizaram o TRAM bilateral tardiamente.
CONCLUSÕES: Assim como todos os tipos de cirurgia, a reconstrução de mama pelo TRAM, mesmo passados 30 anos desde sua descrição, está sujeita a diversas complicações no pós-operatório.
Palavras-chave: Mama/cirurgia. Mamoplastia/efeitos adversos. Procedimentos cirúrgicos reconstrutivos. Retalhos cirúrgicos. Músculos abdominais.
Breast cancer has the highest prevalence and incidence among malignant tumors in women and is the second most common cancer, excluding non-melanoma skin tumors1. Approximately 1.2 million new cases are diagnosed each year with a 5-year survival of approximately 4.5 million patients and a mortality rate of 15% of all cancer deaths in women, making it the leading cause of death in this group2.
The treatment of breast cancer depends on the tumor type and stage, and surgery remains the main therapeutic option consisting of partial or total resection of one or both breasts.
When treating women with breast cancer, it is the surgeon's responsibility to acquire sufficient skill in the available surgical options, and choose the most appropriate option for each case. There is a trend toward performing conservative rather than radical surgery3. However, total mastectomy remains a widely used technique in clinical practice since it affects patients physically, emotionally, and sexually, as well as negatively impacts their quality of life, occasionally to a greater degree than the actual disease2. To avoid such effects, breast reconstruction has been adopted as an excellent alternative for patients undergoing this surgery. It promotes wellness and reverses many of the psychological and emotional consequences associated with mastectomy. Several reconstructive procedures have been described, including silicone implants, expander implants, latissimus dorsi muscle flap and the associated implants, and rectus abdominis muscle flaps (which have been used for almost 3 decades).
The first version of the vertical rectus abdominis (VRAM) flap for breast reconstruction was reported by Drever4 in 1977. In 1979, Holmström5 was the first to employ the free rectus abdominis musculocutaneous flap for breast reconstruction. In the same year, Robbins6 described this as a pedunculated flap. However, this flap was only popularized in 1982 by Hartrampf et al.7, who first described the use of the pedunculated TRAM flap for breast reconstruction. Since then, the TRAM flap and its different variants - unipediculated, bipediculated, free, and free based on a perforator (DIEP) - have comprised the universal procedure for breast reconstruction, and they are still used in the most advanced centers for treatment and breast reconstruction worldwide8,9. Their advantages are well documented and include excellent results in symmetry, shape, and aesthetic appearance of the reconstructed breast. Although it is a widely accepted procedure, it is not devoid of complications.
According to the literature, complications associated with breast reconstruction after TRAM are grouped into 2 categories: flap complications and donor site complications. Flap complications include partial or total loss of the flaps, both of which are related to vascular problems that possibly arise from excessive muscle devascularization or undue resection of the superior epigastric artery10, fat necrosis, wound dehiscence, or infection. Donor site complications include seroma, hematoma, abdominal hernia, abdominal wall weakness, and wound dehiscence3.
The aim of this study was to analyze the prevalence of complications of TRAM reconstruction in its different variants (ipsilateral, contralateral, and bilateral) according to the time at which the reconstruction was performed (immediate or delayed)11.
METHODS
We retrospectively evaluated 30 patients who underwent breast reconstruction after mastectomy using the TRAM flap, at the Plastic Surgery Service of the Hospital Universitário Walter Cantídio (University Hospital Walter Cantídio) - HUWC, from August 2007 to August 2012.
The patients completed a questionnaire, which recorded information on the type of TRAM flap used, surgical complications, whether hospitalization for the procedure was required, comorbidities, time of completion of reconstruction, and types of adjuvant therapies used (chemotherapy/radiotherapy). Relevant information was complemented by clinical histories of each patient that were compiled from the hospital records.
The data were entered into an Excel spreadsheet and presented as simple frequencies to assess the incidence of complications according to the time of reconstruction (immediate or delayed) and the type of TRAM flap used in the reconstruction.
RESULTS
We interviewed 30 mastectomy patients aged 31-60 years (mean, 44 years and 3 months). The duration of postoperative hospital stay ranged from 1 to 10 days, and the majority (63%) of the patients were hospitalized for 4-7 days. Thirty percent of patients had a duration of hospital stay ranging from 1 to 3 days, whereas it ranged from 8 to 10 days in 7% of patients.
Immediate reconstructions were performed in 83% of cases, whereas delayed reconstructions were performed in 17% of cases. Among the patients, 64% had comorbidities prior to mastectomy, such as cesarean sections (26%), hernia (11%), hypertension (11%), diabetes (4%), hypercholesterolemia (4%), hysterectomy (4%), and obesity (4%).
Complications were observed in 10 (33.3%) patients. Some women had more than one type of complication. The most common complications included fat necrosis of < 10% of the volume of the breast (27%) and skin injury of the receiving area (10%) (Figure 1).

Figure 1 - Major complications that occurred in breast reconstruction with a transverse rectus abdominis myocutaneous flap post-mastectomy from August 2007 to August 2012 at the University Hospital Walter Cantídio.
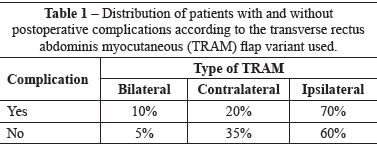
As for the TRAM technique, 19 (63.3%) patients underwent breast reconstruction using an ipsilateral TRAM flap, 9 (30%) underwent breast reconstruction using a contralateral TRAM flap, and 2 (6.7%) underwent breast reconstruction using a bilateral TRAM flap (Figure 2). With regard to the type of TRAM flap used in the patients who had complications, 7 (70%) patients received the ipsilateral variant, 2 (20%) received the contralateral variant, and 1 (10%) received the bilateral variant (Table 1).

Figure 2 - Transverse rectus abdominis myocutaneous flap variants used for breast reconstructions, between August 2007 and August 2012, at the University Hospital Walter Cantídio.
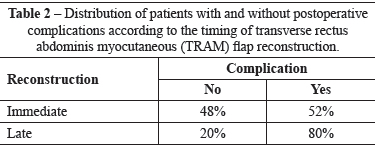
Twenty-five (83.3%) patients underwent immediate reconstruction, whereas 5 (16.7%) underwent late. Among the patients who underwent immediate reconstruction, 13 (52%) had complications; among those who underwent delayed reconstruction, 4 (80%) had complications (Table 2).
DISCUSSION
Breast cancer, which has a high incidence and prevalence worldwide, is responsible for the high number of mastectomies performed. As a result, reconstruction operations are becoming increasingly common. Since it was first described in 1982, the TRAM flap has gained much popularity worldwide and quickly became the preferred method for breast reconstruction using autologous tissue7.
It is of paramount importance to first assess the steps involved in the technique for breast reconstruction since mastectomy can influence cancer treatment as well as the clinical outcome of patients.
Breast reconstruction has assumed an increasingly central role in the treatment of breast cancer due to its proven psychoemotional benefits for patients. The increased demand for breast reconstruction is accompanied by a high demand for reducing psychological damage and functional limitations resulting from oncologic and surgical mutilation12,13. It is critical to carefully consider the indications and contraindications for the use of the TRAM flap, which is immensely popular and is widely used in several reconstructions, particularly in breast reconstruction post-mastectomy13,14. The TRAM flap is based on the superior epigastric vessels. A muscle section technique is used to remove the flap, which reduces the incidence of deformity contours of the abdomen and allows for a safer and immediate abdominal closure15.
Although the TRAM flap is the most commonly used technique, complications are still observed, even when it is performed by experienced surgeons. This present study indicated that the incidence of fat necrosis in the flap was high (27%), which is similar to American studies reporting that 26.9% of cases of fat necrosis are clinically detectable. More serious flap complications, such as total flap loss, were not reported in this article. With regard to skin injury and partial necrosis, these complications occurred in a small number of patients and were generally resolved through conservative measures. Partial necrosis of the skin of the receiving area (10%) may be related to extensive resection of the subcutaneous tissue that nourishes the skin as well as excessive tension at the time of new breast creation. With regard to complications that affected the donor area, the rates observed in the present study were comparable to those of other studies, and most were associated with abdominal pain and partial necrosis. It should be noted that such complications occurred mainly in the navel and in the middle of the abdominal wound, indicating that this may be due to the increased tension in the area as well as poor blood supply to that area.
Different TRAM flap variants, including bipediculated, ipsilateral, contralateral, and bilateral, have been used in breast reconstruction, and the related complications are not representative of a specific technique. Complications of late reconstruction are similar. Several factors may be associated with complications of reconstruction, such as diabetes, obesity, and tobacco use.
CONCLUSIONS
Similar to other types of surgery, breast reconstruction using the TRAM flap, even 30 years since it was first introduced, is associated with various postoperative complications. Fat necrosis in < 10% of the breast volume was the most commonly observed complication, followed by skin injuries to the donor and recipient areas and abdominal wall hernia. These complications have no direct relation to the type of TRAM flap used or the time of reconstruction.
REFERENCES
1. Tournieux TT. Fatores preditivos para um bom resultado estético em cirurgias conservadoras por câncer de mama. Rev Bras Cir Plást. 2012;27(1):37-48.
2. Ibañez GR, Ibañez MR, Pereira NC, Mandiola CB, Andino RN. Comparación de los efectos de la radioterapia sobre los resultados estéticos y complicaciones en reconstrucciones mamarias inmediatas versus diferidas con TRAM pediculado. Rev Hosp Clín Univ Chile. 2011;22(3):187-94.
3. Regueira FM, Rodríguez-Spiteri N, García Manero M, Zornoza G. Novedades en el tratamiento quirúrgico del cáncer de mama. Rev Med Univ Navarra. 2008;52(1):51-5.
4. Drever JM. The epigastric island flap. Plast Reconstr Surg. 1977;59(3):343-6.
5. Holmström H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13(3):423-7.
6. Robbins TH. Rectus abdominis myocutaneous flap for breast reconstruction. Aust N Z J Surg. 1979;49(5):527-30.
7. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69(2):216-25.
8. Lozano JA, Roldán P, Escudero FJ. Reconstrucción mamaria con el colgajo musculocutáneo recto abdominal transverso (TRAM). Anales Sis San Navarra. 2005;28 Suppl. 2:63-71.
9. Giachero-Castaño V, Jacobo-Bastreri O, Grattarola-Rizzo G, Carriquiry-Kayel C. Reconstrucción mamaria con colgajo músculo-cutáneo transverso de recto abdominal (TRAM) y simetrización simultânea. Cir Plást Iberolatinoam. 2010;36(2):135-44.
10. Chveid M. Análise crítica do arco de rotação e posicionamento estético funcional do TRAM-flap nas reconstruções mamárias. Rev Soc Bras Cir Plást. 1997;12(2):15-26.
11. Oliveira Junior FC, Mélega JM, Pinheiro AS, Pereira RF. Reconstrução mamária total: técnicas e complicações. Rev Bras Cir Plást. 2010;25 Supl:62.
12. Atisha D, Alderman AK. A systematic review of abdominal wall function following abdominal flaps for postmastectomy breast reconstruction. Ann Plast Surg. 2009;63(2):222-30.
13. Rietjens M, Urban CA, De Lorenzi F, Bonato Jr A. Reconstrução mamária com retalho miocutâneo do músculo reto abdominal (TRAM). In: Mélega JM, Montoro AF, Albertoni WM, eds. Cirurgia plástica: fundamentos e arte. Cirurgia reparadora de tronco e membros. Rio de Janeiro: MEDSI; 2004. p.92-6.
14. Wilkins EG, August DA, Kuzon WM Jr, Chang AE, Smith DJ. Immediate transverse rectus abdominis musculocutaneous flap reconstruction after mastectomy. J Am Coll Surg. 1995;180(2):177-83.
15. Namnoum JD. An analysis of 920 pedicled and 286 free TRAM flap breast reconstructions. Annual Meeting of the American Society of Plastic Surgeons. Orlando, FL: November 2001.
1. Foreign Student in the Program of Residency in Plastic Surgery and Reconstructive Microsurgery, Hospital Universitário Walter Cantídio da Universidade Federal do Ceará (University Hospital Walter Cantídio Federal University of Ceará - UFC), Fortaleza, CE, Brazil.
2. Plastic Surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery), Regent of the Department of Plastic Surgery and Reconstructive Microsurgery, Hospital Universitário Walter Cantídio (University Hospital Walter Cantídio) - UFC, Fortaleza, CE, Brazil.
3. Medical Student in the UFC, Member of the League of Plastic Surgery, UFC, Fortaleza, CE, Brazil.
Correspondence to:
Carolina Garzon Paredes
Rua Abolição, 2111 - ap. 1802 - Meireles
Fortaleza, CE, Brasil - CEP 333323-432
E-mail: caritog76@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: September 25, 2012
Article accepted: November 24, 2012
This study was performed at the Hospital Universitário Walter Cantídio da Universidade Federal do Ceará (University Hospital Walter Cantídio Federal University of Ceará), Fortaleza, CE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter