

Ideas and Innovation - Year 2012 - Volume 27 -
Dermal barrier for immediate prosthetic breast reconstruction
Barreira cutânea para reconstrução mamária com prótese
ABSTRACT
BACKGROUND: Immediate breast reconstruction with silicone implant after subcutaneous mastectomy became a valid option among doctors and patients based on the simplicity of the surgical maneuvers, shorter surgical period, minimal scarring and immediate aesthetic results. Submuscular implants also have been advocated despite its more aggressive surgical procedures. Both also may bring secondary already described diversification's problems. An in attempt to reduce this kind of problems, in this article, a modification of the circumvertical mastopexy, reduction mammoplasty pattern for mastectomy and immediate breast implant reconstruction is described.
METHODS: The skin between the medial and lateral vertical skin incision lines is de-epithelialized, providing a dermal barrier over the prosthesis to reinforce the vertical suture line.
CONCLUSIONS: The technique ensures a safe reconstruction with gratifying aesthetic results.
Keywords: Mammaplasty/methods. Breast/surgery. Breast implantation/methods. Breast neoplasms/surgery. Mastectomy/methods.
RESUMO
INTRODUÇÃO: A reconstrução mamária imediata com implante de silicone após mastectomia subcutânea tornou-se uma opção válida para médicos e pacientes devido à simplicidade das manobras cirúrgicas, menor tempo cirúrgico, cicatriz mínima e resultados estéticos imediatos. Os implantes submusculares também são recomendados, apesar de exigirem um procedimento cirúrgico mais agressivo. Ambos também podem causar problemas secundários que já foram descritos. Para reduzir esse tipo de problemas, neste artigo é descrita uma modificação da mastopexia circunvertical, redução do padrão de mamoplastia para mastectomia e a reconstrução mamária imediata com implante.
MÉTODO: A pele entre as linhas de incisão cutânea medial e vertical lateral é desepitelizada, criando uma barreira cutânea para a prótese para reforçar a linha de sutura vertical.
CONCLUSÕES: A técnica garante uma reconstrução segura, com resultados estéticos gratificantes.
Palavras-chave: Mamoplastia/métodos. Mama/cirurgia. Implante mamário/métodos. Neoplasias da mama/cirurgia. Mastectomia/métodos.
Techniques for post mastectomy breast reconstruction are diverse and may involve complex free tissue transfers, flaps, fat grafting or insertion of prosthetic implants and expanders. As mastectomy techniques are evolving from radical excisions to skin sparing mastectomies, immediate reconstruction of the breast with an implant is becoming a valid preferred option by many patients because of its simplicity, shorter total operative time, minimal scarring and the immediate aesthetic result it provides. It allows immediate restoration of body figure avoiding psychologically traumatic mutilation even if temporary1-3.
Though enough skin may be available with skin sparing mastectomy, there is however a risk of vascular compromise of long thin skin flaps with subsequent wound dehiscence, implant exposure and extrusion. Total muscle coverage of the implant by the pectoralis major muscle, the serratus anterior muscle, and the fascia of the anterior rectus has been advocated to prevent implant loss. This is however practically impossible to achieve with large implants.
However, as advocated by many over so many years, is total muscle coverage of the implant really necessary? In fact it is essential to separate the implant from the incision line in order to avoid extrusion of the prosthesis should skin edge necrosis and wound dehiscence occur. As such, muscle coverage is a specific mean designed for a specific goal, it is not a goal by itself. Unfortunately, over the years, total muscle coverage seemed to become the major goal in alloplastic breast reconstruction greatly limiting the applicability and outcome of this reconstruction modality. Invariably, total muscle coverage restricts the size of implants that can be inserted. It results also in high-riding breast mound with blunting of the inframammary and lateral mammary folds due to compression of the lower and lateral aspects of the implant1,4. With anatomically shaped implants, the inferior tethering of the submuscular pocket may also prevent these contoured devices from maximally expressing their shapes, leading to a rounded, high-riding breast, with upper-pole fullness5.
For superior aesthetic outcomes regarding lower pole fullness and some degree of ptosis, subcutaneous placement of the implant is preferable1. It is evident at present that the dual dermomuscular pouch, upper submuscular and lower subcutaneous, provides better cosmetic appearance with appropriate distribution of volume between superior and inferior as well as medial and lateral aspects of the breast3,6.
Improved cosmetic appearance may also be attained with the use of skin incision patterns of aesthetic breast procedures for mastectomy particularly when some skin reduction is required. The scars of the reconstructed breast may also be matched to the contralateral mastopexy or reduction mammoplasty whenever indicated.
When no skin reduction is required, a horizontal elliptical excisional pattern will invariably result in vertical skin shortening causing gross asymmetry with the contralateral breast. A vertical pattern on the other hand, will maintain vertical height of the reconstructed breast and helps to narrow the breast base producing a more pleasant rounded lower reconstructed breast pole in contradistinction to the square and flat appearance often observed when alloplastic breast reconstruction is performed with a transverse mastectomy scar particularly when the breast originally is large and ptotic7.
Carlson et al.8 has proposed a classification of four skin pattern types for skin sparing and skin reducing mastectomy. The skin reducing mastectomy, however, has been restricted to the Wise inverted T pattern. Subsequently a fifth type was described by Santanelli et al.9 as a modification to allow skin excision outside the confines of the standard Wise pattern when mandated by oncological considerations. These five described skin incision types, however, do not account for the horizontal elliptical excision most widely performed by general surgeons that allows development of short flaps as well as the increasingly popular vertical scar pattern. We have proposed a new more inclusive classification clearly distinguishing skin sparing from skin reducing mastectomies2.
Skin flap necrosis and T-junction breakdown is the Achilles'heeloftheWise pattern. When it occurs in conjunction of alloplastic breast reconstruction, it results in implant extrusion and reconstruction failure. Many authors have reported various modifications to reinforce the vertical infra-areolar suture line with a de-epithelialized dermal flap, increasing implant protection, and preventing its exposure and extrusion5,8,10,11. An allogenic dermal graft sling to supplement the muscle deficit at the lower breast pole has also been described and is reported to provide safe and aesthetically pleasing reconstruction. It reported also to reduce the incidence of late capsular contractures3,4,12-14.
We describe a modification of the circumvertical mastopexy/reduction mammoplasty pattern15,16 for mastectomy and immediate implant breast reconstruction. The skin between the medial and lateral vertical skin incision lines is de-epithelialized providing a dermal barrier to reinforce the vertical suture line. The technique ensures a safe reconstruction with gratifying aesthetic results.
METHODS
Preoperative planning of the circumvertical incisions is performed in consultation with the oncologic surgeon and drawings are made with the patient in the standing position. Modifications of the standard design are made according to oncologic considerations. For skin sparing mastectomy a limited area of de-epithelialization is marked below the nipple areola complex between the two vertical incisions. In large ptotic breasts a larger infra areolar area of de-epithelialization may be outlined and the limits of skin excision above the nipple areola complex are marked to achieve reduction and elevation as much as needed. It must be noted though that supra areolar skin excision should be very conservative not as much as for a standard reduction mammoplasty or mastopexy since the superior skin flap will eventually retract. For moderate elevation, only the areolar skin is excised. Whenever the nipple areola complex is to be saved such as for prophylactic mastectomy, it may be kept attached to the dermal barrier flap and transposed to its superior location or it may be transposed as a free nipple areola graft.
The dermal barrier flap can be based either medially or laterally. A medially based dermal barrier flap is preferable in most cases hence mastectomy is performed through the determined circumareolar incision line with a downward vertical extension laterally stopping 1-2 cm above the inferior border of the vertical design pattern. This incision provides adequate exposure for mastectomy. A separate axillary incision is made for sentinel lymph node biopsy or eventually axillary lymphadenectomy.
After completing the mastectomy, a subpectoralis major pocket is created by completely dis-inserting the muscle inferiorly. Limited medial muscle fibers release is also required making sure not to extend the release superiorly beyond the level of the projected nipple location. It is important also to preserve a soft tissue layer between the detached medial edge of the muscle and its original sternal attachment to avoid unsightly depression in the medial inferior border of the reconstructed breast postoperatively.
The inframammary fold is then repositioned at a higher level as needed to match the contralateral mastopxy that can often be performed at the same setting. The pectoralis muscle and the dermal barrier flap are then sutured together to form a dual plane pocket capable of accommodating a large implant. The lateral skin flap is subsequently advanced over the dermal barrier and secure closure of the vertical incision is performed (Figures 1 and 2). Superiorly, the circumareolar component of the incision may be closed by a purse string suture rather than linearly to reduce scar length. Modifications of this standard design and technique are possible as dictated by oncologic considerations. In most patients, Mentor© (Irving, TX, USA) textured anatomical cohesive gel implants were used. Rarely, Mentor© Becker tear drop implants were used in cases where there was some concern about excessive tension due to wider skin excision.
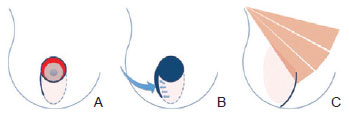
Figure 1 - Diagrammatic representation of the circumvertical skin sparing mastectomy with dermal barrier flap for immediate breast reconstruction. In A, circumvertical design: circumareolar and lateral vertical infra areolar incision lines; skin excision is limited to the circumareolar area. In B, completed mastectomy and de-epithelialized infra-areolar dermal barrier flap to be advanced under the lateral skin flap. In C, dermal barrier flap anchored to the infero-lateral aspect of the pectoralis major muscle and linear vertical suture line.
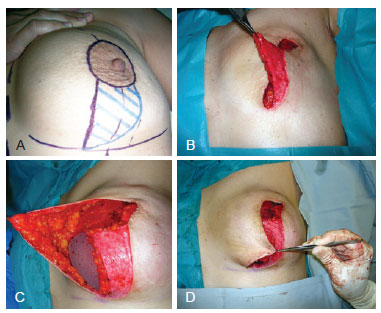
Figure 2 - In A, circumvertical design. In B, dermal barrier flap. In C, lateral advancement of the dermal barrier flap which is sutured to the pectoralis major muscle. In D, vest-over-pant advancement of the lateral skin flap.
DISCUSSION
Mastectomy with vertical excision using the Lejour pattern has already been described. It was stated however that the technique is suitable only for autogenous tissue reconstruction since any wound dehiscence or compromise of skin viability would result in exposure of the alloplastic implant17,18. With the proposed circumvertical pattern and dermal barrier flap the vertical suture line is reinforced making immediate prosthetic breast reconstruction following skin sparing or reducing mastectomy a valid and safe option. Since incisions are limited without any transverse infra-mammary fold component, short skin flaps with wide bases are developed and their vascularity is better preserved. Total muscle coverage of the implant with this technique is not necessary.
Moreover, a medially based dermal flap would tether the breast implant in position and prevent it from slipping into the large lateral pocket invariably created following mastectomy. Hence no additional measures such as obliterating the lateral space with sutures or elevating a serratus muscle flap would be necessary. Even when quilting sutures are adequately placed with the arm normally abducted on the operating table to form the lateral breast fold, great tissue mobility in this area may result in permanent skin dimpling when the arm is adducted. The serratus muscle flap on the other hand, invariably results in some blunting of the lateral breast fold. By just maintaining the implant in proper position and applying continuous negative pressure drainage for at least 10 days a more natural lateral breast fold is created.
Separating the implant from the suture line is all what is needed. This can certainly be achieved with an expensive allogenic dermal sling at the cost of a slight risk of additional complications such as infection or insufficient biocompatibility19; however, this is probably not a logical proposition in view of the available autogenic dermis that may be advantageously used as a free graft or preferably as a vascularized flap.
Dermal flaps associated with a wise pattern already described in the literature are for some of doubtful vascularity. The proposed circumvertical design allows elevations of a well vascularized dermal barrier that can be tailored as needed and even split into medial and lateral flaps transposed as a Z-plasty to provide additional inferior pole length as shown in Figure 3. Moreover, proposed skin markings may be adapted very easily to required oncologic considerations as shown in Figures 4 and 5. However, because of the unfamiliar orientation of the incisions, mastectomy with this approach might initially be technically more challenging for the breast oncologic surgeon. Figures 6 and 7 illustrate the maintenance of long-term results.
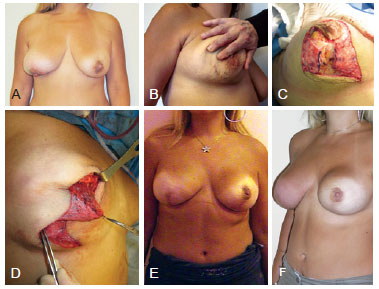
Figure 3 - In A, patient presenting for bilateral mastectomy with previous left partial mastectomy and radiotherapy and recent right inferior quadrant partial mastectomy causing gross deformity. In B, scar of right partial mastectomy greatly limiting the infra-areolar vertical incisions. In C, dermal barrier flap split vertically into medial and lateral flaps. In D, Z-plasty advancement of the 2 dermal barrier flaps. In E, result at 6 months of right breast reconstruction and left breast reconstruction with nipple-areola preservation and circumvertical dermal barrier technique despite previous radiotherapy. In F, result at 1 year.
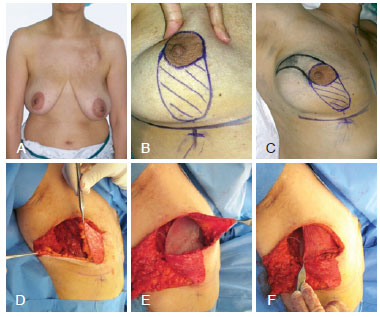
Figure 4 - In A, patient presenting for right mastectomy and immediate alloplastic reconstruction. In B, drawing of circumvertical design. In C, supero-lateral extension of skin excision mandated by oncologic considerations. In D, dermal barrier flap. In E, lateral advancement of the dermal barrier flap. Reconstruction with a Becker permanent expander because of planned post-operative radiotherapy. In F, implant covered superiorly by the pectoralis major muscle.
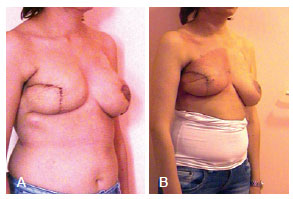
Figure 5 - In A, immediate post-operative result. Expander was fully inflated intra-operatively and contralateral mastopexy was performed simultaneously with the mastectomy and reconstruction. In B, result after completion of radiotherapy.
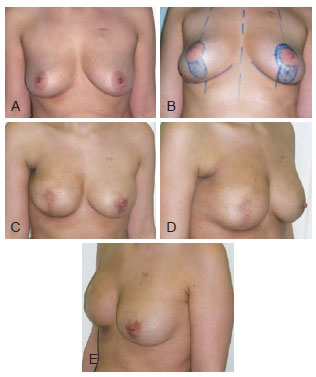
Figure 6 - In A, patient presenting for right skin sparing mastectomy and axillary lymph node dissection and left prophylactic mastectomy. In B, planning for bilateral circumvetical incisions and dermal barrier flap with nipple areola preservation on the left. In C, D, and E, reconstruction results at 1 ½ year. Contour deformity of the anterior axillary fold and minor deformity in projection could be corrected with fat grafting, however the patient was satisfied by the result and refused any further procedures.

Figure 7 - 1 year post-operative result of right skin reducing mastectomy and alloplastic reconstruction with simultaneous contralateral circumvertical mastopexy. Purse string closure of the upper incision shortens scar length and simulates a nipple. The patient refused reconstruction of the areola by tattooing.
CONCLUSIONS
Close collaboration between the oncologic and the reconstructive surgeons is required for proper planning of the skin incisions to optimize the disease treatment while considering the reconstructive needs14. Contrary to what has been originally recommended for post-mastectomy immediate alloplastic breast reconstruction full muscle coverage of the breast implant is not required and probably may be contraindicated. Muscle coverage by itself should not be the primary goal of the reconstruction. It is only a mean, among others, to provide secure skin closure and prevent implant extrusion. Circumvertical excisional pattern with a dermal barrier flap and a vest-over-pant closure of the vertical suture line is probably a better alternative as it provides the necessary safety for alloplastic breast reconstruction and results in an aesthetically pleasing and well balanced breast shape. Naturally, the problem of late capsular contracture following alloplastic breast reconstruction remains a potential issue. The need for post-operative radiotherapy is another issue. Many questions still need to be answered, however any proper oncologic procedure should be discussed within the context of the patient's reconstructive potential with procedures tailored to the needs and wishes of each patient20.
REFERENCES
1. Li FC, Jiang HC, Li J. Immediate breast reconstruction with implants after skin-sparing mastectomy: a report of 96 cases. Aesthetic Plast Surg. 2010;34(6):705-10.
2. Ibrahim AE, Atiyeh BS, Dibo SA, Sarhane KA, Abbas JS. De-epithelialized dermal barrier for a safe immediate prosthetic breast reconstruction post circumvertical skin sparing/reducing mastectomy (SSM/SRM). Eur J Plast Surg. 2012 (in press).
3. Colizzi L, Agostini T, Pascone C, Gandini D, Pantaloni M, Lazzeri D. A dermomuscular pocket provides superior coverage of the implant in skin-reducing mastectomies. Aesthetic Plast Surg. 2010;34(5):675-7.
4. Nahabedian MY. Mastectomy, nipple-areola preservation, and immediate implant reconstruction: are total and partial muscle coverage techniques aesthetically equivalent? Plast Reconstr Surg. 2010;126(6):319e-20e.
5. Hammond DC, Capraro PA, Ozolins EB, Arnold JF. Use of a skinsparing reduction pattern to create a combination skin-muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg. 2002;110(1):206-11.
6. Nava MB, Cortinovis U, Ottolenghi J, Riggio E, Pennati A, Catanuto G, et al. Skin-reducing mastectomy. Plast Reconstr Surg. 2006;118(3):603-10.
7. Losken A, Collins BA, Carlson GW. Dual-plane prosthetic reconstruction using the modified wise pattern mastectomy and fasciocutaneous flap in women with macromastia. Plast Reconstr Surg. 2010;126(3):731-8.
8. Carlson GW, Bostwick J 3rd, Styblo TM, Moore B, Bried JT, Murray DR, et al. Skin-sparing mastectomy. Oncologic and reconstructive considerations. Ann Surg. 1997;225(5):570-5.
9. Santanelli F, Longo B, Sorotos M, Farcomeni A, Paolini G. Flap survival of skin-sparing mastectomy type IV: a retrospective cohort study of 75 consecutive cases. Ann Surg Oncol. 2012. [Epub ahead of print]
10. Skoll PJ, Hudson DA. Skin-sparing mastectomy using a modified Wise pattern. Plast Reconstr Surg. 2002;110(1):214-7.
11. Bayram Y, Kulahci Y, Irgil C, Calikapan M, Noyan N. Skin-reducing subcutaneous mastectomy using a dermal barrier flap and immediate breast reconstruction with an implant: a new surgical design for reconstruction of early-stage breast cancer. Aesthetic Plast Surg. 2010;34(1):71-7.
12. Baxter RA. Intracapsular allogenic dermal grafts for breast implant-related problems. Plast Reconstr Surg. 2003;112(6):1692-6.
13. Breuing KH, Colwell AS. Inferolateral AlloDerm hammock for implant coverage in breast reconstruction. Ann Plast Surg. 2007;59(3):250-5.
14. Salgarello M, Barone-Adesi L, Terribile D, Masetti R. Update on onestage immediate breast reconstruction with definitive prosthesis after sparing mastectomies. Breast. 2011;20(1):7-14.
15. Atiyeh BS, Rubeiz MT, Hayek SN. Refinements of vertical scar mammaplasty: circumvertical skin excision design with limited inferior pole subdermal undermining and liposculpture of the inframammary crease. Aesthetic Plast Surg. 2005;29(6):519-31.
16. Gulyás G. Combination of the vertical and periareolar mammaplasty. Aesthetic Plast Surg. 1996;20(5):369-75.
17. Hunter JE, Malata CM. Refinements of the LeJour vertical mammaplasty skin pattern for skin-sparing mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2007;60(5):471-81.
18. Malata CM, Hodgson EL, Chikwe J, Canal AC, Purushotham AD. An application of the LeJour vertical mammaplasty pattern for skin-sparing mastectomy: a preliminary report. Ann Plast Surg. 2003;51(4):345-50.
19. Mestak J, Sukop A, Mestak O. Use of deepithelialized flap in mammoplasties: simple method with excellent results. Aesthetic Plast Surg. 2011;35(6):1106-11.
20. Toth BA, Forley BG, Calabria R. Retrospective study of the skin-sparing mastectomy in breast reconstruction. Plast Reconstr Surg. 1999;104(1):77-84.
1. Plastic surgeon, professor at Department of Surgery, Division of Plastic, Reconstructive and Aesthetic Surgery, American University of Beirut Medical Center, Beirut, Lebanon.
2. General surgeon, professor at Department of Surgery, Division of General Surgery, American University of Beirut Medical Center, Beirut, Lebanon.
3. Plastic surgeon, professor at Plastic, Reconstructive and Aesthetic Surgery, Toulouse University, Toulouse, France.
Correspondence to:
Bishara S. Atiyeh
American University of Beirut Medical Center Cairo Street - Marignan Center - 6th floor
Beirut, Lebanon
E-mail: batyieh@terra.net.l.lb
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: September 27, 2012
Article accepted: October 29, 2012
This study was performed at American University of Beirut Medical Center, Beirut, Lebanon.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter