

Original Article - Year 2012 - Volume 27 -
The presence of low intraoral pressure in speech following surgical correction of cleft palate
Fraca pressão aérea intraoral na fala após correção cirúrgica da fissura palatina
ABSTRACT
BACKGROUND: Several anatomical and functional changes are observed in individuals with cleft lip and palate, including structural abnormalities of the oropharyngeal muscles, which can cause loss of velopharyngeal function and other functions such as sucking, swallowing, and speaking. The present study aimed to evaluate the presence of weak intraoral air pressure in the speech of individuals with cleft palate who underwent primary palatoplasty at the appropriate time or at a late stage and assess whether surgical timing may lead to a higher occurrence of the disorder. We hypothesized that individuals who undergo belated primary palatoplasty show a higher occurrence of weak intraoral air pressure compared to those who undergo primary palatoplasty at the appropriate time.
METHODS: This study included 37 patients of both sexes with a diagnosis of cleft palate, with or without cleft lip, who were divided into 2 groups: 1) early group (GP), consisting of 22 patients who underwent primary palatoplasty during the second year of life, and 2) the late group (GT), comprising 15 patients who underwent primary palatoplasty at a later stage, after acquiring speech sounds. All participants underwent routine clinical assessment with an interval of at least 3 months after surgery. Among the parameters evaluated, weak intraoral air pressure was an important variable considered in this study.
RESULTS: Data analysis revealed a higher frequency of weak intraoral air pressure in the GT group (33%) as compared to the GP group (18%). However, this difference was not statistically significant (P = 0.44).
CONCLUSIONS: The study hypothesis was rejected. The presence of weak intraoral air pressure was observed in the speech of both groups, and the study findings showed that the timing at which primary palatoplasty was performed is not an influencing factor.
Keywords: Cleft palate. Velopharyngeal insufficiency. Speech.
RESUMO
INTRODUÇÃO: Diversas alterações anatômicas e funcionais são observadas nos indivíduos portadores de fissuras labiopalatinas, dentre elas anormalidades estruturais da musculatura orofaríngea, que podem causar prejuízo da função velofaríngea e, consequentemente, de funções como sucção, deglutição e fala. O presente estudo teve por objetivo avaliar a presença de fraca pressão aérea intraoral na fala de indivíduos com fissura palatina submetidos a palatoplastia primária em tempo adequado e tardiamente, e comparar se o momento do procedimento cirúrgico pode acarretar maior ocorrência do distúrbio. A hipótese é de que os indivíduos submetidos a palatoplastia primária tardiamente apresentam maior ocorrência de fraca pressão aérea intraoral em comparação àqueles que realizaram a palatoplastia primária no momento adequado.
MÉTODO: Participaram do estudo 37 indivíduos de ambos os sexos, com diagnóstico de fissura de palato associada ou não à fissura de lábio, divididos em dois grupos: 1) grupo precoce (GP), composto por 22 pacientes submetidos a palatoplastia primária até o 2º ano de vida; e 2) grupo tardio (GT), composto por 15 pacientes submetidos a palatoplastia primária tardiamente, após o período de aquisição dos sons da fala. Todos os participantes foram submetidos a rotina de avaliação fonoaudiológica com intervalo de, no mínimo, 3 meses de pós-operatório. Dentre os parâmetros avaliados encontra-se a análise da fraca pressão aérea intraoral, que foi a variável considerada para este estudo.
RESULTADOS: A análise dos dados possibilitou observar maior frequência de fraca pressão aérea intraoral no GT (33%) em comparação ao GP (18%). Entretanto, tal diferença não foi estatisticamente significante (P = 0,44).
CONCLUSÕES: A hipótese do estudo foi rejeitada. A presença de fraca pressão aérea intraoral foi observada na fala dos dois grupos estudados, não sendo a idade na ocasião da palatoplastia primária um fator determinante.
Palavras-chave: Fissura palatina. Insuficiência velofaríngea. Fala.
Cleft lip and palate represent the most common congenital face anomalies affecting the lip and/or palate and can occur in isolation or in association with other complex malformations. Congenital anomalies are frequently treated in craniofacial surgery centers, and area associated with an incidence of 1 in every 600 live newborns1. These anomalies are caused by the failure of fusion between the maxillary processes and the mid-nasal area due to genetic and environmental factors, which prevents the complete growth of these structures, thus causing developmental difficulties2.
Several anatomical and functional changes are observed in individuals with cleft lip and palate, including structural abnormalities of the oropharyngeal muscles, which can cause loss of velopharyngeal function as well other functions such as sucking, swallowing, and spaking3. Due to this wide range of changes, a multidisciplinary approach is necessary from birth to the onset of adulthood4.
In the literature, it has become well established that the surgical repair of cleft palate should be performed early, before the patient is 2 years of age5,6. Surgical treatment aims to restore adequate velopharyngeal function, which is essential in early childhood7. Thus, different palatoplasty techniques have been developed to achieve an adequate length of palate to allow for touching of the posterior pharyngeal wall. Another aspect that is addressed involves reorientation of the muscle fibers of the palate, which creates a muscular belt that will allow better mobility of the soft palate6,8.
However, despite progress in the area, it remains difficult to predict the efficiency of muscle function after palate surgery7. Although the effort to establish adequate velopharyngeal function is paramount to the primary surgical repair of the palate, according to the literature, up to 35% of individuals who have undergone correction for cleft palate still have velopharyngeal insufficiency. This may be due to inadequate dissection of the palatal muscles, insufficient palatal length, or even anatomical alterations of the posterior pharyngeal wall. In such cases, palatoplasty can yield an adequate soft palate with posterior elevation; however, adequate velopharyngeal closure would be compromised by anatomical pharyngeal variation9.
Failure of velopharyngeal closure results in loss of the part of the airstream into the nasal cavity that is responsible for speech, leading to the appearance of symptoms that can directly or indirectly impair speech intelligibility10-12. Hypernasality, nasal air emission (audible or not), and weak intraoral air pressure are considered direct consequences7,10,11. Velopharyngeal insufficiency may also lead to the development of compensatory articulation strategies used by an individual to compensate for the inability to exert oral cavity pressure in other parts of the vocal tract10-12.
Hypernasality, the most characteristic symptom of velopharyngeal insufficiency, corresponds to excessive nasal resonance during the production of oral sounds in speech2,7,10. The nasal air emission arises from exhaust airflow into the nasal cavity during speech production, which can be presented audibly or non-audibly, the former being more detrimental to speech intelligibility since it may be perceived by the listener2,7,10,12,13.
The maintenance of expiratory flow and changes in resistance along the vocal tract result in adequate levels of intraoral air pressure during the production of consonant sounds14,15. Weak intraoral air pressure reduces the air pressure maintained in the oral cavity that ensures the proper production of oral speech sounds, thereby reducing the traces of the phoneme discrimination and impairing speech intelligibility. In response to inadequate intraoral air pressure to produce speech, the individual often develops compensatory articulation disorders7,10,11.
Besides allowing for the correct articulation of speech sounds, the adequacy of velopharyngeal function is also crucial for the balance of other oral functions such as suction and swallowing2,8. Therefore, it is necessary that the soft palate and the lateral and posterior pharyngeal walls undertake a broad and synchronized movement that allows for the maintenance of contact between these structures and ensures total separation between the oral and nasal cavities8,13.
This study aimed to evaluate the presence of weak intraoral air pressure in the speech of individuals with cleft palate who underwent primary palatoplasty, either timely or belatedly, and investigate whether the surgical timing may lead to a higher occurrence of the disorder. The hypothesis is that individuals who undergo late primary palatoplasty show a higher occurrence of weak intraoral air pressure compared to those who undergo timely primary palatoplasty.
METHODS
The procedures for participant selection and evaluation began only after approval from the ethics committee was obtained (CAPPesq HCFMUSP 0455/08) and each patient provided written informed consent.
The study included 37 male and female patients with cleft palate with or without cleft lip diagnosed by medical personnel of the Group of Craniomaxillofacial Surgery, Division of Plastic Surgery and Burns of the Hospital das Clinicas, Faculty of Medicine, University of São Paulo (HC-FMUSP) as routine examinations. This sample was divided into 2 groups: early (GP) and late (GT).
The GP group was composed of 22 patients who underwent primary palatoplasty until the second year of life. The GT was composed of 15 patients who underwent late palatoplasty after 2 years of age.
Inclusion Criteria
The study included individuals of any age and sex who were diagnosed with cleft palate with or without cleft lip that was surgically corrected at least 3 months before the screening date.
Exclusion Criteria
Exclusion criteria included the presence of palatal fistula (regardless of size and location), neurological disorders, history of facial trauma and respiratory diseases, and prior speech therapy; patients who underwent secondary palatoplasty to ensure adequacy of velopharyngeal function were also excluded.
All participants underwent routine clinical assessment at the Clinic of Facial Functions in Cleft Palate Support Unit of the Central Institute of Speech HC-FMUSP. All assessments were performed by trained and experienced audiologists.
Data collection for this study was based on routine assessments, specifically the perceptual evaluation of speech. The protocol of our own unit was used. The protocol consisted of the analysis of speech samples composed of excerpts from directed speech (repetition of words and phrases) with recurrence of the target sound to be analyzed containing all the phonemes of Brazilian Portuguese, automatic speech during counting 1 from 10, and spontaneous speech in which the patient was asked to narrate a daily occurrence.
The analysis of weak intraoral air pressure, a variable considered in this study, was among the parameters evaluated by this protocol. This feature was classified as "present" or "absent" in the different speech samples. Weak intraoral air pressure was defined as the presence of a modification while issuing at least one phoneme for each of the samples.
To analyze the results, we used Fisher's exact test with a significance level of P < 0.05.
RESULTS
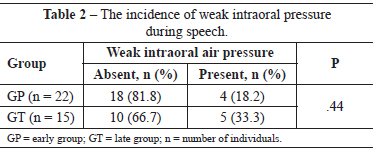
The general characterization of groups in terms of age, sex, and cleft type is shown in Table 1.
With regard to gender, the individuals were not distributed similarly in both groups. The GP group members were mostly males, whereas those in the GT group were mostly females. Regarding cleft type, there were also differences between groups; a cleft lip and palate were more common among younger individuals and a cleft palate only was more common among adults.
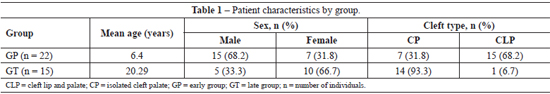
The postoperative outcomes related to the occurrence of low intraoral air pressure are shown in Table 2.
A higher incidence of weak intraoral air pressure was observed in individuals of the GT group; however, this difference was not statistically significant (P = 0.44).
DISCUSSION
In Brazil, as in other developing countries, it is not always possible to follow the cleft lip and palate treatment steps proposed by international protocols. Factors such as socioeconomic status, lack of guidance/information, and the absence of specialized centers hamper appropriate treatment. We also observed that individuals seek treatment after the period of acquisition of oral language, often once the individual has already reached adulthood.
According to the literature, primary palatoplasty should be performed early, preferably before 2 years of age5,6. Closure of the mucosa together with the repositioning of the levator muscle of the velum aims to promote adequate velopharyngeal closure, which leads to the complete separation of the oral and nasal cavities during oral functions (speaking, chewing, and swallowing)2,16-18.
Adequate velopharyngeal function is essential for the acquisition of speech sounds without the development of direct or indirect disorders. Direct disorders, including hypernasality, nasal air emission, and weak intraoral air pressure, alone or combined, result in the loss of speech intelligibility to various degrees7,11. Velopharyngeal insufficiency can indirectly lead to the development of compensatory articulation to compensate for an individual's inability to generate air pressure in the oral cavity7,10,13.
Intraoral air pressure can be subjectively evaluated by audio analysis performed by an experienced professional or even using tools such as the pressure-flow technique, by raising blood pressure values and oral and nasal air flow19.
With regard to the presence of weak intraoral air pressure, no significant differences were found between subjects who underwent palatoplasty at an early or late stage. In an earlier study, researchers evaluated the intraoral air pressure after palatoplasty in 2 groups of patients with and without signs of velopharyngeal insufficiency using instrumental assessment and found reduced pressure values in the population with velopharyngeal insufficiency; however, there were no significant differences between groups20.
Given the influence that cleft palate may have on orofacial functions (speech, chewing, swallowing, and breathing), speech therapy should be initiated at different times in this population through appropriate guidance to ensure that the development of such functions is within the age-expected standards whenever possible10,11.
As mentioned above and discussed in the literature, adequate velopharyngeal function does not always guarantee the correction of speech disorders. The need for speech therapy for the automation of complete velopharyngeal closure and correction of compensatory articulation to allow for better speech intelligibility is commonly observed12.
The speech therapy approach to the automation of adequate velopharyngeal closure aims to promote increased intraoral pressure during the production of speech sounds. Training methods have been developed that ensure that the patients gradually acquire proprioception and automation of this new pattern of velopharyngeal closure during the emission of isolated sounds, syllables, words, sentences, and spontaneous speech. Therefore, one can use visual, auditory and tactile-kinesthetic feedback strategies according to the difficulties presented by the patient12.
CONCLUSIONS
The hypothesis that individuals who undergo primary palatoplasty in adulthood have a higher occurrence of weak intraoral air pressure was rejected. The presence of weak intraoral air pressure was observed in the speech of individuals in both groups, and patient age at the time of primary palatoplasty was not an influencing factor.
REFERENCES
1. Cox TC. Taking it to the max: the genetic and developmental mechanisms coordinating midfacial morphogenesis and dysmorphology. Clin Genet. 2004;65(3):163-76.
2. Kummer AW. Anatomy and physiology: the orofacial structures and velopharyngeal valve. In: Kummer AW, ed. Cleft palate and craniofacial anomalies. 2nd ed. San Diego: Singular Thomson Learning; 2008. p.2-35.
3. Nahai FR, Williams JK, Burstein FD, Martin J, Thomas J. The management of cleft lip and palate: pathways for treatment and longitudinal assessment. Semin Plast Surg. 2005;19(4):275-85.
4. Robin NH, Baty H, Franklin J, Guyton FC, Mann J, Woolley AL, et al. The multidisciplinary evaluation and management of cleft lip and palate. South Med J. 2006;99(10):1111-20.
5. Landis P, Thi-Thu-Cuc P. Articulation patterns and speech intelligibility of 54 Vietnamese children with unoperated oral clefts: clinical observations and impressions. Cleft Palate J. 1972;12:234-43.
6. Rohrich RJ, Love EJ, Byrd HS, Johns DF. Optimal timing of cleft palate closure. Plast Reconstr Surg. 2000;106(2):413-21.
7. Kummer AW. Resonance disorders and velopharyngeal dysfunction (VPD). In: Kummer AW, ed. Cleft palate and craniofacial anomalies. 2nd ed. San Diego: Singular Thomson Learning; 2008. p.176-213.
8. Johns DF, Rohrich RJ, Awada M. Velopharyngeal incompetence: a guide for clinical evaluation. Plast Reconstr Surg. 2003;112(7):1890-7.
9. Perry JL, Kuehn DP. Magnetic resonance imaging and computer reconstruction of the velopharyngeal mechanism. J Craniofac Surg. 2009; 20 Suppl. 2:1739-46.
10. Peterson-Falzone SJ, Trost-Cardamone JE, Karnell MP, Hardin-Jones M. Effects of cleft and non-cleft VPI on speech in older children. In: The clinician's guide to treating cleft palate speech. St. Louis: Mosby; 2006. p.17-39.
11. Nóbrega ESS. Fissuras palatais. In: Mélega JM, ed. Cirurgia plástica: fundamentos e arte. Cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002. p.110-25.
12. Genaro KF, Fukushiro AP, Suguimoto MLFCP. Avaliação e tratamento dos distúrbios da fala. In: Trindade IEK, Silva Filho OG, org. Fissuras labiopalatinas: uma abordagem interdisciplinar. São Paulo: Santos; 2007. p.109-22.
13. Rudnick EF, Sie KC. Velopharyngeal insufficiency: current concepts in diagnosis and management. Curr Opin Otolaryngol Head Neck Surg. 2008;16(6):530-5.
14. Warren DW, Hall DJ, Davis J. Oral port constriction and pressure-air-flow relationships during sibilant productions. Folia Phoniatr. 1981;33(6):380-94.
15. Warren DW, Allen GD, King HA. Physiological and perceptual effects of induced anterior open bite. Folia Phoniatr. 1984;36(4):164-73.
16. Becker M, Svensson H, Sarnäs KV, Jacobsson S. Von Langenbeck or Wardill procedures for primary palatal repair in patients with isolated cleft palate: speech results. Scand J Plast Reconstr Surg Hand Surg. 2000;24(1):27-32.
17. Billmire DA. Surgical management of clefts and velopharyngeal dysfunction. In: Kummer AW, ed. Cleft palate and craniofacial anomalies. 2nd ed. San Diego: Singular; 2008. p.508-40.
18. Agrawal K. Cleft palate repair and variations. Indian J Plast Surg. 2009;42 Suppl.:S102-9.
19. Warren DW. Aerodynamic assessment of velopharyngeal function. In: Bzoch KR, ed. Communicative disorders related to cleft lip and palate. 4th ed. Austin: Pro-Ed Press; 1996.
20. Mayo R, Warren DW, Zajac DJ. Intraoral pressure and velopharyngeal function. Cleft Palate Craniofac J. 1998;35(4):299-303.
1. Master of Rehabilitation Science, Speech Therapist of the Instituto Central do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Central Institute of the Clinical Hospital of the Faculty of Medicine, University of São Paulo), São Paulo, SP, Brazil.
2. PhD in Sciences, Scientific Researcher of the Research Laboratory of Medical Rehabilitation Sciences (LIM 34), Faculdade de Medicina da Universidade de São Paulo (Faculty of Medicine, University of São Paulo - FMUSP), São Paulo, SP, Brazil.
3. Professor of Speech Therapy of the Department of Speech Therapy and Occupational Therapy, FMUSP, São Paulo, SP, Brazil.
4. Associate Professor of the FMUSP, plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery), São Paulo, SP, Brazil.
Correspondence to:
Nivaldo Alonso
Av. Dr. Enéas Carvalho de Aguiar, 255 - 8º andar - sala 8.128 - Cerqueira César
São Paulo, SP, Brazil - CEP 05403-000
E-mail: nivalonso@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 26, 2012
Article accepted: October 20, 2012
Financial support: Smile Train Foundation.
This study was performed at the Instituto Central do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Central Institute of the Hospital das Clinicas, Faculty of Medicine, University of São Paulo - USP), Department of Physical Therapy, Speech Therapy and Occupational Therapy of FMUSP, Department of Plastic Surgery, FMUSP, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter