

Original Article - Year 2012 - Volume 27 -
Lower lip reconstruction strategies
Estratégias em reconstrução do lábio inferior
ABSTRACT
BACKGROUND: The upper and lower lips represent the most important functional and aesthetic anatomical structures of the lower segment of the face. Given the complex functions of these structures, reconstruction of labial defects presents a challenge for plastic surgeons.
METHODS: Thirty patients with full-thickness lower lip defects underwent lip reconstruction according to the extent of the defect after tumor resection.
RESULTS: Six (20%) patients presented lesions of up to 30% of the total lip surface that required primary closure. Eighteen (60%) patients had lesions of 30-80% of the total area of the lower lip that were repaired using a myomucosal flap; in 14 of these patients, bilateral skin flaps were also used due to cutaneous involvement associated with the resection. Five (16.6%) patients had lesions on the lower lip that were adjacent to the oral commissure; therefore, they underwent reconstruction using an Abbé-Estlander flap with a myomucosal flap and bilateral skin flaps. One (3.5%) patient had a lesion covering 90% of the lower lip that was reconstructed using the Webster-Bernard technique and a tongue flap.
CONCLUSIONS: Here, we present a simplified, systematic, and literature-based strategy for planning lower lip reconstructions that employs effective and reproducible techniques, which can be used for training resident physicians in the treatment of complex lower lip lesions according to the extent of tissue loss, thereby yielding appropriate aesthetic and functional results.
Keywords: Lip/surgery. Surgical flaps. Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Os lábios superiores e inferiores representam as estruturas anatômicas funcionais e estéticas mais importantes do segmento inferior da face. Além disso, possuem funções complexas, sendo a reconstrução de defeitos labiais um desafio ao cirurgião plástico.
MÉTODO: Trinta pacientes apresentando defeitos de espessura total do lábio inferior foram submetidos a reconstrução do lábio baseada na extensão dos defeitos após exérese tumoral.
RESULTADOS: Seis (20%) pacientes apresentavam lesões de até 30% da superfície total do lábio, sendo realizado fechamento primário. Dezoito (60%) pacientes apresentavam lesões de 30% a 80% da superfície total do lábio inferior, sendo realizado retalho miomucoso de vermelhão; em 14 desses pacientes, em decorrência da perda cutânea associada à ressecção, foi associado retalho cutâneo mentolabial. Cinco (16,6%) pacientes tinham lesões no lábio inferior e comissura oral adjacente, sendo submetidos a reconstrução pela técnica de Abbé-Estlander com retalho miomucoso associado ao retalho cutâneo mentolabial. Um (3,5%) paciente apresentou lesão de 90% da superfície total do lábio inferior, sendo empregada técnica de Webster-Bernard associada ao retalho de língua.
CONCLUSÕES: Neste artigo é apresentada, de forma simplificada, sistemática e baseada na literatura, uma estratégia para planejamento da reconstrução do lábio inferior com utilização de técnicas eficazes e reprodutíveis em ambiente de aprendizado de médicos residentes, para tratamento de lesões complexas do lábio inferior, baseadas na extensão da perda de tecidos apresentada pelo paciente, com adequados resultados estético-funcionais.
Palavras-chave: Lábio/cirurgia. Retalhos cirúrgicos. Procedimentos cirúrgicos reconstrutivos.
The upper and lower lips are the most important functional and aesthetic anatomical structures of the lower segment of the face. The lips contribute to chewing, speech, facial expressions, and oral competence. Due to these complex functions, the reconstruction of lip defects can pose a challenge to plastic surgeons that seek to achieve excellence in aesthetic and functional lip restoration. Infections, traumatic injuries, congenital abnormalities, and tumors (including squamous cell carcinoma) most often cause defects in the lower lip1. Surgical trauma resulting from lip resections can result in significant changes in lip appearance and normal function, which deeply impact patient self-image and quality of life.
Subtle changes in the appearance of the vermilion border, oral commissure, or cupid's bow are easily detected by the casual observer. The loss of lip competence can interfere with articulation, whistling, kissing, and the containment of salivary secretions. Thus, the functional and aesthetic reconstruction of the lip has been described for centuries2. Reconstruction can be very effective for small defects. However, the larger the defect, the more difficult it is to create an aesthetically pleasing and functional lip.
In the present study, we describe a strategy for lower lip reconstruction based on the size and location of defects, which primarily occur following resection of tumor lesions, that involves the use of treatments ranging from primary closure to local flaps of the remaining structures. This study was performed at the Department of Plastic Surgery, St. Luke's Hospital, Catholic University of Rio Grande do Sul (Porto Alegre, RS, Brazil).
METHODS
The proposed strategy was applied from January 2010 to June 2011 in 30 patients with full-thickness defects of the lower lip that did or did not affect the adjacent labia. Patients with isolated defects of the skin, mucosa, or vermilion alone were excluded. Two patients with lesions on the upper lip were also excluded from the study. The average patient age was 58 years.
All lip defects were caused by resection of a squamous cell carcinoma that required repair by the plastic surgery team.
The surgical reconstruction technique was determined according to the extent and location of the defect resulting from the tumor resection by assessment of the percentage of the lip defect (Figure 1). The safety margins of the resection were 1 cm, and pathological examination revealed tumor-free margins in all cases. Visualization was performed as a freezing examination during the perioperative period in the lesions in which the margins were poorly defined.
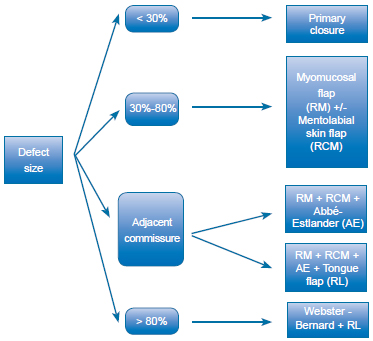
Figure 1 - Flowchart showing the technique used according to lip defect extent. AE = Abbé-Estlander technique; PC = primary closure; MSF = mentolabial skin flap; TF = tongue flap; VMF = vermilion myomucosal flap; WB = Webster-Bernard technique.
The patients were evaluated in the postoperative period in terms of microstomy, salivary continence, flap viability, dehiscence, and postoperative infection.
RESULTS
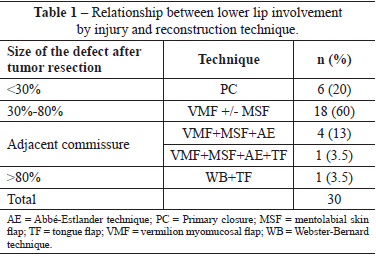
Of the 30 patients operated, 6 had lesions covering 30% of the total area of the lower lip and underwent primary closure of the lesion (Figure 2). Eighteen patients had lesions covering 30%-80% and underwent lip reconstruction with the use of a vermilion myomucosal flap (Figure 3). In 14 of these patients, bilateral skin flaps were also used due to skin loss associated with resection (Figure 4). Five patients who had lesions on the lower lip adjacent to the oral commissure underwent reconstruction using the Abbé-Estlander flap technique with a myomucosal flap and bilateral skin flaps (Figure 5); one of these procedures also required the use of a tongue flap to reconstruct the mucosa (Figure 6). One patient had a lesion covering 90% of the lower lip that was reconstructed using the Webster-Bernard technique and a tongue flap (Figure 7, Table 1).

Figure 2 - Defect of up to 30% demonstrating the primary closuretechnique in stages. In A, preoperative appearance. In B, intraoperative aspect exposing the full thickness of the lip defect. In C, closure without flaking. In D, final appearance 2 weeks postoperatively.

Figure 3 - A 45-year-old patient who underwent reconstruction of 45% of the lower lip with advancement of the myomucosal flap of the oral orbicular muscle. In A, secondary defect due to neoplasm resection. In B, dissected myomucosal vermilion flap. In C, appropriately positioned flaps.

Figure 4 - A 52-year-old patient who underwent reconstruction of 70% of the lower lip. In A, preoperative tumor aspect and marking of the areas to be dissected. In B, bilaterally dissected myomucosal vermilion flaps. In C, bilaterally dissected skin flaps. In D, immediate postoperative appearance in which the advancement myomucosal flap is associated with the mentolabial skin flap via the distal intersection.
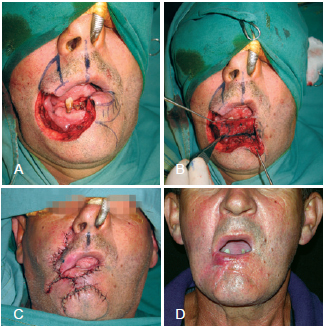
Figure 5 - A patient with a large defect in the lower lip secondary to tumor resection affecting approximately 80% of the lip and adjacent commissure. In A, defect created after oncologic resection. In B, dissected myomucosal vermilion flap. In C, rotated Abbé-Estlander flap positioned for reconstruction with the myomucosal flaps and the mentolabial skin flap. In D, final appearance after commissuroplasty.
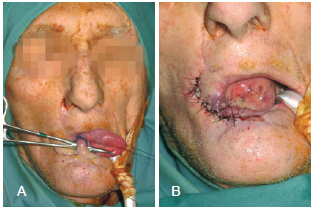
Figure 6 - A tongue flap was used in mucosal reconstruction in some cases. In A, non-autonomized flap. In B, autonomized flap.
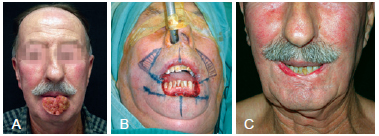
Figure 7 - Webster-Bernard flap. In A, extensive lesion involving the lower lip. In B, secondary tumor resection defect affecting approximately 90% of the lower lip. Demarcated triangles in the nasolabial folds indicate the regions that will allow the advancement of the cheek flaps for defect closure. In C, final reconstruction aspect.
Patients underwent assessments at 2, 4, 6, 12, and 18 months postoperatively. During this period, one patient who underwent reconstruction with a myomucosal flap and bilateral skin flaps showed cutaneous dehiscence, whereas another demonstrated epidermolysis of the mentolabial skin flap that did not require further surgical intervention. Three patients presented with microstomy and posterior enlargement, and one underwent commissuroplasty in a second surgical procedure and indicated a good functional outcome (Figure 8). In the 2 cases in which we used a tongue flap to reconstruct part of the vermilion, autonomization was performed 3 weeks postoperatively. All of the 5 patients who had lesions in the adjacent oral commissure that were reconstructed using the Abbé-Estlander flap technique with a myomucosal flap and bilateral skin flaps underwent a subsequent oral commissuroplasty 3 months after the initial reconstruction that aimed to restore the usual commissure form and the normal fading of the vermilion.

Figure 8 - Converse commissuroplasty used in cases in which the commissure was affected. In A, commissuroplasty marking. In B, final appearance.
All cases showed good sensitivity and proper sphincter function.
DISCUSSION
Lip cancer is the most common malignancy in the oral cavity (15%), of which squamous cell carcinoma - the most common type - has a prevalence that is 20 times higher in the lower lip than in the upper lip3.4.
The primary goal in labial reconstruction includes adequate coverage of the red and adjacent skin associated with reconstitution of the oral sphincter competence with minimal aesthetic functional alterations. Thus, many methods have been proposed for reconstructing the lower lip, which may be indicated based on the extent of loss. Approximately 200 techniques related to this topic have been described in the literature5.
When planning a lower lip repair, it is necessary to evaluate the extent of the loss to be reconstructed. Wedge or V resection and primary closure are very common options for repairing defects of up to one-third of the lip area. The repair of full-thickness defects requires accurate approximation of the 3 tissue layers: mucous, muscle, and skin. However, substance losses greater than one-third of the area require more complex reconstructions and more elaborate surgical planning and may involve the use of pedicle flaps (local or remote) or free flaps. To facilitate systematization, injuries are classified according to their location in relation to the commissure and are divided into defects that affect or approach the commissure and defects that are limited to the central lip4,5.
In the cases of central lesions covering 30%-80% of the labial surface, we used orbicularis advancement flaps with or without mentolabial skin flaps according to the skin coverage available for repair. This technique was employed due to the relative ease of implementation and the maintenance of innervation of the remaining lip, which is essential for its functionality. The basic principle of procedure systematization depends on the presence of redundant tissues within the vermilion. The cutaneous portion has lower elasticity than other regions of the face and neck; however, the redundancy of the lip vermilion can be a favorable factor in lip reconstruction1.
The myomucosal flap maintains the innervation to the lower lip and minimizes the loss of the transverse dimension and the risk of microstomy. The defect should be carefully evaluated and, to ensure good functional and aesthetic results, at least 20% of the remaining lower lip must be distributed unilaterally or bilaterally. Volume and lip aesthetics are maintained as a result of the recruitment of similar adjacent tissues. The incision is easily camouflaged in the vermilion. The flap can be created with ease and confidence and is associated with favorable long-term results.
In 1974, Karapandzic6 described the use of the myocutaneous neurovascular flap, avoiding sections of muscle fibers of the oral orbicularis and causing minimal sensory and motor damage, for losses of 60-80% of the lip. Microstomy, the rounding of the commissure, and modiolus displacement, are its main disadvantages.
Defects involving the commissure require careful planning. In 1872, Estlander7 described the original technique for reconstructing these defects. Reconstruction of the lower lip involved the rotation of a lateral area of the upper lip to the commissure. A second surgery is necessary to reconstruct the commissure angle. The modified Estlander flap is based more medially to the initially proposed flap and seeks to avoid lip commissure deformations. The technique used at our institution to reconstruct commissure defects abides by the principles described by 4 authors (Estlander7, Goldstein8, Robottiet al.9, and Yamauchi et al.10). The use of an innervated myomucosal flap and an Estlander flap allows for the reconstruction of large defects affecting the lower lip and adjacent oral commissure and provides satisfactory functional and aesthetic results. Three months after the initial reconstruction, a commissuroplasty using the Converse11 technique is performed that aims to restore the usual form of the commissure and the normal fading of the vermilion. A triangle of skin and subcutaneous tissue is excised at the point corresponding to the position of the contralateral normal commissure. The labial mucosa is then moved on each side of the incision to restore the vermilion surface (Figure 8).
In patients with almost a total defect of the lower lip, we used the Webster-Bernard flap, which involved the medial advancement of the cheek tissue to create a new lower lip. In 1845, Dieffenbach12 was the first to suggest lower lip reconstruction using bilateral medial advancement flaps of the cheeks. In 1853, Bernard13 presented a technique that in volved triangular resection of the bilateral Burow flap in the nasolabial folds. Subsequently, this procedure underwent modification by Ginestet14 in 1946, Freeman15 in 1958, and Webster et al.16, in 1960. According to the Webster technique, the orbicularis and buccinator muscles are incised laterally to the commissure to advance the lower lip reconstruction17,18.
CONCLUSIONS
Due to the superiority of the techniques that employ the remaining labial tissue, a certain degree of microstomy is preferable for reconstruction using other tissues. Thus, when possible, in cases of lower lip reconstruction, tissues from the remaining lip should be employed or a flap should be taken from the upper lip, according to defect size and location19. This study presented a simplified, systematic, and literature-based strategy for planning lower lip reconstructions using efficient and reproducible techniques for training resident physicians in the treatment of complex lower lip lesions, based on the extent of tissue loss, to yield appropriate aesthetic and functional results.
REFERENCES
1. Oliveira MP, Martins PDE, Cunha GL, Alvarez GS, Gazzalle A, Siqueira EJ. Use of the vermilion myomucosal flap with or without the mentolabial skin flap for lower lip reconstruction. Rev Bras Cir Plást. 2011;26(3):433-8.
2. Ducic Y, Athre R, Cochram CS. The split orbicularis myomucosal flap for lower lip reconstruction. Arch Facial Plast Surg. 2005;7(5):347-52.
3. Turgut G, Ozkaya O, Kayali MU, Tatlidede S, Huthut I, Baş L. Lower lip reconstruction with local neuromusculocutaneous advancement flap. J Plast Reconstr Aesthet Surg. 2009;62(9):1196-201.
4. Neligan P, Gullane P, Werning J. Lip reconstruction. In: Werning J, ed. Oral cancer. New York: Thieme Medical Publishing; 2006. p.180-93.
5. Neligan PC. Strategies in lip reconstruction. Clin Plast Surg. 2009;36(3):477-85.
6. Karapandzic M. Reconstruction of lip defects by local arterial flaps. Br J Plast Surg. 1974;27(1):93-7.
7. Estlander JA. Eine methode aus der einen lippe substanzverluste der anderen zu erstzen. Arch Klin Chir. 1872;14:622. Reprinted in English in Plast Reconstr Surg. 1968;42:361.
8. Goldstein MH. A tissue-expanding vermilion myocutaneous flap for lip repair. Plast Reconstr Surg. 1984;73(5):768-70.
9. Robotti E, Righi B, Carminati M, Ortelli L, Bonfirraro PP, Devalle L, et al. Oral commissure reconstruction with orbicularis oris elastic musculomucosal flaps. J Plast Reconstr Aesthet Surg. 2010;63(3):431-9.
10. Yamauchi M, Yotsuyanagi T, Ezoe K, Saito T, Yokoi K, Urushidate S. Estlander flap combined with an extended upper lip flap technique for large defects of lower lip with oral commissure. J Plast Reconstr Aesthet Surg. 2009;62(8):997-1003.
11. Converse JM. Reconstructive plastic surgery. 2nd ed. Philadelphia: Saunders; 1977.
12. Dieffenbach JF. Die operative chirurgie. Leipzing: Brockhaus; 1845.
13. Bernard C. Cancer de la levre inferieure opere par un proced nouveau. Bull Mem Soc Chir Paris. 1853;3:357.
14. Ginestet G, Landwerlin F. Trois cas de constriction permanente desmâchoires d'origine articulaire ou osseuse para-articulaire. Rev Odontostomatol. 1946;2:197-201.
15. Freeman BS. Myoplastic modification of the Bernard cheiloplasty. Plast Reconstr Surg Transplant Bull. 1958;21(6):453-60.
16. Webster RC, Coffey RJ, Kelleher RE. Total and partial reconstruction of the lower lip with innervated muscle bearing flaps. Plast Reconstr Surg. 1960;25:360-71.
17. Unsal Tuna EE, Oksuzler O, Özbek C, Ozdem C. Functional and aesthetic results obtained by modified Bernard reconstruction technique after tumor excision in lower lip cancers. J Plast Reconstr Aesthet Surg. 2010;63(6):981-7.
18. Wechselberger G, Gurunluoglu R, Bauer T, Piza-Katzer H, Schoeller T. Functional lower lip reconstruction with bilateral cheek advancement flaps: revisitation of Webster method with a minor modification in the technique. Aesthetic Plast Surg. 2002;26(6):423-8.
19. Alvarez GS, Siqueira EJ, de Oliveira MP. A new technique for reconstruction of lower-lip and labial commissure defects: a proposal for the association of Abbe-Estlander and vermilion myomucosal flap techniques. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013 (in press).
1. Plastic surgeon, specialist member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), Porto Alegre, RS, Brazil, Porto Alegre, RS, Brazil.
2. Plastic surgeon, specialist member of SBCP, Doctoral student in Medicine and Health Sciences at Pontifícia Universidade Católica do Rio Grande do Sul (Catholic University of Rio Grande do Sul - PUCRS), Porto Alegre, RS, Brazil.
3. Resident surgeon in Plastic Surgery at Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (St. Luke's Hospital, Catholic University of Rio Grande do Sul), Porto Alegre, RS, Brazil.
4. PhD, full member of the SBCP, Head of the Department of Plastic Surgery, Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (St. Luke's Hospital, Catholic University of Rio Grande do Sul - PUCRS), Porto Alegre, RS, Brazil.
5. Master, full member of the SBCP, preceptor of the Plastic Surgery Service of the Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (St. Luke's Hospital, Catholic University of Rio Grande do Sul - PUCRS), Doctoral student in Medicine at Universidade Federal de Ciências da Saúde de Porto Alegre (Federal University of Health Sciences of Porto Alegre), Porto Alegre, RS, Brazil.
Correspondence to:
Evandro José Siqueira
Rua Sinimbu, 1.878 - Sala 502 - Bairro Centro
Caxias do Sul, RS, Brazil - CEP 95020-002
E-mail: ejsique@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 24, 2012
Article accepted: October 23, 2012
This study was performed at Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (St. Luke's Hospital, Catholic University of Rio Grande do Sul), Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter