

Special Article - Year 2012 - Volume 27 -
Systematization of dressings for clinical treatment of wounds
Sistematização de curativos para o tratamento clínico das feridas
ABSTRACT
The treatment of cutaneous wounds includes both medical and surgical methods; dressing is one of the most commonly used clinical treatments. An extensive therapeutic toolkit comprising passive dressings or dressings with active principles can help repair wounds in various situations. Dressings are used to improve the conditions of the wound bed and may occasionally be considered the definitive treatment, whereas in some cases, they may be considered an intermediate step to surgical treatment. Intelligent and biological wound dressings are currently classified as dermal substitutes and will not be discussed in this article. Dressings should be selected on the basis of knowledge of the pathophysiology of wound healing and tissue repair while keeping the systemic problems of the patient in mind.
Keywords: Bandages. Wound healing. Wounds and injuries.
RESUMO
O tratamento das feridas cutâneas inclui métodos clínicos e cirúrgicos, sendo o curativo um dos tratamentos clínicos mais frequentemente utilizados. Um vasto arsenal terapêutico composto por curativos passivos ou com princípios ativos é capaz de auxiliar na reparação do tegumento em diversas situações. Curativos visam a melhorar as condições do leito da ferida, podendo ser, em algumas ocasiões, o próprio tratamento definitivo, mas em muitas situações constituem apenas uma etapa intermediária para o tratamento cirúrgico. Curativos inteligentes e biológicos são hoje mais bem classificados como substitutos cutâneos e não serão considerados neste artigo. A escolha do curativo a ser utilizado deve ser baseada no conhecimento das bases fisiopatológicas da cicatrização e da reparação tecidual, sem nunca esquecer o quadro sistêmico do paciente.
Palavras-chave: Bandagens. Cicatrização. Ferimentos e lesões.
Since ancient times, maintenance of skin continuity has been an important topic in medicine1. The treatment of wounds includes both surgical and clinical methods, with dressing being the most frequently used clinical treatment to aid tissue repair2. Suitable material for dressings is selected on the basis of pathophysiological and biochemical knowledge of the mechanisms underlying wound healing and tissue repair.
Wounds involve not only rupture of the skin and subcutaneous tissue but also injury to muscles, tendons, and bones in some cases. Wounds can be classified according to etiology, complexity, and time of existence3.
Traumas, burns, pressure ulcers, venous ulcers, wounds in the lower limbs of patients with diabetes, and radiation therapy wounds are examples of some of the wounds encountered in clinical practice.
In terms of complexity, a simple wound is defined as one that resolves spontaneously following the 3 main stages of physiological healing: inflammation, cell proliferation, and tissue remodeling4. Lesions that affect large and/or deep areas require special treatment for resolution and their natural course of progression has to be amended; these wounds represent a threat to the viability of a member. Recurring wounds that reopen or require more elaborate treatment are referred to as complex wounds5.
Ferreira et al.5 defined criteria to classify the complexity of a wound: (I) extensive and profound loss of integument; (II) presence of local infection; (III) impairment of tissue viability with necrosis; and (IV) association with systemic diseases that hinder the physiological process of tissue repair.
Dressings or bandages are therapeutic methods that involve cleaning and the application of material to a wound for protection, absorption, and drainage in order to improve the conditions of the wound bed and assist its resolution. In some situations, dressings can be considered the definitive treatment, whereas they are only an intermediate step for surgical treatment in others6.
Many dressing materials are currently available for different stages of wound management, including cleaning, debridement, reduction of bacterial population, exudate control, granulation stimulation, and protection of re-epithelialization.
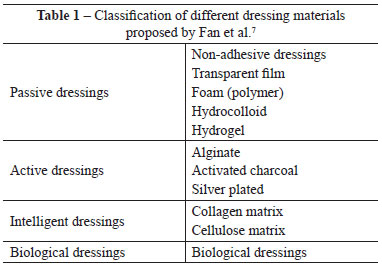
Fan et al.7 suggest that dressings should be classified as passive dressings, dressings with active principles, intelligent wound dressings, and biological dressings. Table 1 lists the types of dressings as described in the literature.
According to clinical experience in the Outpatient Center, Surgical Wards, and Division of Plastic Surgery of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clinicas, Faculty of Medicine, University of São Paulo) - HCFMUSP, we consider it more appropriate to differentiate dressings (passive dressings and those with active principles) from synthetic or biosynthetic dermal substitutes. In the present work, we will only discuss passive dressings and ones with active principles and not dermal substitutes.
METHODS
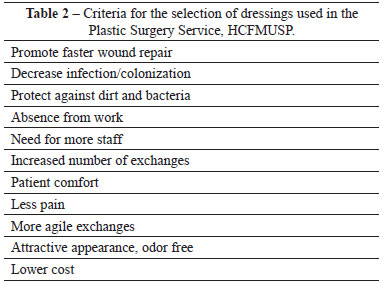
The criteria for the selection of the type of dressing to be used in the Division of Plastic Surgery, HCFMUSP are shown in Table 2.
RESULTS
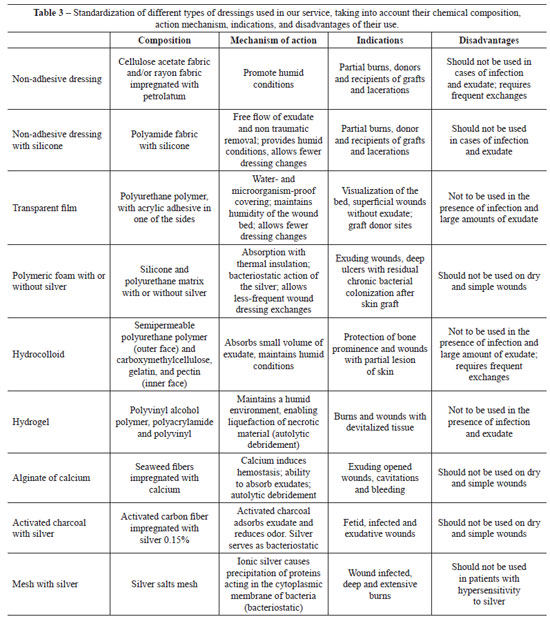
Table 3 presents the systematization proposed in our service, listing products along with their composition, action mechanisms, indications, and disadvantages.
DISCUSSION
In wounds that do not heal normally, the physiological tissue-repair process is not coordinated properly by signal molecules (i.e., TGF-β, PDGF, IGF-1, VEGF, and FGF), and the biochemical mechanisms mediated by cytokines (i.e., TNF-α, IL-1, and INF-γ) are ineffective8. In such cases, the tissue repair process is not completed properly; therefore, the integrity of the integument is not re-established.
Acute wounds are wounds that resolve within 3 weeks. Some authors advocate that the wound should be considered chronic only after 3 or 4 months of non-resolution9. Considering the more modern treatments for wounds, the previous definition does not seem reasonable. Therefore, we believe wounds that fail to resolve after 3 weeks should be classified as chronic.
In the treatment of the wounds, dressings can be classified as those used to cover the wound (i.e., bandages) or those that carry any active principal to the bed of the wound. We classified intelligent or biological dressings as dermal replacement of the degraded dermis. This subject deserves substitutes, because their actions are more dependent on the an independent publication10.
The use of passive dressings was first described in the literature in 1962, when Winter11 demonstrated that re-epithelialization occurs more rapidly in dressed wounds than in wounds exposed to air. The author attributed this phenomenon to the humid environment provided by the dressing. Hinman & Maibach12 reported similar results in humans.
Dressings with active principles possess topical action dependent on their chemical composition13. These active ingredients act mainly on enzymatic debridement and control the bacterial population during preparation of the wound bed.
Dressings referred to as "intelligent" by Fan et al.7 can alter the microenvironment of the bed of a chronic wound, stimulating endogenous signals responsible for orchestrating wound repair. Such signals are cytokines (i.e., growth factors), which are gaining increasing importance in this context14.
Allografts or heterogeneous tissues, which are used to temporarily replace the human skin in injuries such as burns, traumatic wounds, chronic ulcers, or diabetic wounds, should not be termed biological dressings in our opinion; they are rather components of the surgical procedures performed by plastic surgeons.
The gold standard for reconstruction of the cutaneous tegument has been established as autogenous skin grafting15.
The negative-pressure therapy described by Argenta & Morikwas16 in 1997 and introduced in Brazil in 2003 by Ferreira et al.17 is gaining acceptance in current practice as an additional option for the treatment of wounds, especially for preparation of the wound bed. However, it should not be considered curative.
Another important aspect to be highlighted is that the physiologic non-resolution of a wound is often associated with the presence of systemic comorbidities and specific situations such as malnutrition, autoimmune diseases, diabetes, and corticosteroid therapy9.
The treatment of skin wounds is dynamic, depending on the evolution of the tissue repair stages and is initially clinical, mainly involving the use of dressings or bandages. Surgical treatment should be used when the initial treatment proves to be ineffective or too slow8.
In addition to passive dressings (i.e., inert) or those with active principles, the variety of dressings is currently increasing, as is the pressure for the pharmaceutical industry to take up space in the market. Despite this, no universal dressings are available for all wounds. However, the currently available vast therapeutic arsenal can assist tissue repair in various situations. Health professionals must choose the best therapeutic option, taking into consideration the systemic framework involved in the treatment of a wound.
REFERENCES
1. Jones JE, Nelson EA. Skin grafting for venous leg ulcers. Cochrane Database Syst Rev. 2005;25(1):CD001737.
2. Chung KC, Glori AK. Systematic review of skin graft donor-site dressings. Plast Reconstr Surg. 2009;124(1):307-8.
3. Kanj LF, Wilking SV, Phillips TJ. Pressure ulcers. J Am Acad Dermatol. 1998;38(4):517-36.
4. Isaac C, Ladeira PRS, Rego FMP,Aldunate JCB, Ferreira MC. Processo de cura das feridas: cicatrização fisiológica. Rev Med. 2010;89(3/4):125-31.
5. Ferreira MC, Tuma Jr. P, Carvalho VF, Kamamoto F. Feridas complexas. Clinics. 2006;61(6):571-8.
6. Harding KG, Morris HL, Patel GK. Science, medicine and future: healing chronic wounds. BMJ. 2002;324(7330):160-3.
7. Fan K, Tang J, Escandon J, Kirsner RS. State of the art in topical wound-healing products. Plast Reconstr Surg. 2011;127 Suppl 1:44S-59S.
8. Grazul-Bilska AT, Johnson ML, Bilski JJ, Redmer DA, Reynolds LP, Abdullah A, et al. Wound healing: the role of growth factors. Drugs Today. 2003;39(10):787-800.
9. Harding KG, Morris HL, Patel GK. Science, medicine and future: healing chronic wounds. BMJ. 2002;324(7330):160-3.
10. Ferreira MC, Paggiaro AO, Isaac C, Teixeira Neto N, Santos GB. Substitutos cutâneos: conceitos atuais e proposta de classificação. Rev Bras Cir Plást. 2011;26(4):696-702.
11. Winter GD. Formation of the scab and the rate of epithelization of superficial wounds in the skin of the young domestic pig. Nature. 1962;193:293-4.
12. Hinman CD, Maibach H. Effect of air exposure and occlusion on experimental human skin wounds. Nature. 1963;200:377-8.
13. Franco D, Gonçalves LF. Feridas cutâneas: a escolha do curativo adequado. Rev Col Bras Cir. 2008;35(3):203-6.
14. Alves HR, Almeida PC, Grillo VA, Smaniotto P, Santos DV, Ferreira MC. Clinical experiences of using a cellulose dressing on burns and donor site wounds. J Wound Care. 2009;18(1):27-30.
15. Lindford AJ, Kaartinen IS, Virolainen S, Kuokkanen HO, Vuola J. The dermis graft: another autologous option for acute burn wound coverage. Burns. 2012;38(2):274-82.
16. Argenta LC, Morikwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38(6):563-76.
17. Ferreira MC, Wada A, Tuma Jr P. The vacuum assisted closure of complex wounds: report of 3 cases. Clinics. 2003;58(4):277-30.
1. Resident of Plastic Surgery, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clinicas, Faculty of Medicine, University of São Paulo) - HCFMUSP, São Paulo, SP, Brazil.
2. Full professor of Plastic Surgery, Faculdade de Medicina da Universidade de São Paulo (Faculty of Medicine, University of São Paulo), full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), São Paulo, SP, Brazil.
3. Assistant physician in the Division of Plastic Surgery HCFMUSP, full member of the SBCP, São Paulo, SP, Brazil.
Correspondence to:
Pedro Henrique de Souza Smaniotto
Rua Abílio Soares, 666 - ap. 21B - Paraíso
São Paulo, SP, Brazil - CEP 04005-002
E-mail: pedrofmusp@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: December 13, 2011
Article accepted: January 18, 2012
This study was performed at the Division of Plastic Surgery, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clinicas, Faculty of Medicine, University of São Paulo), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter