

Original Article - Year 2012 - Volume 27 -
Treatment of coxofemoral dysmorphia in formerly obese patients
Tratamento das dismorfias coxofemorais em pacientes ex-obesos
ABSTRACT
BACKGROUND: Patients showing massive weight loss eventually develop excessive skin and fat in several body parts, including the lower extremities. Given the diversity of the localization, shape, and content of coxofemoral dysmorphia, this study proposes guidelines for planning and systematizing the treatment of each deformity.
METHODS: Twenty-eight female patients who underwent thigh lifts and showed 3 types of deformities were assessed. The deformities encompassed the upper third of the thigh alone, the upper and middle thirds, or the entire medial aspect of the thighs. A specific technique was used for treating each type of deformity. Moreover, when necessary, suspension of the lateral thigh was combined with liposuction. Patient satisfaction with the surgical results was assessed by a graded questionnaire. Unexpected events, complications, and treatments were recorded.
RESULTS: Mobility, hygiene, sexual performance, use of clothing, and scars were assessed as excellent (80.5%), good (14.5%), and regular (5%).
CONCLUSIONS: Considering the broad heterogeneity of thigh dysmorphia in formerly obese patients, therapeutic guidelines correlating each type of deformity with a specific treatment are necessary.
Keywords: Bariatric surgery. Weight loss. Plastic surgery. Thigh/surgery.
RESUMO
INTRODUÇÃO: Os pacientes que apresentam perda poderal maciça evoluem com sobras dermogordurosas em várias áreas corporais, incluindo os membros inferiores. Diante da heterogeneidade de localização, forma e conteúdo das dismorfias coxofemorais, este trabalho oferece um roteiro de planejamento e sistematização para tratamento de cada uma das deformidades.
MÉTODO: Foram avaliadas 28 pacientes do sexo feminino que realizaram coxoplastias e que apresentavam basicamente 3 tipos de deformidade, que poderiam envolver apenas o terço superior, os terços superior e médio ou toda a face medial das coxas. Para cada tipo de deformidade foi aplicada técnica específica; além disso, quando necessário, foi associada suspensão da face lateral das coxas e lipoaspiração. A satisfação das pacientes com os resultados cirúrgicos foi avaliada por meio da aplicação de questionários e notas atribuídas a cada resposta. Foram enumerados intercorrências, complicações e tratamento aplicado.
RESULTADOS: Os itens mobilidade, higiene, desempenho sexual, vestimentas e cicatrizes foram avaliados como ótimo (80,5%), bom (14,5%) e regular (5%).
CONCLUSÕES: Considerando-se a grande heterogeneidade de dismorfias das coxas em pacientes ex-obesos, um roteiro de tratamento relacionando a deformidade ao tratamento deve ser incorporado ao arsenal cirúrgico.
Palavras-chave: Cirurgia bariátrica. Perda de peso. Cirurgia plástica. Coxas/cirurgia.
Coxofemoral dysmorphia after weight loss is characterized by ptotic skin folds and disfigured local contour. Loss of fat content is accompanied by structural dermal modifications that are characterized by qualitative and quantitative changes in elastin and collagen and result in decreased elasticity of the skin, which loses its retractability and allows ptosis of the folds1. In thighs, this condition is more pronounced on the medial aspect, where the skin and superficial fascia are thinner2. On the lateral aspect, the remaining fat accumulation remains significant, even after weight loss, and folds are less frequently present due to the powerful underlying muscles and the thicker superficial fascia that results from denser connective tissue.
According to the Pittsburgh scale, such dysmorphia is classified into 3 types, in which type 3 patients show skin folds on the medial aspects of the thighs and these folds can extend from the inguinal fold to the knees3. For this group of patients, treatment involves resection of the excess skin with or without liposuction. The skin folds in these patients may be located only in the upper third of the medial aspect of the thighs (Group 1), in the upper and middle thirds (Group 2), or throughout the medial aspect of the thighs (Group 3).
Given such heterogeneity in the location, shape, and content of coxofemoral dysmorphia, the present study provides some guidelines for planning and systematizing the treatment of each deformity.
METHODS
Patients
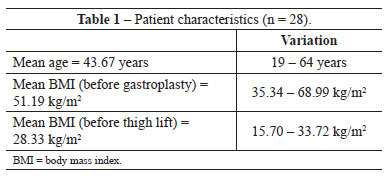
Treatment was performed for 28 female patients who had undergone gastroplasty for obesity therapy and had maintained a stable weight for > 18 months (Table 1). All patients were in good clinical condition, were non-smokers, and did not use drugs that might have caused behavioral changes. No patient was using a hormonal contraceptive or replacement therapy.
The patients received psychological assistance in both the pre- and postoperative periods to ensure understanding of the surgical proposal and to overcome potential result-related frustration. Each patient provided written informed consent after being informed about the study protocol.
The patients were grouped together according to dysmorphia type. Group 1 included 3 patients whose skin folds accumulated on the upper third of the thigh below the inguinal fold. Group 2 included 9 patients who had dermal fatty folds extending from the inguinal fold to the middle third of the medial aspect of the thigh. Group 3 included 16 patients with flaccid and ptotic skin folds along the full length of the thigh.
Surgical Techniques
Patients in Group 1 underwent a thigh lift as proposed by Lockwood4. With the patient in a standing position and the thighs moderately apart, a posterior point was marked that corresponded to the ischial spine projection; from there, a line was drawn continuing anteriorly through the inguinal fold. Another line parallel to the first was drawn 2 cm above, and using 2-finger pinching, a spindle shape containing the excess dermal fatty area to be resected was marked (Figure 1). It is important to note that excessive tissue removal must be avoided to prevent stress on the sutures. Resection was performed above the superficial fascia to preserve the local vascular system, especially the lymphatic vessels. Subsequently, under the fat of the vulva from the ischiopubic insertion of the thigh's adductor muscles, Colles' fascia was identified and sutured with 3 polyamide 2-0 stitches to the superficial fascia of the lower margin of the surgical wound (Figure 2). Wound closure was performed in 3 planes: a deep plane with separate polyamide wire 3-0 stitches, a subdermal plane with separate poliglecaprone acid thread 4-0 sutures, and an intradermal plane with continuous poliglecaprone acid 4-0 absorbable thread sutures.
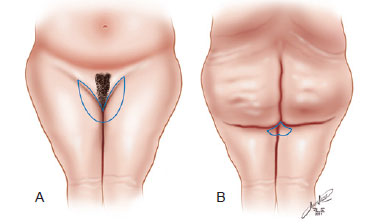
Figure 1 - Representation of the drawing of incisions according to Lockwood's technique. In A, anterior view. In B, posterior view.
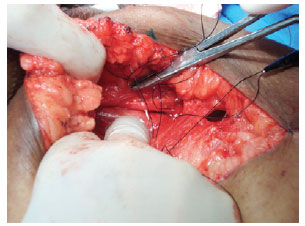
Figure 2 - Needle transfixing Colles' ligament for suturing the superficial fascia of the inferior border of the surgical wound.
In Group 2, the Lewis technique5 was used. This technique involves the inguinal transversal resection proposed by Lockwood4 with a longitudinal sickle-shaped incision; this procedure initiates at the posterior end of the transverse incision and draws an ellipse containing the dermal fatty excess with anterior concavity and extends longitudinally, along the middle third of the thigh, similar to the drawing of a sickle (Figure 3). The excess tissue to be resected was identified by 2-finger pinching with care to avoid exaggerated resections that could cause suture stress. An incision and dissection were performed above the superficial fascia, which was sutured in the inguinocrural portion to Colles' ligament with 3 polyamide 2-0 thread sutures. The use of such a suture, in addition to fixating the fold above, avoids traction-induced deformities of the vulva. The wound was closed in 3 planes: a deep plane with separate polyamide 3-0 thread stitches, a subdermal plane with separate poliglecaprone acid 4-0 thread stitches, and an intradermal plane with continuous acid poliglecaprone 4-0 sutures.
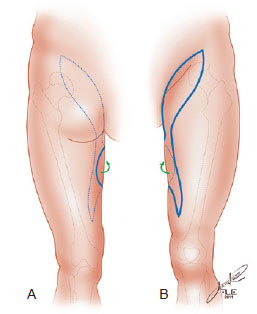
Figure 3 - Drawing of the incisions encompassing the sickle-shaped area as proposed by Lewis. In A, posterior view. In B, anterior view.
In Group 3, the technique proposed by Cram & Aly6 was used. The resection followed the drawing of a longitudinal spindle, which was extended from 2 cm below the middle point between the insertion tendons of the adductor and gracilis muscles of the thigh to 2-3 cm posterior to the medial condyle of the femur (Figure 4). As in the other groups, the spindle was drawn using 2-finger pinching with the patient in the standing position and with care to avoid exaggerated resections.
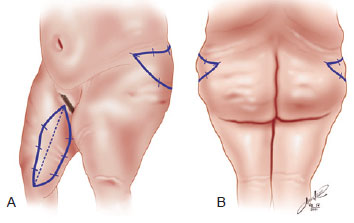
Figure 4 - Diagram showing the spindle-shaped marks on the medial side of the thigh according to Cram & Aly's technique and the resection drawing on the superior lateral portion of the thigh according to Baroudi. In A, oblique view. In B, posterior view.
In some patients, regardless of group, when a fatty excess existed in the thighs with the folds, liposuction was performed to decrease the fat content and allow a more adequate resection without excess, thus preventing suture stress.
Patients showing gluteal medial fatty deposits underwent surgery supplemented with tumescent liposuction and resection of the remaining fold, as proposed by Baroudi7. Aspindle was drawn on the lateral and upper region of the thigh, limited above by a line determined by prolongation of the inferior abdominal grove and below by 2-finger pinching of the skin with the patient standing. Resection was performed above the superficial fascia, and closure was performed in 3 planes similar, as previously described (Figure 4).
No drains were used in any of the procedures. The dressings were prepared with gauze spread with an antibiotic cream over which a truss-shaped microporous surgical tape was applied. Perioperative antibiotic therapy was initiated with cephalosporin and maintained for 5-7 days. Anticoagulation therapy with low molecular weight heparin derivatives was prescribed for patients who were at risk of thrombophilia. In patients who underwent concomitant liposuction, bermuda-type moderate compression girdles were used.
Early walking was encouraged during the postoperative period. Walking was combined with resting periods in which the lower extremities were subjected to intermittent and alternate compression. Massage of the thighs and legs was recommended 10-15 days after surgery to favor venous and lymphatic drainage and minimize lower extremity edema. Even after discharge, the use of moderate compression elastic stockings was recommended. Patients who underwent liposuction concomitant with the thigh lift were advised to keep wearing the bermudas. The dressings were replaced every 3 days or earlier as needed.
RESULTS
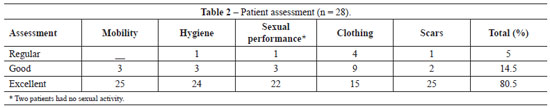
Assessment of satisfaction levels followed scoring criteria similar to those adopted by Bruschi et al.8. The results were assessed through a questionnaire considering aesthetic and functional criteria. The patients gave scores from 1 to 3 according to their satisfaction level: 1 for regular, 2 for good, and 3 for excellent. Result assessments are summarized in Table 2. Two patients did not reply to the question on sexual performance since they had no related activity. Thus, 138 grades were given by 28 patients.
Complications and Unexpected Events
The complications and unexpected events observed in this group of patients were considered inconsequential (Table 3). A small bruise drained spontaneously following incision and did not recur. Seromas observed in 6 patients were treated with puncture and did not relapse. Dehiscence cases were small, extended along suture lines, and were closed by second intention. Seven patients showing localized edema in the legs had a varicose component and were treated with proper exercise and elastic stockings. Hypertrophic and enlarged scars can occur via 3 mechanisms: first, early walking and corresponding tension over the suture line; second, through a longitudinal position of the surgical wound, which counteracts the force line of the thigh; and third, through gravitational traction over the scar on the inguinal fold. As requested and according to clinical progress, such scars will be reassessed later. Asymmetry was observed by the surgeons in 3 patients, but there were no patient complaints; therefore, this was deemed of minor relevance.
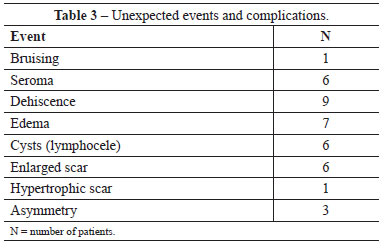
Lymphoceles diagnosed in 6 patients were confirmed by ultrasound imaging. They were treated with cyst removal, talc instillation, and sutures, leaving the remaining space to cystectomy.
DISCUSSION
Patients who experience massive weight loss usually show different and heterogeneous deformities throughout the body. The Pittsburgh scale classifies these deformities into several types according to the relevant body area and allows for routine therapy3.
According to such classification systems, the standardization proposed in this article enables surgeons to choose the most appropriate thigh lifting technique. The surgical techniques are established and widely used and, in this study, were indicated according to deformity type to obtain the most adequate result for each case4-7. Thus, in Group 1 patients, horizontal resection was performed next to the inguinal fold for the folds that had accumulated on the upper third; this required vertical suspension with significant improvement of the upper contour to smoothen the transition between the thighs and the pubic region (Figure 5).

Figure 5 - Patient from Group 1. In A, preoperative appearance, anterior view. In B, the dermal fatty excess in the superior portion of the medial side of the thigh. In C, preoperative marking in which the grayed area corresponds to the area where skin will be pushed back and fixated with non-absorbable thread. In D, positioning of the scar on the inguinal fold. In E, postoperative appearance, anterior view. In F, postoperative appearance, scar detail.
In Group 2 patients who showed fold accumulation in the upper third and part of the middle third of the thighs, resection next to the inguinal fold followed by a sickle-shaped resection in addition to a vertical suspension reduced the transverse direction of the thighs, markedly decreased the volume, and resulted in better definition of the transition between the thighs and the pubic region (Figure 6).

Figure 6 - Patient from Group 2. In A, preoperative appearance, anterior view. In B, preoperative marking detail (Lewis's technique). In C, postoperative appearance, anterior view. In D, postoperative appearance, detail of the scar on the medial aspect of the thigh.
Finally, in Group 3 patients, resection of a longitudinal spindle including the flaccid folds reduced the volume and created significant improvement in the contour of the thighs, which became plumper (Figure 7).

Figure 7 - Patient from Group 3. In A, preoperative marking, anterior view. In B, preoperative marking, posterior view. In C, postoperative appearance, anterior view in which improvement in the contour of the thighs is visible. In D, postoperative appearance, detail of the scar on the medial aspect of the thigh.
In patients who also underwent gluteal medial liposuction and resection, there was a clear reduction in the upper perimeter of the thigh, corroborating the results of an earlier study9.
All patients were classified as type 3 on the Pittsburgh scale, with the largest proportion of the sample falling within groups 2 and 3. This finding may be related to the large reduction in mean body mass index resulting from gastroplasty and the performance of the thigh lift, which resulted in a significant number of patients having skin folds of larger volume and quantity distributed throughout the thighs. In contrast, fewer patients were classified into Group 1, in which accumulation occurred in the upper third of the thigh. Although result assessment was not an aim of this study, its inclusion validates the use of the techniques suited to each dysmorphia type.
Among the 28 patients, regardless of the technique used, only 1 showed a regular degree of satisfaction to all inquired variables, whereas all other patients showed a high degree of satisfaction with the results obtained. Of the 6 patients with enlarged scars, only 4 graded the result as regular; this may not be compromising because scar enlargement and hypertrophy are considered unexpected events that arise from adverse biological factors. Since the sutures were performed without stress, such complications may be attributed to the recommended early walking because it exerts tension on the suture line and can result in scar enlargement. Such adverse outcomes in 5 cases may also be linked to the fact that incisions and subsequent sutures counteract the force lines of the thighs. In another patient, the scar located on the inguinal fold (after the use of Lockwood's technique) was subjected to gravitational traction aggravated by the thigh's own weight. It is important to stress that all patients were informed about the possibility of a more harmonic coxofemoral contour resulting in an unattractive scar.
For the use of long pants under clothing, the same patient showed a regular degree of satisfaction, repeating the same score for sexual performance, hygiene, and mobility variables. Consideration should be given to sexual performance, which is an extremely subjective factor. Despite psychological assessments, it is not possible to determine what patients expect to gain from the surgery; therefore, evaluations should be performed from obesity to thigh lift to determine whether variations in sexuality occur with more satisfactory or less satisfactory outcomes.
Hygiene and mobility factors depend exclusively on patients taking better care of themselves and being dedicated to physical exercises that favor body dynamics.
The incidence and type of complications and unexpected events encountered in this study are consistent with those reported in the literature. In fact, these complications arose from unknown adverse factors and therefore may simply be considered unexpected events4-7. These considerations justify the guidelines that allow for systematization and planning of surgeries according to the demands of each patient as well as the location, shape, and content of the dysmorphia.
Moreover, such planning and systematization leads to results that corroborate the criteria put forward by Ching et al.10 since the variables assessed in the postoperative period are simple, easy to evaluate, effective, reliable, and facilitate the identification of surgery-induced modifications. Therefore, the use of these criteria allows surgeons to assess improvement in quality of life and self-esteem of patients.
CONCLUSIONS
The guidelines proposed in this study are recommendable considering the heterogeneity in the topographic distribution of coxofemoral dysmorphia. Use of these guidelines will enable plastic surgeons to harmonize body contour and improve quality of life in formerly obese patients.
REFERENCES
1. Orpheu SC, Coltro PS, Scopel GP, Gomez DS, Rodrigues CJ, Modolin ML, et al. Collagen and elastic content of abdominal skin after surgical weight loss. Obes Surg. 2010;20(4):480-6.
2. Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87(6):1009-18.
3. Song AY, Jean RD, Hurwitz DJ, Fernstrom MH, Scott JS, Rubin JP. A classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale. Plast Reconstr Surg. 2005;116(5):1535-44.
4. Lockwood TE. Fascial anchoring technique in medial thigh lifts. Plast Reconstr Surg. 1998;82(2):299-304.
5. Lewis JR Jr. Correction of ptosis of the thighs: the thigh lift. Plast Reconstr Surg. 1966;37(6):494-8.
6. Cram AE, Aly AS. Lower extremity body contouring after massive weight loss. In: Aly A, ed. Body contouring after massive weight loss. St. Louis: Quality Medical Publishing; 2006. p. 213-36.
7. Baroudi R. Flankplasty: a specific treatment to improve body contouring. Ann Plast Surg. 1991;27(5):404-20.
8. Bruschi S, Datta G, Bocchiotti MA, Boriani F, Obbialero FD, Fraccalvieri M. Limb contouring after massive weight loss: functional rather than aesthetic improvement. Obes Surg. 2009;19(4):407-11.
9. Modolin MLA, Cintra Junior W, Gemperli R, Rocha RI, Lima e Silva E, Pares DFS, et al. Coxoplastias pós-cirurgia bariátrica: avaliação dos resultados. Rev Bras Cir Plást. 2011;26(3):512-7.
10. Ching S, Thoma A, McCabe RE, Antony MM. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111(1):469-80.
1. Ph.D. in Plastic Surgery by the Faculdade de Medicina da Universidade de São Paulo (Faculty of Medicine, University of São Paulo - FMUSP), assistant physician at the Plastic Surgery Department of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Clinics Hospital of the Faculty of Medicine, University of São Paulo - HCFMUSP) and Instituto de Assistência Médica ao Servidor Público Estadual (Institute of Medical Assistance to the State Public Service - IAMSPE), full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), São Paulo, SP, Brazil.
2. Assistant physician at the Plastic Surgery Department of the HCFMUSP, full member of the SBCP, São Paulo, SP, Brazil.
3. Resident physician at the Plastic Surgery Department of the HCFMUSP, São Paulo, SP, Brazil.
4. Associate professor of the Plastic Surgery Course at the FMUSP, full member of the SBCP, São Paulo, SP, Brazil.
5. Full professor of the Plastic Surgery Course at the FMUSP, full member of the SBCP, São Paulo, SP, Brazil.
Correspondence to:
Wilson Cintra Junior
Av. São Gabriel, 201 - conj. 704/5 - Itaim Bibi
São Paulo, SP, Brazil - CEP 01435-001
E-mail: wcintra@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 13, 2012
Article accepted: October 15, 2012
This study was performed at the Plastic Surgery Department of the Clinics Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital of the Faculty of Medicine, University of São Paulo), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter