

Original Article - Year 2012 - Volume 27 -
Crescent mastopexy with silicone implants: a longitudinal prospective study
Mastopexia crescente com implantes de silicone: um estudo longitudinal prospectivo
ABSTRACT
BACKGROUND: The combination of crescent periareolar mastopexy with breast augmentation is a well-described technique for the cosmetic improvement of breast ptosis classified as grades I and II, according to the Regnault grade scale. The aim of this study is to discuss the results obtained by the authors using a combination technique where the center of the round implants was positioned below the nipple projection.
METHODS: Grade I ptosis was corrected in certain patients by a combination of crescent periareolar mastopexy with breast augmentation using round-shaped, high-profile silicone gel implants. Each patient completed a questionnaire and rated the results obtained as poor, satisfactory, or good.
RESULTS: Were studied 128 patients who received silicone implants (average volume, 308 mL). The observed reoperations and complications rates were 9.4% and 8.6%, respectively. Eighty one (63.3%) patients responded to the questionnaire, and 58% considered the result good, 35.8% considered it satisfactory, and 6.2% considered it poor.
CONCLUSIONS: This study showed that this combination of techniques yields good results and low complication rates.
Keywords: Mammaplasty. Breast implants. Breast implantation. Silicone gels.
RESUMO
INTRODUÇÃO: Mastopexia periareolar crescente com aumento mamário é uma técnica bem descrita para correção de ptoses mamárias classificadas com graus I e II de Regnault. O objetivo deste estudo é discutir os resultados obtidos utilizando essa técnica, com posicionamento do centro de implantes redondos abaixo do mamilo.
MÉTODO: Ptoses de grau I foram corrigidas, em pacientes selecionadas, utilizando uma combinação de mastopexia crescente periareolar com aumento mamário utilizando implantes de gel de silicone redondos de perfil alto. As pacientes responderam a um questionário, classificando os resultados obtidos com a mamoplastia como pobres, satisfatórios ou bons.
RESULTADOS: Foram estudadas 128 pacientes, que receberam implantes de silicone com volume médio de 308 ml. Foram observadas taxas de reoperação e de complicação de 9,4% e 8,6%, respectivamente. Oitenta e uma (63,3%) pacientes responderam ao questionário, das quais 58% consideraram o resultado bom, 35,8% satisfatório e 6,2% pobre.
CONCLUSÕES: Este estudo demonstrou que essa combinação de técnicas proporciona bons resultados, com baixo índice de complicações.
Palavras-chave: Mamoplastia. Implantes de mama. Implante mamário. Géis de silicone.
The frequency of patients undergoing augmentation mammoplasty with silicone implants and mastopexy is increasing. Both breast hypoplasia and skin flaccidity may result in behavioral disturbances that affect self-esteem, and can lead to significant psychosocial changes and negative effects on quality of life1-3.
The correction of mild or moderate breast ptosis can be performed by increasing the volume using silicone implants, removing excess skin, or using both these techniques. The combination is considered more complex than either individual technique due to high rates of unsatisfactory results, recurrences, and complications associated with this procedure3,4.
The aim of this study is to evaluate the complications in and satisfaction of patients undergoing an upper crescent mastopexy technique where the center of the silicone breast implant was positioned below each nipple projection.
METHODS
A longitudinal prospective study was conducted between 2005 and 2010 that included patients undergoing breast augmentation due to hypomastia and breast ptosis.
The inclusion criteria were age, 16-70 years; presence of hypomastia or Regnault grade I ptosis; screening tests performed by patients; and the signing of an informed consent form. The exclusion criteria of this study were history of breast surgery, Regnault ptosis grades II or III, and depression.
All surgeries were performed under local anesthesia and sedation anesthesia using remifentanil and midazolam. The surgical technique consisted of an incision in the upper half of the transition line between the skin and the areola with an extension in the shape of a half-moon in the cranial portion of the areola skin, and the removal of 2 cm-3 cm of this skin in its largest longitudinal axis. Thereafter, a dissection was performed in the subglandular space for the placement of the breast implants. The breast tissue was approximated with single stitches inverted (Halsted) using 4-0 nylon, whereas the periareolar suture was made with stiches in a horizontal U (Wolf) fashion with 5-0 nylon sutures. The surgical protocol is shown in Figure 1.

Figure 1 - The presented surgical technique.
Between 2 months and 6 months postoperatively, the patients completed a questionnaire and rated the results obtained with the mammoplasty as poor, satisfactory, or good. The complication rates were also recorded. The data are presented in the form of arithmetic average and frequency.
RESULTS
From June 2005 to December 2010, 128 patients underwent the upper crescent mastopexy technique where the center of the silicone breast implant was positioned below the nipple projection. All patients were Caucasian, 6.3% were smokers, and 39% had a history of pregnancy prior to the operation. The average implant volume was 308 mL (range, 200 mL - 425 mL). The mean age was 25 years (range, 16-51 years).
Figures 2 and 3 illustrate satisfactory and unsatisfactory results using this technique, respectively. Complications were observed in 11 (8.6%) patients, including 5 (3.9%) with partial dehiscence, 2 (1.6%) with seroma, 1 (0.8%) with a hypertrophic scar, 1 (0.8%) with contracture, 1 (0.8%) with dehiscence as well as seroma, and 1 (0.8%) with extrusion of dehiscence.
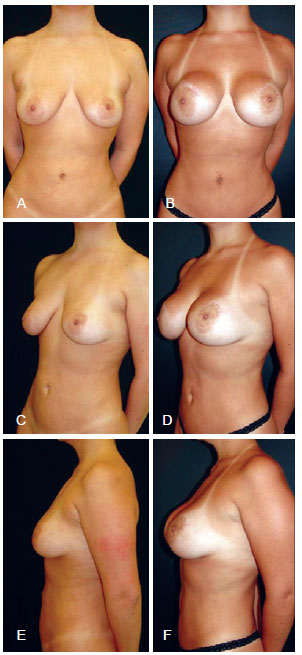
Figure 2 - Unsatisfactory results requiring further surgery. In A, C, and E, preoperative image of the anterior, left oblique, and left view profiles, respectively. In B, D, and F, postoperative image of the anterior, left oblique, and left view profiles, respectively.
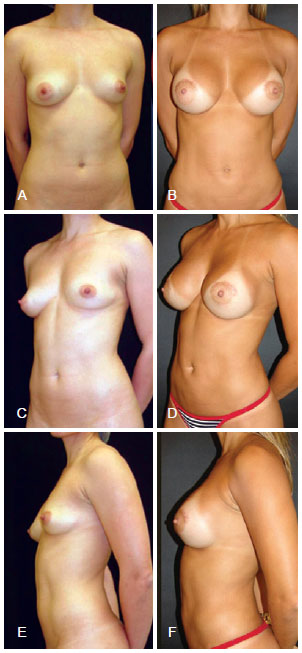
Figure 3 - Satisfactory results. In A, C, and E, preoperative image of the anterior, left oblique, and left view profiles, respectively. In B, D, and F, postoperative image of the anterior, left oblique, and left view profiles, respectively.
Among all the patients, 12 (9.4%) additional surgeries were required, including 8 (6.3%) minor scar revisions, 3 (2.3%) mastopexies with inverted T-shaped scars, and 1 (0.8%) explantation.
Eighty-one (63.3%) patients completed the questionnaire. The results obtained from the operation were rated good by 47 (58%), satisfactory by 29 (35.8%), and poor by 5 (6.2%) patients.
DISCUSSION
A study on mastopexy, in which 487 members of the American Society for Aesthetic Plastic Surgery (ASAPS) participated, revealed that techniques resulting in inverted T-shaped scars were the most frequent procedures performed by the participants, although techniques with reduced scarring have become more popular since 2000. The techniques that involve the creation of the inverted T-shape scar are associated with excessive scarring as well as an increase in the distance between the papillary-areolar complex and the submammary groove, due to the greater flaccidity of that area caused by the weight of the prosthesis. The patients who underwent periareolar techniques frequently required additional surgeries, and these procedures were associated with the lowest rate of satisfaction among surgeons5. These data justify the reoperation rate observed in this study.
In patients with a high degree of ptosis, treatment with techniques that result in periareolar, vertical, or inverted T-shaped scars is mandatory. Periareolar mammoplasty techniques generally remove a smaller amount of skin as compared to those resulting in T-shaped, L-shaped, or even vertical scars. This fact limits the indication of this technique to cases with very large breasts, particularly in those patients with high degrees of skin flaccidity. However, in cases of mild ptosis, techniques that produce smaller scars and treat skin flaccidity by increasing volume can be used1,6-8.
In 1923, Aubert9 published the first report of mammoplasty with elevation of the papillary-areolar complex. Since then, several articles have been published on the use of nipple elevation, with or without the simultaneous use of silicone implants. The complications cited in the reviewed articles included persistence or early recurrence of ptosis, keloids, hypertrophic and hypotrophic scars, flattening of the breast cone, loss of sensation in the areola, areolar malposition, infection, distortion of the areolar shape, flattening of the nipple, hematomas, and seromas8,10,11. This paper presented complication rates similar to those observed in the literature.
The degree of postoperative patient satisfaction is closely related to surgical success. The implant size and technique used are known to be dependent on both the patient and the surgeon. In the present study, most patients considered their results good. Undoubtedly, surgical planning and perfect patient understanding of the limitations of the available techniques are essential for the execution of a technique with reduced scarring12.
In 1985, Puckett et al.13 described a technique of crescent mastopexy. The main limitation of this technique is that it raises the papillary-areolar complex by approximately 2 cm, thus limiting its use. The major problem of this technique consists of the formation of scars > 5 mm wide and the modification of the aspect of the areola to a more oval shape14,15. This fact justifies the use, in this study, of the presented technique in cases of mild ptosis only.
High-profile implants are useful in patients who desire a breast volume that exceeds the diameter of the base of their natural breasts. The main disadvantages of this technique are the low mobility of the implant and the formation of a less obtuse transition between the upper portion of the breast and the chest, as compared to implants with moderate or low profiles. The implants used in periareolar mastopexy can provide a more conical shape to the breast; therefore, in the present study, we chose to position the center of the implant below the nipple projection to create gentle breast elevation and lower the submammary groove to complement the treatment of ptosis16.
CONCLUSIONS
This study indicated that the technique of crescent mastopexy where the center of the silicone breast implant was positioned below the nipple projection yields good results and low complication rates.
REFERENCES
1. Aboudib JH. Avaliação tardia dos resultados das mamoplastias por via periareolar. Rev Soc Bras Cir Plást. 2004;19(3):21-30.
2. Saldanha OR, Maloof RG, Dutra RT, Luz OAL, Saldanha Filho O, Saldanha CB. Mamaplastia redutora com implante de silicone. Rev Bras Cir Plást. 2010;25(2):317-24.
3. Parsa AA, Jackowe DJ, Parsa FD. A new algorithm for breast mastopexy/augmentation. Plast Reconstr Surg. 2010;125(2):75e-77e.
4. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67.
5. Rohrich RJ, Gosman AA, Brown SA, Reisch J. Mastopexy preferences: a survey of board-certified plastic surgeons. Plast Reconstr Surg. 2006;118(7):1631-8.
6. Mansur JRB, Bozola AR. Mastopexia e aumento das mamas com proteção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24(3):304-9.
7. Rinker B, Veneracion M, Walsh CP. Breast ptosis: causes and cure. Ann Plast Surg. 2010;64(5):579-84.
8. Spear SL, Dayan JH, Clemens MW. Augmentation mastopexy. Clin Plast Surg. 2009;36(1):105-15.
9. Aubert V. Hypertrophie mammaire de la puberté. Arch Fr Belg Chir. 1923;3:284-9.
10. Gruber R, Denkler K, Hvistendahl Y. Extended crescent mastopexy with augmentation. Aesthetic Plast Surg. 2006;30(3):69-74.
11. García Velasco M, Arizti P, García Toca R. Surgical correction of the "small" postpartum ptotic breast. Aesthet Surg J. 2004;24(3):199-205.
12. Adams WP Jr, Teitelbaum S, Bengtson BP, Jewell ML, Tebbetts J, Spear S. Breast augmentation roundtable. Plast Reconstr Surg. 2006;118(7 Suppl):175S-87S.
13. Puckett CL, Meyer VH, Reinisch JF. Crescent mastopexy and augmentation. Plast Reconstr Surg. 1985;75(4):533-43.
14. Nigro DM. Crescent mastopexy and augmentation. Plast Reconstr Surg. 1985;76(5):802-3.
15. Snow JW. Crescent mastopexy and augmentation. Plast Reconstr Surg. 1986;77(1):161-2.
16. Baxter RA. Indications and practical applications for high-profile saline breast implants. Aesthet Surg J. 2004;24(1):24-7.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Plastic Surgery Society, Porto Alegre, RS, Brazil.
2. Physician, Dermatology postgraduate, Porto Alegre, RS, Brazil.
Correspondence to:
Denis Souto Valente
Rua Veríssimo do Amaral, 580 - ap. 1706
Porto Alegre, RS, Brazil - CEP 91360-470
E-mail: denisvalente@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 12, 2012
Article accepted: October 5, 2012
This study was performed at the Department of Plastic Surgery, Hospital Mãe de Deus, Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter