

Original Article - Year2012 - Volume27 - Issue 3
Autologous periorbital fat grafting in facial rejuvenation: a retrospective analysis of efficacy and safety in 31 cases
Lipoenxertia periorbitária no rejuvenescimento facial: análise retrospectiva da eficácia e da segurança em 31 casos
ABSTRACT
BACKGROUND: Periorbital and zygomatic hollows as well as flaccid cheeks are among the most evident characteristics of aging or facial disharmony. Volume replacement is a simple and efficient procedure, and fat grafting is considered as the best treatment for these characteristics. This study evaluates 31 patients who underwent autologous fat grafting and emphasizes the safety and efficacy of this procedure.
METHODS: A retrospective analysis of 31 consecutive patients who underwent periorbital and zygomatic fat grafting, alone or in combination with other cosmetic procedures, was carried out. Final evaluation was performed by assessing pre- and postoperative photographs as well as the degree of patient satisfaction.
RESULTS: Of 31 patients, 26 (83.9%) reported excellent postoperative outcomes; 3 (9.7%), satisfactory outcomes; and 2 (6.4%), poor outcomes. According to the authors' evaluation, 24 (77.5%) patients had excellent outcomes, 5 (16.1%) had satisfactory outcomes, and 2 (6.4%) had poor outcomes. Retouching of the fat graft was recommended for only 4 patients. The complications observed were minimal and transient.
CONCLUSIONS: Facial fat grafting is a simple and effective procedure that presents minimal complications when performed by skilled surgeons.
Keywords: Transplantation, autologous. Lipectomy. Orbit. Face. Rejuvenation.
RESUMO
INTRODUÇÃO: Os sulcos periorbitários e zigomático e o malar flácido estão entre as características mais marcantes de envelhecimento ou de desarmonia facial. A reposição do volume é um método simples e eficiente, e o lipoenxerto pode ser o melhor material. O presente trabalho traz uma análise de 31 pacientes submetidos a autolipoenxertia, com ênfase na eficácia e na segurança da técnica.
MÉTODO: Análise retrospectiva de 31 pacientes consecutivos, submetidos a lipoenxertias periorbitária e malar, concomitantemente ou não a outros procedimentos estéticos. A avaliação foi feita por meio de comparação entre fotografias pré e pós-operatória, bem como pelo grau de satisfação dos pacientes.
RESULTADOS: Dos 31 pacientes, 26 (83,9%) classificaram o resultado pós-operatório como ótimo, 3 (9,7%), bom, e 2 (6,4%), regular. Na avaliação dos autores, 24 (77,5%) pacientes apresentaram resultado ótimo, 5 (16,1%), bom, e 2 (6,4%), regular. Houve necessidade de retoque de lipoenxertia em apenas 4 pacientes, por sugestão do cirurgião. As complicações foram mínimas e passageiras.
CONCLUSÕES: A lipoenxertia facial é fácil e eficaz, e as complicações são mínimas quando realizada por cirurgiões qualificados.
Palavras-chave: Transplante autólogo. Lipectomia. Órbita. Face. Rejuvenescimento.
One of the typical signs of beauty and youth is an apple-shaped face that is uniform, smooth, and in continuity with the inferior periorbital region. Major periorbital abnormalities involve a deeper orbital cavity, in which the orbital rim and midface depression are V-shaped and extend medially along the nasojugal groove as well as laterally to the orbital hollow in a palpebral-malar direction and to the zygomatic hollow in a zygomatic-malar direction, which obliquely divides the malar region1-5. The presence of fat bags may cause midface bulging. Moreover, the skin is usually darker in this region, an effect that highlights deformities even further (Figure 1). These abnormalities may be personal, that is, they may have been present in the individual since childhood and youth. However, they may also be the result of aging or iatrogenic causes such as the excessive withdrawal of fat bags during blepharoplasty.
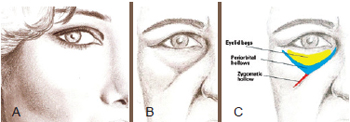
Figure 1 - In A, standards for youth and beauty. In B and C, periorbital and malar deformities, including periorbital and zygomatic hollows as well as eyelid bags.
During midface aging, these structures do not change (or "sag") because of the effects of gravity, but rather are altered by qualitative skin changes, volumetric redistribution of facial fat compartments (hypotrophy and hypertrophy), and continuous remodeling of the craniofacial bones6-13. The aim of the procedure proposed in the current report is to redistribute facial soft tissue volumes and replace eyelid fat bags according to the requirements of the patient14,15. Periorbital volume replacement may be performed using different midface suspensions, alloplastic implants1-4,16, or autogenous fat grafting. This study evaluates 31 patients who underwent autogenous fat grafting and emphasizes the safety and the efficacy of this procedure.
METHODS
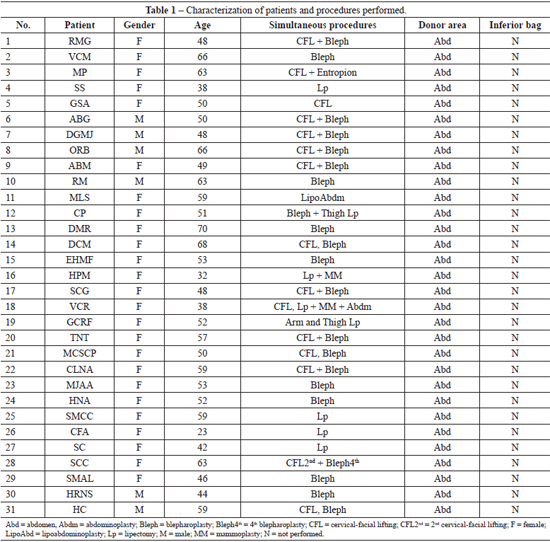
From January 2010 to January 2012, periorbital and malar fat grafting was performed for 31 consecutive patients, of whom 25 were women aged between 23 and 70 years (average age, 52.2 years; Table 1).
Local anesthesia was used when periorbital fat grafting was performed alone or in combination with blepharoplasty. General anesthesia was administered when this procedure was performed in combination with other surgeries.
Facial fat grafting was recommended for patients with deep periorbital and zygomatic hollows, presenting with or without malar deflation. The total volume and the volumes corresponding to the different areas treated were not measured. The patients and authors carried out a subjective assessment by comparing photographs obtained before and 4-8 months after surgery. The degree of patient satisfaction was classified as excellent, satisfactory, poor, or unsatisfactory. The authors considered the following parameters to assess patient outcomes: volume, skin integrity, and firmness of the esthetical unit. This assessment was used to classify the results as excellent, satisfactory, poor, or unsatisfactory.
All patients were informed about the risk of volume loss up to 6 months after surgery and were told that the volume grafted may vary according to fluctuations in their weight. Moreover, the patients were informed that a worsening of pre-existing hyperchromia may also be observed.
Surgical Technique
Evaluation was performed with the patient in an orthostatic position. Areas of depression were delimited.
If projection of the lower eyelid bag exceeded the inferior orbital rim, lower cutaneous blepharoplasty was performed with the pinch method17, involving a dilatation of approximately 3 mm in length of the preorbital orbicularis oculi muscle. The fat bag was resected to the level of the orbital rim and malar folds (Figure 2). When the inferior bag did not project beyond the orbital rim, the surrounding depression was filled and leveled with fat grafting.
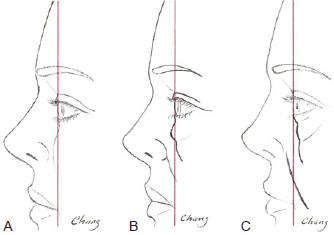
Figure 2 - In A, desirable features: inferior palpebral region leveled to the orbit and slight malar projection. In B, eyelid protrusion and malar retraction: requires resection of the eyelid bag until flatness is achieved and malar fat grafting. In C, detached eyelid bag, with no protrusion except in the orbit: requires periorbital and malar fat grafting with no eyelid bag resection.
In combined surgeries, facial fat grafting was the first procedure performed, before the appearance of edema; this may have affected the injections.
The donor area was chosen according to the preference of the patient, local fat abundance, and ease of access. The lipoaspirate was removed with negative pressure using a 60-mL syringe with a catheter tip and cannula, which had a 3-mm internal diameter and 3 side holes in series localized at the distal tip.
In patients undergoing general anesthesia, fat was suctioned without prior infiltration of any solution. In patients who received local anesthesia, 0.5% lidocaine and 1:160,000 epinephrine were infiltrated uniformly in a proportion of 1:1. In the receiving area, trunk block of the infraorbital nerve was performed using the minimum possible volume of anesthetics and vasopressors.
The lipoaspirate was decanted without the addition of any solution until the appearance of 3 phases. The upper and lower layers, formed mostly by oil and red blood cells, respectively, were discarded, whereas the middle layer was transferred into 1-mL syringes.
Lipoaspirate injection in previously defined areas was performed through retroinjections using a microcannula (Figures 3 and 4). A small amount of lipoaspirate was injected deeply into the face. The more superficial layers were then progressively treated until the skin was homogenously injected. The minimum amount of pressure possible was applied to the plunger of the syringe, and if any resistance was encountered, the injection was discontinued. In cases where this occurred, a new syringe and microcannula were used, because these instruments may have been obstructed by globules larger than the microcannula itself. Maximum care was taken to prevent complications due to the injections; these complications are encountered mainly in the superficial layers and usually lead to irreversible effects. A proper three-dimensional distribution of the graft is required to avoid excessive local tension. Over-correction of the periorbital area should not be performed, as retouching of the fat graft can be carried out 6 months after the initial procedure.
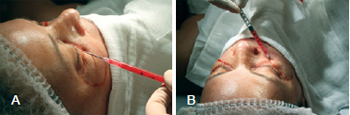
Figure 3 - In A, filling of the nasojugal groove. In B, filling of the periorbital hollow.
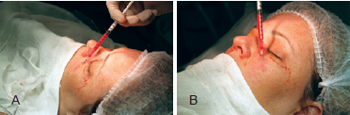
Figure 4 - In A, filling of the zygomatic and malar region. In B, filling of the malar region.
RESULTS
Of the 31 patients, 26 (83.9%) classified their postoperative outcomes as excellent; 3 (9.7%), as satisfactory; and 2 (6.4%), as unsatisfactory (Table 2). The authors evaluated the outcome of 24 (77.5%) patients as excellent; 5 (16.1%), as satisfactory; and 2 (6.4%), as unsatisfactory.
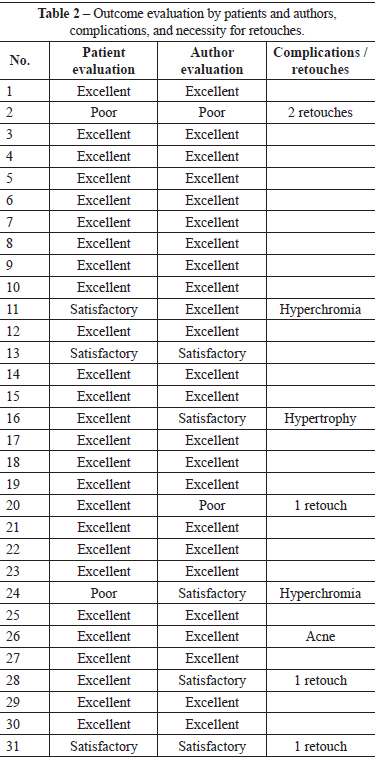
Figures 5 to 9 illustrate cases in this series.
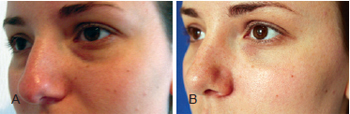
Figure 5 - Twenty-three-year-old patient who underwent periorbital and malar autologous fat grafting. In A, appearance before surgery. In B, appearance 6 months after surgery.
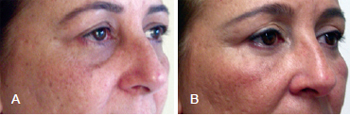
Figure 6 - Fifty-one-year-old patient who underwent periorbital and malar fat grafting combined with blepharoplasty. In A, appearance before surgery. In B, appearance 14 months after surgery.
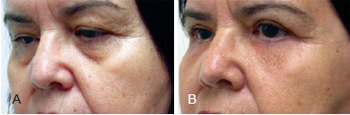
Figure 7 - Forty-six-year-old patient who underwent periorbital and malar fat grafting combined with blepharoplasty. In A, appearance before surgery. In B, appearance 4 months after surgery.
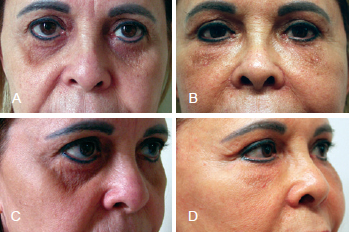
Figure 8 - Forty-eight-year-old patient with iatrogenic periorbital depression that developed after undergoing blepharoplasty for the third time. She underwent secondary cervical-facial lifting combined with periorbital and malar fat grafting. In A and C, appearance before surgery. In B and D, appearance 6 months after surgery.
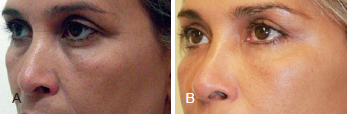
Figure 9 - Forty-eight-year-old patient treated with cervical-facial lifting combined with blepharoplasty as well as periorbital and malar fat grafting. In A, appearance before surgery. In B, appearance 14 months after surgery.
Edema and ecchymosis resolved completely after 3 to 4 weeks. Two patients showed worsening of pre-existing hyperchromia in the lower eyelid, which required dermatologic treatment for up to 4 months. Due to personal reasons, one patient returned for surgery revision 15 months after the initial procedure. This patient had gained 12 kg in weight because of a history of pregnancy and suffered from fat graft hypertrophy (Figure 10). Finally, a 23-year-old patient developed acne on her face. Four patients underwent small retouches as recommended by the surgeon and were satisfied with the final outcome of the procedure.
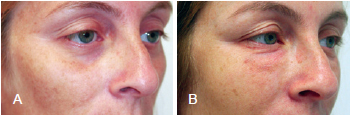
Figure 10 - Thirty-two-year-old patient. In A, appearance before surgery. In B, appearance 15 months after surgery. The patient gained 12 kg in weight due to a pregnancy that occurred after the procedure and shows fat graft hypertrophy.
DISCUSSION
In this retrospective study, the injected volume and volume maintenance were not measured. Efficiency was evaluated subjectively, according to the degree of satisfaction of both the patients and the surgeon. The safety of the procedure was assessed on the basis of the complication rate observed.
The volume of the fat graft stabilized approximately 4 months after surgery. The patients' evaluations were influenced to a greater extent by development of hyperchromia than by graft volume, whereas the authors assessed the results taking into consideration the overall consistency of the esthetic unit.
Further comparative analyses of patient outcomes considering gender, age, or body mass index were not performed because of the small cohort analyzed. However, esthetic outcomes were fairly reproducible, and the technique presented a low complication rate. These results are in agreement with those published in the literature18,19. Interestingly, acne developed in a young patient, as already reported by other authors18,19.
Pseudoptosis is a mechanism of midface aging that occurs via the absence or loss of volume of the deep medial cheek compartment9. The periorbital and zygomatic hollows as well as midface volume are typical characteristics of an individual's face. Accentuated by aging, these features can undergo bone remodeling, skin thinning, and atrophy of fat compartments. The absence of volume may not be easily or effectively corrected with blepharoplasty or rhytidoplasties. Filling of these areas with extra volume is a simple and effective technique that may be performed using alloplastic materials or autotransplantation of lipoaspirate14,15.
Fat grafting procedures have been refined and are now commonly used, in particular since the roles of mesenchymal cells, which are abundant in the fat tissue, have been assessed20. However, this procedure is invasive and requires a steep learning curve. Moreover, maintenance of the initial volume injected21 is unpredictable, and further grafting may be required.
The advantages of fat grafting are the absence of formation of foreign body granulomas or biofilms22; the possibility of injection in all layers; the abundance of transferred material, which enables the use of larger volumes and ensures a better distribution; and efficient tissue integration, which guarantees a natural and complete result.
Nowadays, the ability of fat grafting to regenerate or rejuvenate the skin is being investigated23. However, the injection of lipoaspirate is not simple as it requires a larger caliber cannula. Moreover, because the consistency of lipoaspirate is not homogenous, the outcome of this technique is dictated by lipoaspirate concentration, the presence of larger fat globules, and the potential complications encountered24. Nevertheless, when performed by skilled surgeons, fat grafting is a safe procedure and may replace or complement major midface surgeries.
CONCLUSIONS
This study demonstrated the high esthetic efficacy of fat grafting performed in periorbital regions, as assessed by distribution and volume maintenance. The low complication rate found is in agreement with findings reported in the literature.
Periorbital and midface volume replacement are specific procedures that cannot be replaced by major surgeries such as blepharoplasty or rhytidectomy when considering practicality and efficacy. No complications associated with alloplastic materials were observed when using autogenous fat grafts in the current study. Complications that do arise can be easily minimized or avoided with training.
REFERENCES
1. Goldberg RA. The three periorbital hollows: a paradigm for periorbital rejuvenation. Plast Reconstr Surg. 2005;116(6):1796-804.
2. Yaremchuk MJ, Kahn DM. Periorbital skeletal augmentation to improve blepharoplasty and midfacial results. Plast Reconstr Surg. 2009;124(6):2151-60.
3. Hirmand H. Anatomy and nonsurgical correction of the tear trough deformity. Plast Reconstr Surg. 2010;125(2):699-708.
4. Yaremchuk MJ. Infraorbital rim augmentation. Plast Reconstr Surg. 2001;107(6):1585-95.
5. Pessa JE, Desvigne LD, Lambros VS, Nimerick J, Sugunan B, Zadoo VP. Changes in ocular globe-to-orbital rim position with age: implications for aesthetic blepharoplasty of the lower eyelids. Aesthetic Plast Surg. 1999;23(5):337-42.
6. Donofrio LM. Fat distribution: a morphologic study of the aging face. Dermatol Surg. 2000;26(12):12:1107-12.
7. Lambros V. Observations on periorbital and midface aging. Plast Reconstr Surg. 2007;120(5):1367-77.
8. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219-31.
9. Rohrich RJ, Pessa JE, Ristow B. The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg. 2008;121(6):2107-12.
10. Pessa JE. An algorithm of facial aging: verification of Lambro's theory by three-dimensional stereolithography, with reference to the pathogenesis of midfacial aging, scleral show, and the lateral suborbital trough deformity. Plast Reconstr Surg. 2000;106(2):479-90.
11. Pessa JE, Chen Y. Curve analysis of the aging orbital aperture. Plast Reconstr Surg. 2002;109(2):751-60.
12. Shaw Jr RB, Kahn MD. Aging of the midface bony elements: a threedimensional computed tomographic study. Plast Reconstr Surg. 2007;119(2):675-83.
13. Mendelson BC, Hartley W, Scott M, McNab A, Granzow JW. Age-related changes of the orbit and midcheek and the implications for facial rejuvenation. Aesthetic Plast Surg. 2007;31(5):419-23.
14. Trepsat F. Periorbital rejuvenation combining fat grafting and blepharoplasties. Aesthetic Plast Surg. 2003;27(4):243-53.
15. Trepsat F. Midface reshaping with micro-fat grafting. Ann Chir Plast Esthet. 2009;54(5):435-43.
16. O'Hara KL, Urrego AF, Garri JI, O'Hara CM, Bradley JP, Kawamoto HK. Improved malar projection with transconjunctival hydroxyapatite granules. Plast Reconstr Surg. 2006;117(6):1956-63.
17. Rosenfield LK. The pinch blepharoplasty revisited. Plast Reconstr Surg. 2005;115(5):1405-14.
18. Kim SM, Kim YS, Hong JW, Roh TS, Rah DK. An analysis of the experiences of 62 patients with moderate complications after full-face fat injection for augmentation. Plast Reconstr Surg. 2012;129(6):1359-68.
19. Grahovac TL, Rubin JP. An analysis of the experiences of 62 patients with moderate complications after full-face fat injection for augmentation. Plast Reconstr Surg. 2012;129(6):1369-70.
20. Lu F, Li J, Gao J, Ogawa R, Ou C, Yang B, et al. Improvement of the survival of human autologous fat transplantation by using VEGF-transfected adipose-derived stem cells. Plast Reconstr Surg. 2009;124(5):1437-46.
21. Swanson E. Malar augmentation assessed by magnetic resonance imaging in patients after face lift and fat injection. Plast Reconstr Surg. 2011;127(5):2057-65.
22. Mojallal A, Lequeux C, Shipkov C, Breton P, Foyatier JL, Brayer F, et al. Improvement of skin quality after fat grafting: clinical observation and an animal study. Plast Reconstr Surg. 2009;124(3):765-74.
23. Rohrich RJ, Monheit G, Nguyen AT, Brown SA, Fagien S. Soft-tissue filler complications: the important role of biofilms. Plast Reconstr Surg. 2010;125(4):1250-6.
24. Lazzeri D, Agostini T, Figus M, Nardi M, Pantaloni M, Lazzeri S. Blindness following cosmetic injections of the face. Plast Reconstr Surg. 2012;129(4):995-1012.
1. Full Member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), member of the Sociedade Brasileira de Microcirurgia Reconstrutiva/Brazilian Society of Reconstructive Microsurgery, surgeon at the Reconstructive Microsurgery Department of the Hospital dos Servidores do Estado do Rio de Janeiro, surgeon at the Plastic Surgery Department of the Hospital Federal do Andaraí do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
2. Aspirant member in training of the SBCP, resident physician at the Plastic Surgery Department of the Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil.
Correspondence to:
Chang Yung Chia
Av. Lúcio Costa, 3360 - bloco 8 - ap. 2402 - Barra da Tijuca
Rio de Janeiro, RJ, Brazil - CEP 22630-010
E-mail: changplastica@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 5, 2012
Article accepted: August 21, 2012
This study was performed at the Plastic Surgery Department of the Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter