

Original Article - Year 2012 - Volume 27 - Issue 3
Temporofrontal galea periosteal lifting with double access: a conservative procedure
Suspensão temporofrontal gálea-periostal com duplo acesso: tática conservadora
ABSTRACT
BACKGROUND: Surgical treatment of the superior third of the face should usually involve an extensive area, including the frontal and temporal regions. However, the open coronal technique has been avoided because it carries a risk of potential complications and a wide scar. The technique has been supplanted by endoscopic and other less-invasive techniques, which are perhaps less efficacious. This article proposes an open technique that maintains the coronal lifting efficiency without its typical complications.
METHODS: A retrospective analysis of 20 consecutive female patients who underwent cervicofacial facelift from February 2008 to July 2011 was performed. The patients had a mean age of 53.3 years (range, 46-71 years). The sensitivity of the regions covered (i.e., anesthesia, hypoesthesia, hyperesthesia, paresthesia), motor function of the temporal branch of the facial nerve (i.e., frontal muscle movement), and healing (i.e., widening and alopecia) were evaluated.
RESULTS: There were no sensory, motor, or vascular complications. Moreover, neither cicatricial enlargement nor alopecia was observed. One patient required revision of the corrugator muscle myectomy, and another underwent myectomy of the lateral orbicularis muscle of the eye for optimal results.
CONCLUSIONS: The proposed technique is simple, safe, does not require special equipment or devices, and has the advantage of wide and harmonious distribution of the flap, including the temporal and frontal regions.
Keywords: Rhytidoplasty. Face/surgery. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: O tratamento do terço superior da face deve ser amplo, englobando as regiões frontal e temporal. Entretanto, em decorrência das potenciais complicações e da cicatriz extensa, o lifting coronal tem sido evitado e substituído por técnica endoscópica e procedimentos menos invasivos, porém, talvez, menos eficazes. O objetivo deste estudo é propor uma tática cirúrgica com eficácia similar à do lifting coronal, sem, no entanto, as complicações típicas desse procedimento.
MÉTODO: Foi realizada análise retrospectiva de 20 pacientes do sexo feminino, consecutivas, com média de idade de 53,3 anos, submetidas a lifting cervicofacial, no período de fevereiro de 2008 a julho de 2011. Foram avaliadas a sensibilidade da região abordada (anestesia, hipoestesia, hiperestesia, parestesia), a função motora do ramo temporal do nervo facial (movimento do músculo frontal), e a cicatrização (alargamento e alopecias).
RESULTADOS: Não houve complicações sensitivas ou motoras, bem como vasculares. Também não foram observados alargamento cicatricial ou alopecias. Uma paciente precisou de revisão da miectomia dos músculos corrugadores e outra foi submetida a miectomia do músculo orbicular lateral do olho, para otimização do resultado.
CONCLUSÕES: A tática é segura, simples, não necessita de equipamentos ou materiais especiais, e tem a vantagem da ampla e boa distribuição cutânea, englobando as regiões frontal e temporal.
Palavras-chave: Ritidoplastia. Face/cirurgia. Cirurgia plástica/métodos.
Because of potential complications, coronal lifting1,2 has been abandoned and replaced by less-invasive procedures3,4, including botulinum toxin administration or isolated brow lift techniques.
In untreated facial rhytidoplasties of the temporal region, after superolateral traction of the facial flap, excess skin accumulates in the region of the zygomatic arch, causing incomplete and unsatisfactory results.
The upper face includes the frontal and temporal regions; their "block" treatment is fundamental in the cervicofacial lifting and in the blepharoplasties3,5. The extensive scar of the coronal facelift is less attractive to patients than that from techniques that result in reduced scars3,4 including endoscopic lifting6-13. However, the extensive scar allows better distribution of the skin flap and excision of the remaining skin; in addition, its design may vary according to a patient's need, such as a pre-capillary design in patients with a high forehead.
The anatomy of this region is complex. Moreover, there is an apparent lack of a simple technique with consistent fixation14 that can avoid complications such as frontal muscle paralysis, sensory disturbances of the scalp, enlargement of scars, and alopecia1,2,10,11.
In this report, we review the anatomy of the temporofrontal region, propose a new surgical technique, and discuss the results obtained with temporofrontal galea periosteal lifting with dual access.
METHODS
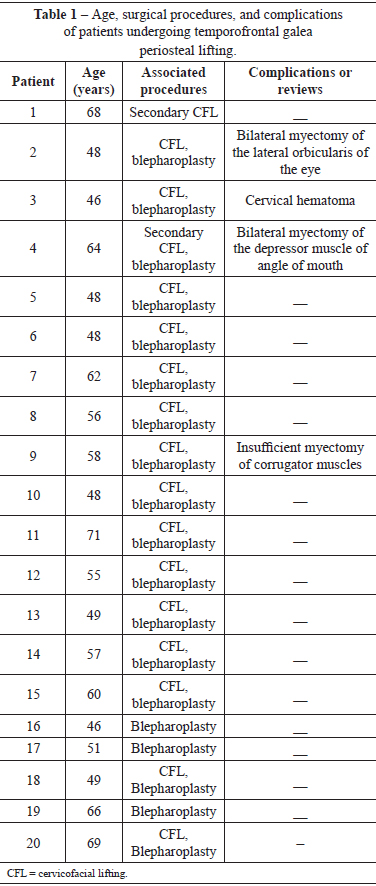
A retrospective analysis including 20 consecutive female patients with a mean age of 53.3 years (range, 46-71 years) who underwent cervicofacial lifting from February 2008 to July 2011 was performed. The cervicofacial lifting was primary and secondary in 18 and 2 patients, respectively (Table 1).
The inclusion criteria were as follows: female gender, no baldness issues, cervicofacial flaccidity, and excess skin in the temporofacial region.
The sensitivities of the frontal and parietal regions were evaluated, considering the integrity of the medial and lateral branches, supraorbital nerve, branches of the supratrochlear nerve, frontalis and corrugator muscle movements, and the coronal scar.
The frontalis muscle movements were assessed by requesting the patient to lift the supercilia. Symmetry and range of motion were analyzed. The coronal scar was evaluated, focusing on alopecia and its width. Sensitivity was tested with a digital touch and pressure sensor with a sharp object in the frontal region and scalp and compared to other regions of the body where sensitivity was unchanged. The presence of paresthesia was also evaluated.
Surgical Anatomy
The temporoparietal fascia, also known as superficial temporal fascia, contains the auricularis anterior muscle and is the continuation of the temporal region of the superficial muscular aponeurotic system (SMAS) of the face. It is frontally contiguous with the frontal muscle plane, galea aponeurotica, and subgaleal plane. The superficial and deep temporal fascia, which cover the temporalis muscle, medially fuse with the periosteum in the crista temporalis, which is contiguous with the periosteum in the frontal region.
Knize15 divides the superficial temporal fascia into 3 layers. The most superficial layer, layer I, is thick and continues medially in the forehead as the epicranial aponeurosis, top layer of the galea aponeurotica, and frontalis muscle. The thin intermediate and deep layers, layers II and III of the superficial temporal fascia, respectively, are contiguous medially in the forehead "subplane" of the epicranial aponeurosis - the deepest layer of the galea. The zone where these planes unite is approximately 6 mm wide and medial to the temporal crest. The orbital ligament is a band of connective tissue that secures the temporal fascia to the bone, caudal end of the anchoring zone, and lateral-upper corner of the orbit16. The temporal branch of the facial nerve is located on the bottom surface of the thick layer of layer I and enters the frontalis muscle medially. Deep dissection close to the temporalis fascia avoids injury to the temporal branch of the facial nerve.
The sensitivity of the frontal region is mediated by the supratrochlear and supraorbital nerve branches of the frontal nerve, which in turn is a branch of the ophthalmic nerve, which is a division of the trigeminal nerve. More medially, the supratrochlear nerve emerges from the orbit via a notch on the orbital rim, pierces the corrugator muscle on its medial side, and provides sensitivity to the middle part of the forehead. The supraorbital nerve usually exits via the supraorbital foramen bone in the medial orbital rim and branches into a medial or superficial branch and a lateral or deep branch. The medial branch crosses and runs superficially over the frontal muscle, supplying the rest of the frontal region and the anterior part of the scalp. The side branch lateralizes, traveling on the periosteum 1 cm medial and parallel to the temporal crest and enters the galea in the cranial portion of the forehead, providing sensitivity to the parietal region16-18 (Figures 1 and 2).

Figure 1 - Sensory area and nerve pathway. 1 = supratrochlear nerve, sensory area in blue; 2 = medial branch of the supraorbital nerve, sensory area in green; 3 = lateral branch of the supraorbital nerve, sensory area in orange; 4 = temporal branch of the facial nerve; 5 = temporal crest.

Figure 2 - Relationships between the nerves and anatomical planes. 1 = temporal branch of the facial nerve; 2 = supraorbital nerve; 3 = medial branch of the supraorbital nerve; 4 = lateral branch of the supraorbital nerve; 5 = periosteum; 6 = deep temporal fascia, contiguous with the medial periosteum to the temporal crest; 7 = layers II and III of the superficial temporal fascia, which continue in the medial subplane; 8 = I layer of the superficial temporal fascia, which continues medially as the aponeurotic galea; 9 = temporalis muscle.
Medial to the temporal crest in the frontoparietal region, a transverse incision in the galea will inevitably sever the lateral supraorbital nerve (Figure 3). Similarly, subgaleal dissection in the superior and caudal orbital rim over the forehead may damage the nerve even more17. Therefore, the plane of safe dissection when lifting the temporal region is below the superficial temporal fascia and subperiosteal in the frontal region.

Figure 3 - Relationships between the supraorbital nerve branches and anatomical planes of the forehead.
Surgical Technique
With the patient in an orthostatic position, the elevation of the temporal region of the eyebrow position and approach of the corrugator muscle were assessed. In general, it is unnecessary to raise the medial third of the eyebrows and not desirable to totally abolish the activity of the corrugator supercilii muscles to preserve minimum facial expression of the patient.
The incision in the scalp was marked 1 cm above the ear in the temporal region, rising in an arched path approximately 2 cm after the capillary edge, where the transition of sensitivity supplied by the medial and lateral branches of the supraorbital nerve occurs. The medial extension of the incision at the skin level was determined according to the need for skin resection, with the possibility of meeting the incisions on both sides.
In patients with a very high forehead, the incision may be pre-capillary with skin resection and lowering of the hairline of the forehead. The upper blepharoplasty was marked routinely.
The field block was performed under anesthetic and vasoconstrictor administration. The procedure started with the removal of upper eyelid skin. After hemostasis, the pre-orbital portion of the orbicularis oculi muscle was incised on the upper edge of the blepharoplasty incision, being dissected at its rear face above the orbital septum, to the orbital rim bone. The corrugator muscle was dissected from the vascular pedicle and supratrochlear nerve branches, and a large segment was resected3,19-21.
In the intermediate and lateral thirds of the orbital rim, an incision was made with a scalpel in the periosteum parallel to the rim. The periosteum was raised with a "zest" or dissector throughout the frontal region to the lateral rim of the orbit, releasing the lateral orbital ligament and temporal crest.
In sequence, an incision was made on the frontoparietal region only at the scalp, which was carefully dissected caudally by 3-4 cm to avoid injury to the sensory nerves of the lateral branch of the supraorbital muscle, which arise on the galea aponeurotica.
The superficial temporal fascia was subsequently incised to the plane of the deep temporal fascia, and the medial incision was extended to 1 cm beyond the temporal crest. The superficial temporal fascia flap, which contains the temporal branch of the facial nerve, was raised close to the deep temporal fascia. The temporal crest was dissected caudally to the orbital rim, and the subperiosteal plane was accessed medially (Figures 4 and 5). Thus, the transpalpebral and coronal dissections met. Therefore, the superficial temporal fascia and galea with periosteum formed a single plane. This flap was then pulled cranially to the desired height, and a suture lock was made with 2-0 nylon monofilament. Medially, the galea was pulled as needed, and a suture plication was performed without addressing the nerves. Laterally, the superficial temporal fascia was pulled cranially and laterally and subsequently sutured (Figure 6). The overlapping scalp was resected and sutured without any tension with 5-0 nylon monofilament. With vertical traction, the deep and superficial flaps underwent medial rotation. A small redundancy of the scalp may appear in the medial end of the incision, which can be corrected with a small extension of the scar (Figure 7).

Figure 4 - Area of subperiosteal detachment (green), and direction of traction of the deep and superficial flaps (arrows).

Figure 5 - Temporofrontal blepharoplasty and facial incisions. In detail, the excision of the scalp. 1 = subperiosteal dissection for transpalpebral access. 2 = subperiosteal flap dissection of the periosteum and galea for temporal access.

Figure 6 - In A, dissection of the scalp. In B, lateral incision of the superficial temporal fascia until the emergence of the lateral branch of the supraorbital nerve. Dissection of the temporal crest and medial subperiosteal plane.

Figure 7 - In A, traction of the galea aponeurotica flap and periosteum. In B, plication and fixation of the medial flap to the temporal crest: 1 = plication and fixation of the medial flap to the temporal crest, where the lateral branch of the supraorbital nerve is located; 2 = lateral view of the temporal crest, observing traction of the incised fascia, which is folded to strengthen the flap; 3 = scalp flap after accommodation and resection of the excess skin, sutured with 5-0 nylon monofilament with no traction.
RESULTS
There were no cases of muscle paralysis in this group of patients. Six (30%) patients had postoperative transient paresthesia of the parietal region, which lasted from 2-6 weeks, probably due to perioperative injury or postoperative edema compression.
No patient reported any difference in the sensitivity of the frontoparietal region compared to other areas of the body. There was no enlargement of scars.
When present, postoperative pericicatricial alopecia persisted for 2 months. There was no asymmetry of the position of the brows; to date, there were no cases of the recurrence of ptosis of the eyebrows, presence of forehead wrinkles, or hyper- or hypocorrection.
There was 1 case of insufficient myectomy of the corrugator muscles, which were very strong. In addition, 1 patient required reoperation for myectomy of the orbicularis oculi (i.e., pre-lateral orbicularis) because of hypertonicity (Figure 8).

Figure 8 - In A and B, preoperative appearance in frontal and profile views, respectively. In C and D, postoperative aspects of cervicofacial facelift with SMAS plication, upper blepharoplasty with partial myectomy of the corrugator muscle as well as subperiosteal periorbital and frontal and temporal crest dissection, lower blepharoplasty "pinch," periorbital and malar fat grafting, and temporofrontal lifting in 2 planes in the frontal and profile views, respectively. In E and F, postoperative appearance with slight elevation of the tail of the eyebrows and full frontal muscle relaxation, i.e., observed inactivity of the corrugator muscles of the eyebrows.
Figures 9 and 10 illustrate some cases in this series.

Figure 9 - In A, preoperative appearance. In B, postoperative cervicofacial lifting and temporofrontal lifting. Improvements in periorbital wrinkles, brow contour, and skin distribution can be observed. In C, juxtotragus and pre-capillary preauricular scars. In D, temporal and parietal intracapillary scar.

Figure 10 - In A and B, preoperative appearance in the frontal and profile views, respectively. In C and D, postoperative appearance 1 year after cervicofacial lifting in frontal and profile views, respectively.
DISCUSSION
The planes that correspond to the facial SMAS in the frontal and temporal regions are the superficial temporal fascia and galea aponeurotica, respectively15. Since the lateral branch of the supraorbital nerve passes adjacent to the periosteum on the forehead and the temporal branches of the facial nerve are located in the superficial temporal fascia, the safest and most effective surgical plane is the subperiosteal in the forehead and subfascial in the temporal region18. The release of the temporal crest, adhesion band, and orbital ligament is essential for improving the block lifting of this region15,16. Simultaneously, the depressor muscles of the forehead can be mitigated as needed20,21. Since there is generally no need or desire to significantly elevate the medial part of the forehead, partial myectomy of the corrugator muscles may suffice, although the depressor muscles of the supercilia and procerus can easily be addressed by superior transpalpebral access if needed. Similarly, laterally, a range of pre-orbital orbicularis oculi muscle can be resected via the access of blepharoplasty in some cases.
The techniques of endoscopic and small incision frontoplasty have or may have the same length and dissection plane. The elevation of the supercilia3-13 can be performed with the aid of wire that directly addresses, raises, and fixes the supercilia in more rigid structures by the tines (i.e., endotine), fixed on the bone plate14. It is possible to perform this procedure without fixation as demonstrated by Troilius12,13, who used a technique in which with the front of the periorbital region is released by the subperiosteal plane and the frontal muscle postoperatively elevates this region continuously. However, these techniques do not remove the excess scalp, pull the deep plane more broadly, or address the excess skin of a long and tall forehead5.
The skin incision and extensive dissection proposals in this article aim to provide more harmonious and uniform distribution and traction of the temporofrontal region. The skin is not pulled in tension; it is only distributed and accommodated. All of the tension is supported by suturing the superficial temporal fascia laterally and the plication of galea and periosteum medially. The superficial temporal fascia incision extends up to 1 cm medially to the temporal crest, preserving the lateral branch of the supraorbital nerve; moreover, the subperiosteal dissection encompasses and releases the entire forehead. Cranial and medial tractions elevate the position of the frontal muscle and tighten the skin. With no need for contraction, the frontal muscle relaxes and the front wrinkles disappear, making it unnecessary to perform myotomy or partial myectomy of the frontal muscle. Unlike techniques that directly address and statically set the eyebrows, with the proposed technique, the eyebrows remain free and move naturally without excessive traction. Vertical traction of the temporal flap distributes the skin in this region that is accumulated because of the facelift without lifting the rib and improves the lateral periorbital region, reaching the middle third.
It should be noted that this study is not designed to compare the proposed technique with other well-established procedures. Instead, the objective is to evaluate the effectiveness of this technique and the possibility of reducing potential complications of coronal lifting.
CONCLUSIONS
A large incision in the scalp allows for better distribution and smooth traction of the skin flap. The traction is performed in the deep plane of the galea periosteal, and the cutaneous scar is not tensioned and therefore presents no scarring enlargement or alopecia. The incisions on each side may meet medially if necessary. In cases with a long and high forehead, the incision can be pre-capillary with lowering of the front hair line using the same plication technique. The incision of the superficial temporal fascia is extensive but limited to 1 cm medial to the temporal crest, preserving the lateral branch of the supraorbital nerve and the sensitivity of the scalp. This incision allows extensive mobilization of the superficial temporal fascia and galea periosteal flaps in addition to uplifting and relaxing the frontal muscle, eliminating forehead wrinkles. The lack of static fixation of the supercilia allows them to remain free and move naturally. Moreover, partial myectomy of the corrugator muscles do not completely "freeze" the glabella, preserving a minimum natural aspect without exaggeration or distortion.
Finally, the procedure is safe, simple, requires no special equipment or materials, and has the advantage of wide and good skin distribution, encompassing the frontal and temporal regions.
REFERENCES
1. Rees TD, Aston SJ, Thorne CHM. Blepharoplasty and facialplasty. In: McCarthy JG, ed. Plastic surgery. Part 2: the face. Philadelphia: WB Saunders; 1990. p.2406-10.
2. Day CR, Nahai F. Forehead correction of aging. In: Mathes SJ, ed. Plastic surgery: the head and neck. Part 1. Philadelphia: Saunders Elsevier; 2006. p.47-76.
3. Cintra HP, Basile FV. Transpalpebral brow lifting. Clin Plast Surg. 2008;35(3):381-92.
4. Tabatabai N, Spinelli HM. Limited incision nonendoscopic brow lift. Plast Reconstr Surg. 2007;119(5):1563-70.
5. Codner MA, Kikkawa DO, Korn BS, Pacella SJ. Blepharoplasty and brow lift. Plast Reconstr Surg. 2010;126(1):1e-17e.
6. Nahai F. Endoscopic brow lift: three-portal approach. In: Nahai F, Saltz R, eds. Endoscopic plastic surgery. St. Louis: Quality Medical Publishing; 2008.
7. Jones BM, Grover R. Endoscopic brow lift: a personal review of 538 patients and comparison of fixation techniques. Plast Reconstr Surg. 2004;113(4):1242-50.
8. Graf R, Pace D, Araújo LR. Cirurgia videoendoscópica frontal e de terço médio: experiência de 8 anos. Rev Soc Bras Cir Plást. 2005;20(4):197-203.
9. Graf RM, Tolazzi AR, Mansur AE, Teixeira V. Endoscopic periosteal brow lift: evaluation and follow-up of eyebrow height. Plast Reconstr Surg. 2008;121(2):609-16.
10. Graham DW, Heller J, Kurkjian TJ, Schaub TS, Rohrich RJ. Brow lift in facial rejuvenation: a systematic literature review of open versus endoscopic techniques. Plast Reconstr Surg. 2011;128(4):335e-41e.
11. Dayan SH, Perkins SW, Vartanian AJ, Wiesman IM. The forehead lift: endoscopic versus coronal approaches. Aesthetic Plast Surg. 2001;25(1):35-9.
12. Troilius C. A comparison between subgaleal and subperiosteal brow lifts. Plast Reconstr Surg. 1999;104(4):1079-90.
13. Troilius C. Subperiosteal brow lifts without fixation. Plast Reconstr Surg. 2004;114(6):1595-603.
14. Walden JL, Orseck MJ, Aston SJ. Current methods for brow fixation: are they safe? Aesthetic Plast Surg. 2006;30(5):541-8.
15. Knize DM. Aponeurose epicraniana e fáscias temporais. In: Knize DM, ed. Região temporal e fossa temporal. Rio de Janeiro: Revinter; 2007. p.45-72.
16. Ghavami A, Pessa JE, Janis J, Khosla R, Reece EM, Rohrich RJ. The orbicularis retaining ligament of the medial orbit: closing the circle. Plast Reconstr Surg. 2008;121(3):994-1001.
17. Knize DM. Nervos e vasos da fronte e da fossa temporal. In: Knize DM, ed. Região temporal e fossa temporal. Rio de Janeiro: Revinter; 2007. p.25-44.
18. Knize DM. A study of the supraorbital nerve. Plast Reconstr Surg. 1995;96(3):564-9.
19. Knize DM. Anatomic concepts for brow lift procedures. Plast Reconstr Surg. 2009;124(6):2118-26.
20. Knize DM. Transpalpebral approach to the corrugator supercilli and procerus muscle. Plast Reconstr Surg. 1995;95(1):52-60.
21. Janis JE, Ghavami A, Lemmon JA, Leedy JE, Guyuron B. The anatomy of the corrugator supercilii muscle: part II. Supraorbital nerve branching patterns. Plast Reconstr Surg. 2008;121(1):233-40.
Member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery; member of the Sociedade Brasileira de Microcirurgia Reconstrutiva/Brazilian Society of Reconstructive Microsurgery; surgeon of the Reconstructive Microsurgery Service, Hospital Federal dos Servidores do Estado, Rio de Janeiro; Coordinator of the Medical Residency and the Plastic Surgery Research Center, Hospital Federal do Andaraí do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Correspondence to:
Chang Yung Chia
Av. Lúcio Costa, 3.360 - Bloco 8 - ap. 2402 - Barra da Tijuca
Rio de Janeiro, RJ, Brazil - CEP 22630-010
E-mail: changplastica@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: May 18, 2012
Article accepted: September 2nd, 2012
This study was performed at the private practice of the author, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter