

Original Article - Year 2012 - Volume 27 -
Anatomic study of pockets areas in the hypogastrium
Estudo anatômico de bolsões adiposos na região hipogástrica
ABSTRACT
BACKGROUND: In lipodystrophies of the anterior abdominal wall, variables such as genetic factors, weight gain, age, and loss of muscle tone, either alone or in combination, determine generalized aesthetic changes or changes localized in the epigastrium, hypogastrium, or both. The aim of this study was to describe the limits, distribution, and dimensions of fat bags in the hypogastrium, as well as their anatomic relationships with the neighboring structures.
METHODS: Fifty-seven anatomical specimens were dissected from patients undergoing abdominoplasty, during which the hypogastrium was resected en bloc. Moreover, the anterior abdominal wall was also dissected in 8 cadavers. In all samples, the lamellar layer was resected, keeping the dermis-epidermis, areolar layer, and superficial fascia intact.
RESULTS: In all specimens, 2 symmetrical adipose clusters were observed bilaterally in the areolar layer, which were in the shape of a bag and had peculiar coloration. These bags were analyzed in relation to their neighboring tissues: the skin, superficial fascia, and deep fat layer.
CONCLUSIONS: The lamellar layer was considered as a structural base of the skin, owing to its thinness. The areolar layer showed accumulations and varying amounts of fat in the various body regions without precise limits, which were particularly observed in dissections of the lower abdominal wall and identified by their elasticity, volume, and coloration.
Keywords: Abdomen. Adipose tissue. Lipectomy.
RESUMO
INTRODUÇÃO: Nas lipodistrofias da parede abdominal anterior, fatores genéticos, aumento de peso, idade e lasseamento da musculatura, de forma isolada ou associada, determinam alterações estéticas generalizadas ou localizadas no epigástrio, no hipogástrio ou, mesmo, em ambas as regiões. O objetivo deste estudo é descrever os limites, a disposição, as relações anatômicas das bolsas adiposas no hipogástrio com as estruturas vizinhas e suas dimensões.
MÉTODO: Foram dissecadas 57 peças anatômicas de pacientes submetidas a abdominoplastia, em que o hipogástrio foi ressecado em monobloco. Além disso, foi realizada dissecção da parede abdominal anterior em 8 cadáveres. Em todas as peças, a camada lamelar foi ressecada, mantendo-se a derme-epiderme, a camada areolar e a fáscia superficial íntegras.
RESULTADOS: Em todas as peças, foram observados dois cúmulos adiposos na camada areolar bilateralmente, simétricos, em forma de bolsa e de coloração peculiar. Essas bolsas foram também analisadas em relação aos tecidos cutâneos vizinhos: pele, fáscia superficial, camada profunda de gordura.
CONCLUSÕES: A camada lamelar foi considerada estrutural como base da pele, pela sua fina espessura, e a camada areolar apresentou acúmulos e volumes variáveis de tecido adiposo nas diversas regiões do corpo, sem limites precisos, particularmente observados nas dissecções da parede abdominal inferior, pela sua elasticidade, pelo volume e pela coloração.
Palavras-chave: Abdome. Tecido adiposo. Lipectomia.
Subcutaneous fat deposits in the form of dense bags located in the anterior abdominal wall have been referred to as esteatomas1 and are more commonly found in women2. The location, distribution, and boundaries of these deposits have not been fully defined in the literature owing to the absence of corroborative dissections. Figures 1A and 1B illustrate this type of fat accumulation, the shape and distribution of which often resembles the number 8.
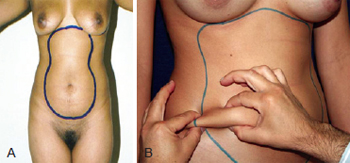
Figure 1 - Regions of the epigastrium and hypogastrium, delimited by fatty buildups in the form of localized pockets. The difference in thickness was clearly observed by clamping the skin.
Topographical knowledge of the anterior abdominal wall, as well as other regions of the body, is imperative for any type of surgery for aesthetic purposes, particularly liposuction. Considering the diversity of fat accumulation in the region of the anterior abdominal wall, the elimination of excessive tissue with excellent initial aesthetic effects may ultimately contribute to further distortions and irregularities in skin relief.
In very obese patients or patients who have undergone major weight loss, macro and microscopic changes occur in the structure of both layers of the adipose tissue as well as the superficial fascia. In these patients, localization of the adipose bags is not evident because of the fragmentation of the fascia and invasion by fatty lobes in the lamellar and areolar layers3.
The aim of this study was to describe the borders, distribution, and dimensions of fatty bags in the hypogastrium as well as their anatomic relationships with neighboring structures.
METHODS
Based on previous demarcations performed in the standing position, 57 tummy tucks with low transverse suprapubic incision were performed in female patients by en bloc resection of the excessive skin of the hypogastrium4,5. The abdominal wall of 8 cadavers was also dissected en bloc in the epigastric and hypogastric regions, with preservation of the adipose tissue (Figure 2).

Figure 2 - Cadaver dissection with a single folded skin flap from the epigastrium and hypogastrium without evidence of fat bags or boundaries because of preservation in formaldehyde.
The pieces of the hypogastrium were dissected in an inverted position, with the dermal-epidermal layer on the surgical table. First, the lamellar layer was resected and compacted with clear borders while preserving the superficial fascia directly covering the areolar surface. The lamellar layer in all specimens appeared homogeneous in thickness and extension (Figures 3 to 5). After resection of the lamellar layer and removal of the superficial fascia, the fat bags appeared pinkish, and they could be easily and clearly distinguished from the surrounding gray tissues.

Figure 3 - Cutaneous monoblock resected from the hypogastrium during abdominoplasty. The dermoepidermal piece was supported by the table for dissection and direct visualization of the superficial fascia was applied to the areolar layer after removal of the lamellar layer. The 2 bags of fat present with clear bilateral limits.
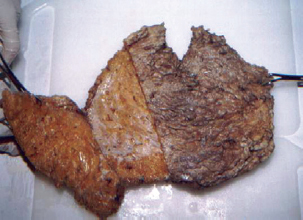
Figure 4 - Specimen of the hypogastrium of a cadaver with partial incision of the lamellar layer, exposing the adipose bag.

Figure 5 - A thin lamellar layer was observed in dissected specimens.
The 2 bags were bilaterally positioned in the hypogastrium and were symmetrical and of equal size. Their major vertical axis reached the level of the umbilicus superiorly, and in some specimens, it reached the inguinal ligament inferiorly. The medial borders showed connective tissue joining them to the level of the dermis (Figure 6).
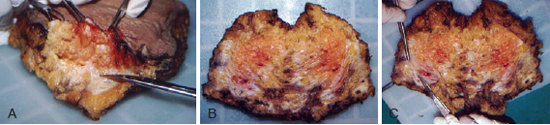
Figure 6 - In A, B, and C, pieces of skin from the hypogastrium are shown; the fat bags can be seen to be positioned bilaterally and are salmon-red in color with clear borders. The partially rebated superficial fascia, indicated with forceps and the end of a pair of scissors, is separated medially by a web of connective fibers from the level of the umbilicus to the inguinal ligament.
The adipose bags showed a different consistency from the neighboring adiposity, being more elastic and comparable to a "bag of jelly" covered by the surrounding fascia. Outside their borders, the fascia and fat were less elastic and more consistent, respectively. Figure 7 defines the direct contact of the dermis and superficial fascia with the areolar layer, separating the lamellar layer. Figures 8 and 9 illustrate the reflection of the superficial fascia of the external borders of the bags towards the dermis, which was considered as their lateral border, comparable to a thin pocket containing these bags. With regard to the volumes observed, the bags could be evaluated as small, medium, or large (Figure 10). The occurrence of herniation from the fat layer to the lamellar layer was also observed (Figure 11). The formaldehyde-preserved samples, which included the epigastrium (Figure 12) and were positioned at the navel center with a folded lamellar layer, showed slight contouring of the bags in the epigastrium and hypogastrium.
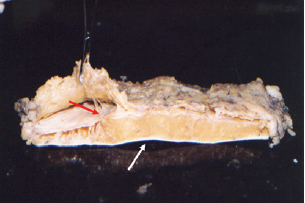
Figure 7 - Cross section of skin where the white arrow indicates the epidermis-dermis and the red arrow indicates the superficial fascia, which are separated by the areolar layer.
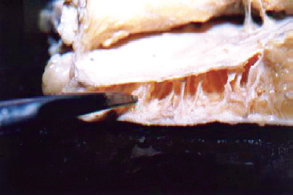
Figure 8 - Cross-section of skin with the scissors indicating reflection of the superficial fascia on the outer limits of the bags towards the dermis, involving the medial fat purse.

Figure 9 - Clamping of the superficial fascia laterally, involving a fat purse.
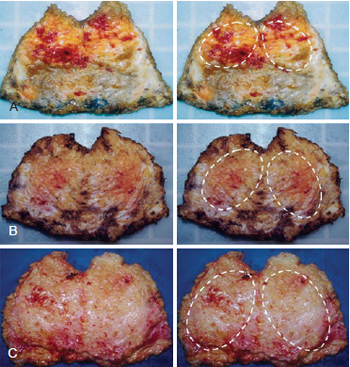
Figure 10 - Adipose bags of different sizes, classified as small (A), medium (B), or large (C).
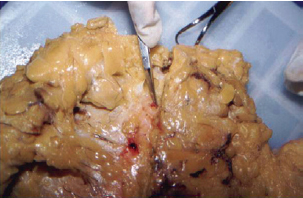
Figure 11 - Tip of the scissors indicating detail on herniation of adipose tissue through the superficial fascia of the lamellar cover in the direction of the areolar layer.
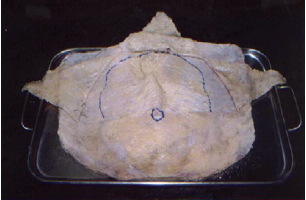
Figure 12 - Dissected and inverted specimen of the hypogastrium of a cadaver and inverted segment containing the epigastrium and hypogastrium, with the navel at the center. The lamellar layer folded in 3 directions exposes the superficial fascia containing fat inside bags, as a closed compartment.
This study allows us to draw attention to possible adipose bags, which may be distributed in other body regions (Figure 13) and have not yet been evidenced by studies and more conclusive dissections.

Figure 13 - Fat bags distributed in other body regions.
RESULTS
In patients weighing within the normal range and with epigastric and hypogastric adiposity, fat bags were difficult to visualize. In obese and multiparous patients, fat bags were only clear by palpation in the standing position.
The adipose bags had lengths ranging from 8-17 cm (mean, 12.5 cm), widths ranging from 6.3-10.5 cm (mean, 8.4 cm), and thicknesses ranging from 1.5-4.7 cm (mean, 3.1 cm).
The lamellar layer was thinner than the areolar layer in all specimens. It was consistently possible to visualize and palpate the lamellar layer, and it was always found to have the same thickness. The specimens from cadavers showed no hypogastric bags because they were conserved in formaldehyde.
DISCUSSION
Despite their easy identification upon inspection and palpation, there are no detailed reports describing hypogastric bags in the literature4-12. Perforations in the superficial fascia and fat displacement in the lamellar layer by areolar fat (Figure 11) were also observed, corroborating findings from other authors3.
The thickness of the fat layer in the lamellar layer and the fatty accumulations in the areolar layer of the anterior abdominal wall were comparable in all dissected specimens. This finding allows us to question the necessity of performing liposuction in the lamellar layer of the anterior abdominal wall, and confirms the requirement of new studies to support this hypothesis. To our knowledge, no studies have been performed to prove the existence of these bags in other regions of adiposity.
We performed dissections on 8 cadavers preserved in formalin; these dissections were carried out on the anterior abdominal wall and exposed the epigastrium and hypogastrium, but they were not conclusive when compared to findings in the dissected samples from abdominoplasties. The fatty pockets were not well defined and did not show clear limits because the cadavers were preserved in formalin, and thus served only to establish that this procedure is not viable for this type of study.
CONCLUSIONS
Anatomical dissections of skin specimens from the hypogastrium showed the presence of adipose tissue in the areolar layer, which had the characteristics of adipose bags and precise limits. The constant lamellar layer thickness within an individual in the region of the hypogastrium and diversification in the areolar layer suggests that there is no need to perform liposuction in the lamellar layer, reducing the risk of adverse postoperative events.
REFERENCES
1. Illouz YG. Lipoesculpture et chirurgie de la silhouette. Chirurgie plastique reconstructrice et esthétique. Encycl Med Chir Editions Scientifiques et Médicales. Paris: Elsevier; 1998. p.45-120.
2. Souza Pinto EB. Lipoaspiração superficial. Rio de Janeiro: Revinter; 1999.
3. Silva SL. Variações anatômicas do tecido celular subcutâneo pós-perda ponderal. Rev Bras Cir Plást. 2010;25(4):675-8.
4. Avelar JM. Surgical abdominoplasty without panniculus undermining and resection. São Paulo: Hipócrates; 2002. p.57-110.
5. Markman B, Barton Jr FE. Anatomy of the subcutaneous tissue of the trunk and lower extremity. Plast Reconstr Surg. 1987;80(2):248-54.
6. Melega JM. Cirurgia plástica: fundamentos e arte. Cirurgia Estética. Vol. IV. Rio de Janeiro: MEDSI; 2003. p.609-705.
7. Sabiston DC. Textbook of surgery. 13rd ed. Philadelphia: W. B. Saunders; 1986.
8. Hollinshead WH. Anatomia. 4ª ed. Rio de Janeiro: Interlivros; 1991. p.491-503.
9. Latarjet M, Liard AR. Anatomia humana. 2ª ed. São Paulo: Panamericana; 1989.
10. Testut L. Tratado de anatomia humana. Rio de Janeiro: Salvat Editores; 1976. p.940-88.
11. Pontes R. Abdominoplastia: ressecção em bloco e sua aplicação em lifting de coxa e torsoplastia. São Paulo: Revinter; 2004. p.11-20.
12. Saldanha OR. Lipoabdominoplastia. Rio de Janeiro: Di Livros; 2004.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), Uberaba, MG, Brazil.
2. Doctor in Human Anatomy and Neuroanatomy, Master and Associate Professor of Anatomy and Neuroanatomy at the Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil.
3. Plastic surgeon, Master and Doctor in Plastic Surgery, full member of the SBCP, Santos, SP, Brazil.
4. Plastic surgeon, full member of the SBCP, Santos, SP, Brazil.
5. General surgeon at the UFTM, Uberaba, MG, Brazil.
6. Nurse, Master's student at the UFTM, Uberaba, MG, Brazil.
7. Medical student at the UFTM, Uberaba, MG, Brazil.
Correspondence to:
Renato Sivieri de Souza
Rua Vigário Silva, 750 - Centro
Uberaba, MG, Brazil - CEP 38022-190
E-mail: rsivieri@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 16, 2012
Article accepted: August 5, 2012
This study was performed at the Service of Plastic Surgery Dr. Ewaldo Bolivar de Souza Pinto, Universidade Santa Cecília de Santos (UNISANTA), Santos, SP, Brazil, and in the Federal University of Triângulo Mineiro (UFTM), Uberaba, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter