

Original Article - Year 2012 - Volume 27 -
Use of the informed consent form in aesthetic plastic surgery
Uso do termo de consentimento informado em cirurgia plástica estética
ABSTRACT
BACKGROUND: The informed consent form provides security for the plastic surgeon and the patient, and its use is recommended by the Consumer's Defense Code.
METHODS: A total of 100 judgments made by the courts of 5 Brazilian states were analyzed, in cases involving aesthetic plastic surgeries. This retrospective study was conducted between July 2010 and August 2012 involving a total of 3,427 plastic surgeons. The most common causes of lawsuits and the evidence that led to conviction or acquittal decisions in these cases were assessed.
RESULTS: There was an average conviction rate of 55% among the states under study (range, 35-85%). The average compensation for moral damages was R$30,900. The main surgical procedures that resulted in the lawsuits and the convictions were abdominoplasty, mammoplasty, and breast implantation. In the cases in which the physician was acquitted, there was a favorable expert opinion in 84,6% of the judgments, whereas adequate information was provided in 100% of such cases.
CONCLUSIONS: This study showed that a favorable expert opinion and the adequate provision of information about suggested treatments were instrumental in physician acquittal.
Keywords: Informed consent. Plastic surgery. Jurisprudence.
RESUMO
INTRODUÇÃO: O termo de consentimento informado representa uma segurança para o cirurgião plástico e para o paciente, sendo sua utilização preconizada pelo Código de Defesa do Consumidor.
MÉTODO: Realizada análise de 100 acórdãos dos Tribunais de Justiça de 5 estados brasileiros, em casos envolvendo cirurgias plásticas estéticas. O estudo retrospectivo foi realizado no período de julho de 2010 a agosto de 2012, em um universo de 3.427 cirurgiões plásticos. Foram avaliadas as causas mais frequentes das ações e os principais elementos probatórios que levaram à condenação ou absolvição dos casos.
RESULTADOS: Houve uma taxa média de condenação entre os estados avaliados de 55%, variando de 35% a 85%. O valor médio das indenizações por dano moral foi de R$ 30.900,00. As principais cirurgias que motivaram as ações e as condenações foram abdominoplastia, mamoplastia e implante de próteses mamárias. Nos casos de absolvição do médico, houve perícia oficial favorável em 84,6% dos acórdãos, além da prestação de informações adequadas em 100% dos casos avaliados.
CONCLUSÕES: Este estudo permitiu observar que a perícia oficial favorável e o fornecimento adequado das informações sobre os tratamentos preconizados foram fundamentais para a absolvição do médico.
Palavras-chave: Consentimento livre e esclarecido. Cirurgia plástica. Jurisprudência.
The informed consent form (ICF) provides security for the plastic surgeon and the patient since it levels and strengthens the contractual nature of the service between the parties. This kind of arrangement consists of the physician being obliged to inform the patient and the patient stating that he/she understands and agrees to undergo the proposed treatment without having the ability to negate what he/she has signed unless the form was obtained irregularly.
Although the Civil Code, the Consumer's Defense Code, and the Medical Ethics Code (CEM) recommend that information must be provided to patients prior to starting treatment, many physicians neglect the security obtained with the simple application of the ICF duly signed by both parties1.
Although the CEM is not clear about whether the ICF should be obtained and signed by the patient or whether an oral agreement is sufficient, countless judgments and court sentences undoubtedly state that - what is not written does not exist. Material evidence that the information has been given in a proper document under the correct circumstances and signed by all parties is required from and recommended to physicians1-3.
Plastic surgeons have been concerned with the way some convictions have been decided, as evidenced by somewhat "feckless" votes and defended by some lawyers; thus, even without a clear justification of guilt, a physician ends up being convicted because the court assumes that aesthetic plastic surgery is associated with the obligation of delivering a positive result. Therefore, a conviction occurs even though there is no lack of skill, imprudence, or negligence. In addition, no consideration is given to the involved biological, technical, and random circumstances that are outside the physician's or patient's control, and evidence is often disregarded.
The court's necessity of obtaining a positive result following aesthetic plastic surgery has caused a considerable amount of concern within the medical community since many judges do not yet understand that it is impossible to guarantee results in all types of surgery, as organic tissue reacts independently of the wills of physicians and patients4.
Fortunately, a new jurisprudence has been increasingly adopted by Brazilian judges in alignment with a contemporary trend, thus following in the steps of the French and Canadian systems, which consider aesthetic plastic surgery an obligation of means and requires that a physician's guilt be proven prior to a conviction. As such, the decisions detailed in their judgments are true legal monographs in which they seek to extensively assess the topic by examining every angle and all evidence as well as the technical opinion of official experts. The latter, in turn, decipher medical facts for a judge who does not possess that knowledge, which makes it all the more critical that the expert is a plastic surgeon and an expert in legal medicine or medical practices himself, since he will interpret the singular biological and technical phenomena of his specialty.
One mitigating circumstance, which currently is already an obligation for all physicians, is the use of the ICF that must be applied correctly. That document makes the doctor-patient relationship clear, transparent, and honest, and respects the autonomy of the patient in having his body violated by surgery. Thus, it ensures that the patient is aware of the advantages, disadvantages, risks, objectives, possible results, and limitations. Moreover, the plastic surgeon, when using it properly, shows his repute, good intentions and principles, honesty, and this then becomes a mitigating factor.
This study sought to assess the importance and influence that the use of ICF had in the convictions and acquittals of plastic surgeons in the Courts of Justice of 5 Brazilian states in addition to proposing an ICF model that is derived from ample revisions on the subject.
METHODS
A recent analysis was conducted on the last 100 judgments obtained in the courts of justice of Brasília, Minas Gerais, Rio Grande do Sul, Rio de Janeiro, and Sao Paulo in alleged cases involving aesthetic plastic surgery errors. This retrospective study was conducted between July 2010 and August 2012 by searching for the expression "plastic surgery," and considering only those judgments focusing on aesthetic plastic surgery; cases of corrective plastic surgery were excluded from this study. The last 20 judgments of each state were considered, encompassing a total of 3,427 active plastic surgeons.
The data thus obtained yielded variables that were analyzed in the form of absolute figures and their simple corresponding percentage. The obtained results are presented in the study as simple occurrence rates.
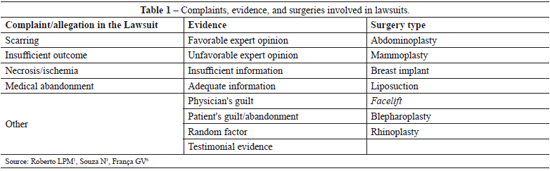
The most common causes of the lawsuits included scarring, insufficient results, necrosis, and medical abandonment, whereas the main forms of evidence included official expert opinions, adequate information, physician or patient guilt, random factors, and witness testimony. The names of the states were hidden and the results were coded as A to E in decreasing order of conviction rates such that the states may not be identified.
The results are shown as tables, and different variables and their frequencies were assessed. During the data extraction process, the autonomy of each judicial organ was respected, as the writing of the judgments differs to allow for different interpretations of similar cases. This fact is a result of the possibility that the judge applies his own free judgment as long as it is based on logic and reason.
Among the several variables under study, the main complaints and allegations that resulted in the lawsuits were assessed, as were the main favorable or unfavorable evidence reported in the case, the types of surgery involved, and the financial amounts involved in the convictions (Table 1).
RESULTS
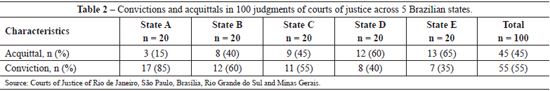
An average conviction rate of 55% was observed in all 100 judgments assessed, with a high conviction rate in the state represented by the letter "A," reaching 85%; a moderate rate in the state represented by the letter "B," reaching 60%; and a low rate in the state represented by the letter "C," reaching 55%. The states with the lowest conviction rates were represented by the letters "D," reaching 40%, and "E", reaching 35% (Table 2).
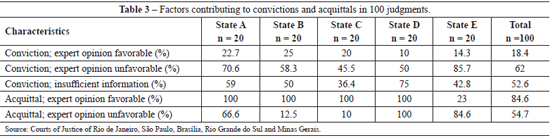
The study showed that, in the cases in which the plastic surgeon was acquitted, the medical opinion given by the court's expert was in favor of the physician in 84.6% of the cases. The plastic surgeon was convicted in 18.4% of the cases despite a favorable expert's opinion. The plastic surgeon was convicted in another 62% of cases, but the expert's opinion was unfavorable.
We found that in the judgments acquitting the plastic surgeons, the provision of preoperative information was adequate and given through the use of an ICF. The routine use of an ICF was more common in the states with the highest acquittal rates (letters "D" and "E", being observed in 100% and 84.6% of the judgments, respectively).
Various factors were associated with the convictions and acquittals, such as abandonment of treatment, failure to observe medical recommendations, and careless actions by the patients, all of which were facts contributing to the physicians' acquittals. On the other hand, patient abandonment by the physician, prescriptions given by phone, inadequate filling of the patient's record, poor guidance, and inadequate surgical preparation were indicated as causes for convictions (Table 3).
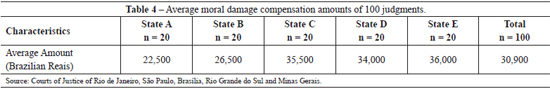
The average amount of compensation for moral damages was R$ 30,900 at the time of the judgment, although this does not include material damages and the plaintiffs' attorney's fees (Table 4).
The surgeries that yielded the highest number of lawsuits were abdominal, breast, and mammary prosthesis aesthetic surgeries, and these procedures also resulted in the highest number of convictions.
DISCUSSION
The first use of ICF occurred in 1767 in England in a badly performed orthopedic procedure that resulted in conviction of the physician5. During World War II, in which experimental tests caused cruel suffering and death in human beings associated with the ideas of eugenics in Germany (1933) preaching the extinction of the inferior races, the importance of ICF use prior to treatment was stressed. The Nuremberg Code (1947), the Declaration of Helsinki (1964), and the Word Medical Assembly (Hong Kong, 1989) confirmed the use of the ICF.
The Supreme Court of the United States (1914) acknowledged the right to self-determination, with the expression "informed consent" being introduced in 1957. In the 1970s, the medical professional hazard made the adoption of the ICF compulsory, which cannot be negated in the United States, and has probative value1.
Obtaining the ICF consolidates the doctor-patient relationship since there are obligations of both parties and the principles of good faith, ethics, loyalty, correction, and truthfulness prevail as well as the obligation to keep the contractual agreement. That document also preserves the person's rights of protection, and the right to life, dignity, freedom, equality, health, and publicity as well as personal, physical, moral, and psychic integrity2.3.
The physician, as a service provider, must provide correct, clear, and precise information about the treatments and their risks and must answer for the insufficient information in cases of fault since the physician has taken away the patient's right to self-determination4.
There are more than a dozen designations for ICF; however, all professionals must provide adequate and sufficient information, include the nature and purpose of the treatment, the possible risks and benefits, and the alternative treatments in addition to the risks of not performing the proposed or alternative treatments. The patient must also be given the opportunity to ask questions and obtain understandable answers in addition to making a decision free from undue coercion and influence6.
The ICF must be obtained by a physician, not by an assistant or nurse, and the information must be provided in a clear manner using simple language. It must be collected prior to treatment and written explicitly; the more complicated the treatment, the more comprehensive it must be. The patient may refuse treatment, revoke the already signed consent, and even be replaced by a legal representative in special cases7.
The importance of the adequate use of the ICF may be assessed in the analysis of the judgment results obtained in the courts of justice of 5 Brazilian states in cases of aesthetic plastic surgery. Completion of the patient's medical report and sufficient medical assistance also contributed to that favorable outcome.
The most common causes of lawsuits included the formation of a surgical scar, insufficient surgical outcome, skin necrosis, medical abandonment of the patient, and treatment abandonment by the patient. The main pieces of evidence considered by the judges that contributed to the conviction or acquittal were the medical expertise of the court, the provision of adequate pretreatment information, investigation into the guilt of the physician or patient, the presence of a random factor, and testimonial evidence.
The average conviction rate of Brazilian plastic surgeons was high at 55%. The highest conviction rate was 85%, meaning that 17 of the latest 20 lawsuits reaching the court of justice in that state resulted in conviction of the plastic surgeons, which is highly unfavorable to those professionals. The high number of convictions may be attributed to negligence in the use of the ICF, incomplete filling of the patient's medical record, and random factors in addition to possible medical errors. On the other hand, in the states with the lowest conviction rates (35-40%), of every 20 lawsuits reaching their respective courts of justice, only 7 or 8 resulted in convictions. In these states, physicians were more diligent, which contributed to their better defense by experts during the trial.
One crucial factor in the acquittal of the plastic surgeons was linked to the fact that the medical investigation conducted by the court's expert yielded a result that was favorable to the plastic surgeon, and the physician was not considered guilty. It should be noted that, in many of these cases, there was some kind of complication that was attributed to either random factors or the patient, with the medical expert opinion favoring the physician in 84.6% of such cases. On the other hand, in only 18.4% of the cases resulting in a conviction, the same occurred, despite the court's expert having a favorable opinion regarding the plastic surgeon. This fact has been seen as unjust by physicians, since for the most part the doctor's guilt was not proven and no imprudence, negligence, or lack of skill was observed. In those cases, conviction was the result of the theory of obligation that has been losing its way in Brazilian jurisprudence, which is following in the steps of the Canadian and French judicial systems4,6.
It should be noted that there are many cases in which complications arise due to random factors to which all patients are liable but that have been characterized as medical errors that lead to the physician's conviction, even if he cannot be proven guilty. That discrepancy is already blatant and has been criticized by legal practitioners, who have understood and recognized the existence of the random factor3-6,8. On the other hand, the official medical expert opinion was unfavorable in 62% of the cases in which the plastic surgeons were convicted. As such, there was some fact or damage as a result of the medical act that somehow represented negligence, imprudence, or lack of skill.
Physicians consider it incoherent to consider that obtaining a positive result is obligatory when aesthetic plastic surgery is performed, following a legal view of the right of subjective liability of the physician, since according to article 14 of the Consumer's Defense Code, the provider shall be responsible for repairing the damage caused regardless of guilt in cases of defective services rendered, irrespective of or due to the physician's responsibility for the occurrence of the random factor. Therefore, there is disregard for the fact that the determination of the guilt of independent professionals is necessary and that it must be verified and not presumed. This is even more evident in aesthetic plastic surgery, in which there is a "random factor inherent to the procedure1."
A fundamental factor that is observed and depends only on the actions of the plastic surgeons was the provision of adequate and sufficient information prior to treatment through the application of an ICF. In a relationship between a physician and his patient, there are obligations for both parties, which must follow the principle of good faith with respect for ethics in a relationship of loyalty, accuracy, and truthfulness since both parties must faithfully keep the contractual agreement to ensure that the intended service is obtained2,4,9.
Through Resolution 1.703/03, the Federal Medicine Council sets the criteria for medical advertising and forbids the physician from promising results or guarantees of success of treatments to protect the patient from being deceived by false promises. The CEM confirmed that it is up to the physician to inform the patient about the diagnostic treatments, alternatives, risks, and complications of the procedures and that the patient has the right to consent or refuse2-4,10,11.
Article 4 of the Consumer's Defense Code quotes that the balance of the relationships of consumption resides in supporting the most vulnerable party and in the good faith of the imposition of rights, limitations, and duties, thereby maintaining a contractual balance. Therefore, the physician, who is the service provider, must provide correct, clear, and precise information about the treatment and its risks and that he must answer in cases of insufficient information in case the physician is at fault. The right to the protection of life, health, and safety against risks caused by medical treatment imposes a duty on the physician to clarify the treatment, benefits, and risks to allow the patient to better decide whether to submit to the proposed treatment1-3,7,12,13.
The structure of the ICF states that it must be presented explicitly and in written form; the more complicated the treatment, the more comprehensive it must be, and that the patient may waive the right to consent if they do not know the contents of the ICF and refuse to submit to the treatment. If a patient who is in an appropriate mental state that allows him to make a correct judgment does not wish to undergo a particular treatment, it must not be performed unless there is a risk of death that must be documented. Furthermore, the ICF may be revoked at any moment and the consent may be given by a relative or person in charge, and is only of any value in those situations.
The duty to inform demands more of plastic surgeons, who must go to great lengths to provide information and avoid giving any false expectations in terms of the dangers inherent to any surgery. It must be considered that there is a great expectation regarding the result; the patient must receive adequate information and choose what is best for the procedure. If the physician promises a result, he is obliged to obtain it; otherwise, it is deceitful advertising. Lack of information constitutes moral damage by medical negligence since, if informed, the patient could choose not to submit to the risks of the intervention.
There is restriction regarding the use of the ICF due to the inability of the patient, which, if total, renders the ICF void and, on the other hand, if partial, may even result in cancellation of the document in a legal dispute. When information is inadequate, the ICF may become invalid due to absence of information, inadequate or insufficient information, deception, or coercion1,2,4,9,12,13.
The study also revealed that the average compensation for moral damages among all judgments was R$30,900, which excludes material damages, attorney's fees, technical expert investigations, and judicial expenses, all of which may raise that amount significantly. The main surgeries resulting in lawsuits and convictions were abdominoplasty, mammoplasty, and breast implantation, probably because these are the most commonly performed surgeries. It is therefore recommended that plastic surgeons have a diligent attitude, use the the properly obtained ICF, ensure that it is duly signed by the patient, hire lawyers specialized in medical law, carefully select their patients for surgery, and thoroughly explain the procedures, risks, benefits and expectations.
Proper obtaining of the ICF is, first of all, important for protecting the professional and demonstrates the prudent way in the which the medical act is performed, both for surgical treatment of disease and for aesthetic plastic surgery4,10,11. The judgments that were analyzed clearly demonstrated different interpretations for the judgments of similar cases. Although the autonomy of each judicial court is respected due to the free conviction of each, that creates a feeling of insecurity in those cases in which the physician's guilt was not demonstrated, wherein there was no lack of skill, imprudence, or negligence, and even so, the physician is convicted and held responsible for the random occurrences1,2,10,11.
CONCLUSIONS
The obtained results allow the conclusion that, in cases of aesthetic plastic surgeries in which acquittal occurred, there was a predominantly proper use of the ICF and the medical opinion of the court's expert was favorable to the physician. The most common causes motivating the lawsuits included surgical scarring, allegedly insufficient surgical outcome, skin necrosis, medical abandonment of the patient, and patient abandonment of the treatment. The main forms of evidence considered by the judges that contributed to either conviction or acquittal were the opinion of the court's expert, the provision of adequate pretreatment information, investigation into the guilt of the physician or patient, the presence of a random factor, and testimonial evidence.
The surgeries that were most commonly involved in lawsuits included abdominoplasty, reduction mammoplasty, and breast implantation. If requested, it is recommended that the physician hires specialists in medical law and technical assistance.
REFERENCES
1. Roberto LMP. Responsabilidade civil do profissional da saúde e consentimento informado. 2ª ed. Curitiba: Juruá; 2008.
2. Willherm C. Responsabilidade civil do cirurgião plástico: obrigação de meio ou de resultado. Porto Alegre: Stampa; 2009.
3. Souza N. Erro médico e consentimento informado. Teresina: Jus Navigandi; 2004.
4. Giostri H. Sobre o consentimento informado: sua história, seu valor. Simpósio Medicina e Direito. J Vasc Bras. 2003;2(3):267-70.
5. Appelbaum PS, Lidz CW, Meisel A. Informed consent: legal theory and clinical practice. New York: Oxford; 1987. p.36-7.
6. Jaimovich CA, Kfouri Neto M, Almeida AHT, Pinheiro AG, Loma DC. Debate: consentimento informado e cirurgia plástica. Rev Soc Bras Cir Plást. 2007;22(3):188-93.
7. França GV. Fundamentos de medicina legal. Rio de Janeiro: Guanabara Koogan; 2005.
8. Aguiar Jr RR. Responsabilidade civil do médico. Rev Tribunais. 1995;718:33-5.
9. Avelar JM. Cirurgião plástico: obrigação de meio. São Paulo: Hipócrates; 2000.
10. Menezes CA. Responsabilidade civil do médico. Acórdão publicado na RT 767/118-2000. In: Comentários ao Novo Código Civil. Vol.XIII. Responsabilidade civil, das preferências e privilégios creditórios. Direito CAM & Cavalheri S. Rio de Janeiro: Ed. Forense; 2004. p.21-35.
11. França GV. Direito médico. 9ª ed. Rio de Janeiro: Forense; 2007.
12. Kfouri Neto M. Responsabilidade civil do médico. 5ª ed. São Paulo: Revista dos Tribunais; 2003.
13. Doncatto LF. Modelo de termo de consentimento informado para Cirurgia Plástica. In: Boechat H, ed. Consentimento informado no exercício da Medicina e tutela dos direitos existenciais: uma visão interdisciplinar. Vol. 1. Itaperuna: Hoffmann; 2011. p.122.
Plastic Surgeon, Fellow of the Sociedade Brasileira de Cirurgia Plástica/ Brazilian Society of Plastic Surgery, PhD in Medicine, Associate Professor of Plastic Surgery, Bioethics and Medical Deontology and Coordinator of the Medicine Course of the Universidade Luterana do Brasil (ULBRA), Canoas, RS, Brazil.
Correspondence to:
Léo Francisco Doncatto
Rua Mostardeiro, 780 - cj 202 - Moinhos de Ventos
Porto Alegre, RS, Brazil - CEP 90430-000
E-mail: leodoncatto@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 19, 2012
Article accepted: September 15, 2012
Study performed at the Surgery Department of the Medicine Course of the Universidade Luterana do Brasil (ULBRA), Canoas, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter