ABSTRACT
BACKGROUND: Primary tumors of the long bones are rare, accounting for 0.2-1% of malignant tumors. In the past, amputation was the standard treatment and had a large impact on patient morbidity and mortality. With advances in surgical techniques and multidisciplinary involvement, conservative surgery of the limbs has become the treatment of choice, and reconstruction using a microsurgical fibula flap is the most commonly used technique. In this study, we aimed to present the experience of the National Cancer Institute (INCA) with limb reconstruction using a microsurgical fibula flap following tumor resection from the long bones.
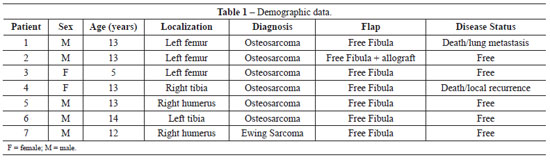
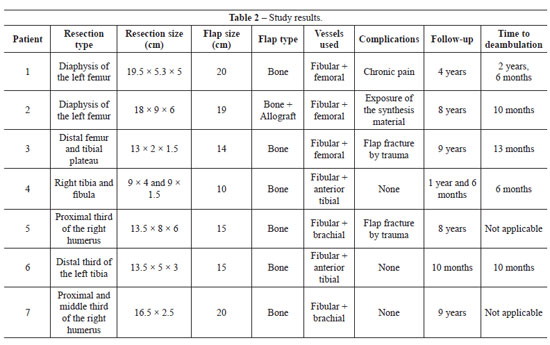
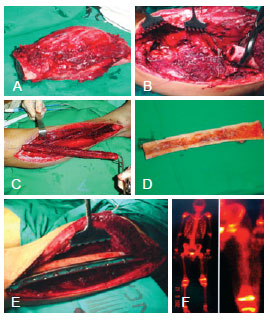
METHODS: We retrospectively analyzed 7 cases of free fibular flap surgery at the INCA from 1997 to 2009 for the reconstruction of defects of the extremities after bone tumor resection. We evaluated the following parameters: gender, age, diagnosis, tumor location, resection size and type, reconstruction size and type, vessels used for the anastomosis, postoperative complications, disease status at the last visit, follow-up, and time to ambulation.
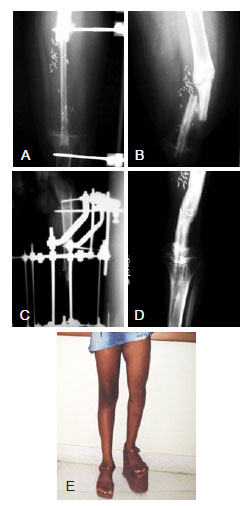
RESULTS: Seven patients with a mean age of 11.8 years (range, 5-14 years) underwent extremity reconstruction with a free fibula flap with 100% bone viability. The lesions were located within the femur, tibia, or humerus. Osteosarcoma was the most common tumor type. The average return to ambulation was 14.7 months.
CONCLUSIONS: The use of a free fibula flap is an excellent alternative for limb reconstruction and features a high bone healing rate, early ambulation, good functionality, and a low complication rate.
Keywords:
Fibula. Extremities. Transplantation, homologous. Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O tumor primário de ossos longos é raro, correspondendo de 0,2% a 1% dos tumores malignos. No passado, a amputação era o tratamento padrão, ocasionando grande impacto na morbidade e na mortalidade desses pacientes. Com o avanço das técnicas cirúrgicas e o envolvimento multidisciplinar, a cirurgia conservadora dos membros tornou-se o tratamento de escolha, sendo a reconstrução com retalho microcirúrgico de fíbula a mais utilizada. Este trabalho tem como objetivo apresentar a experiência do Instituto Nacional de Câncer (INCA) nas reconstruções de membros com retalho microcirúrgico de fíbula após ressecções de tumores de ossos longos.
MÉTODO: Foi realizada análise retrospectiva de 7 casos de retalho livre de fíbula operados no INCA, no período de 1997 a 2009, para reconstrução de defeitos de extremidades após ressecções de tumores ósseos. Foram avaliados os seguintes parâmetros: sexo, idade, diagnóstico, localização do tumor, tipo e tamanho da ressecção, tipo e tamanho da reconstrução, vasos utilizados para anastomose, complicações pós-operatórias, estado da doença na última consulta, seguimento e tempo até deambulação.
RESULTADOS: No total, 7 pacientes com média de idade de 11,8 anos (variando de 5 anos a 14 anos) foram submetidos a reconstrução de extremidades com retalho livre de fíbula, com 100% de viabilidade e consolidação óssea. As lesões eram localizadas em fêmur, tíbia ou úmero. O tumor mais comum foi o osteossarcoma. O tempo médio de retorno à deambulação foi de 14,7 meses.
CONCLUSÕES: O uso do retalho livre de fíbula é uma excelente alternativa para reconstrução de membros, apresentando alta taxa de consolidação óssea, deambulação precoce, boa funcionalidade e baixa taxa de complicações.
Palavras-chave:
Fíbula. Extremidades. Transplante homólogo. Procedimentos cirúrgicos reconstrutivos.