

Original Article - Year 2012 - Volume 27 -
Mini-abdominoplasty associated with liposuction and lowering of the umbilical scar without pedicular detachment
Lipoaspiração associada à miniabdominoplastia com abaixamento do umbigo sem desinserção umbilical
ABSTRACT
BACKGROUND: Mini-abdominoplasty surgery is considered partial because it only targets the area positioned below the navel without requiring transposition of the umbilicus. It is less invasive than classic abdominoplasty and can achieve a more contoured body in a less invasive manner with a smaller scar and shorter recovery time free of major risks and complications. This article presents a technique in which liposuction around the abdomen and flanks, hips, and back is performed as indicated, with resection of the skin above the pubic zone below the navel without detachment of the pedicle. This technique aims for better presentation of the umbilical scar while addressing supraumbilical flaccidity in the abdomen.
METHODS: Between 2007 and 2010, 24 female patients (aged, 26-55 years) with excess fat in the lower abdomen underwent classic mini-abdominoplasty associated with liposuction.
RESULTS: The results were considered satisfactory by both the patients and surgeon. No major complications occurred during surgery or the transoperative period.
CONCLUSIONS: Mini-abdominoplasty surgery is safe with no severe complications such as infection, pulmonary embolism, and perforation of cavities or skin necrosis. This procedure is effective for the aesthetic treatment of the abdominal region and is easy, fast, and safe to perform.
Keywords: Lipectomy. Abdomen/surgery. Plastic surgery.
RESUMO
INTRODUÇÃO: A miniabdominoplastia é considerada uma cirurgia parcial, pois só trabalha a área que está posicionada abaixo do umbigo, não sendo necessária a transposição do umbigo. É menos invasiva que uma abdominoplastia clássica e consegue obter melhor contorno corporal, de forma menos invasiva, com cicatriz menor, tempo de recuperação um pouco mais curto e livre de grandes riscos e complicações. O objetivo deste estudo é apresentar uma técnica em que são realizadas lipoaspiração de todo o abdome, bem como dos flancos, da cintura e do dorso, conforme indicação, e ressecção em fuso de pele suprapúbica, com abaixamento de umbigo sem a desinserção de seu pedículo, para melhor apresentação de cicatriz umbilical, tratando uma pequena flacidez supraumbilical em abdome.
MÉTODO: Entre 2007 e 2010, 24 pacientes do sexo feminino foram submetidas a miniabdominoplastia clássica associada a lipoaspiração, com idades entre 26 anos e 55 anos, com excesso de tecido adiposo no abdome inferior.
RESULTADOS: Os resultados obtidos foram satisfatórios, sem complicações maiores, e considerados muito bons pelo cirurgião. Não ocorreu nenhuma complicação no transoperatório.
CONCLUSÕES: A cirurgia de miniabdominoplastia mostrou-se segura, não ocorrendo complicações graves, como infecção, embolia pulmonar, perfurações de cavidades ou necrose de pele. A técnica descrita é eficaz no tratamento estético da região abdominal, de fácil execução, rápida e segura.
Palavras-chave: Lipectomia. Abdome/cirurgia. Cirurgia plástica.
Liposuction has evolved over more than 20 years from a less-credited surgery to one of the most widely accepted techniques. For many years, authors have published different techniques that have been put into practice. Changes in the surgery are mainly related to the types of infiltration and caliber of cannula used1.
Abdominoplasty, also known as abdominal dermolipectomy, is the removal of fat localized in the lower abdomen, sagging skin around the umbilical region, and stretch marks located between the navel and pubic hair. It is a functional and aesthetic correction of the abdominal wall2,3.
Abdominoplasty has been performed for more than a century. The first descriptions involved simple incisions without detachment or taking into account the umbilical scar3. However, the surgery was first published in 1899 by Kelly4, who performed a wide transverse resection in the abdomen to correct excess skin and fat in the abdominal wall. Abdominoplasty is a technique that has encouraged the publication of works by plastic surgeons.
In 1905, Grazer et al.5 described the resection of skin and fat with the preservation of the umbilicus for the treatment of large abdominal wall hernias. In 1911, Morestin6 published dermolipectomy procedures involving transverse elliptical excisions. Several modifications of surgical techniques have been proposed since Kelly4; among them are those of Flesch-Thebesius and Weishelmer7, who established transverse infraumbilical resection with preservation of the umbilicus in 1931; Thorek8, who proposed higher abdominoplasty in 1942; and Gonzalez-Ulloa9, who proposed belt lipectomy in 1960.
Some authors such as Callia10, Pontes11, and Pitanguy et al.12 recommend performing the incision lower, aiming to hide the scar below the waistline. Later, Psilakis13 as well as Bozola and Bozola14 published their techniques, proposing the treatment involving the muscle wall of the abdomen.
Mini-abdominoplasty surgery has been used since the late 1960s9. Since 1980, the report of Uebel15 has resulted in widespread use of mini-abdominoplasty in Brazil; the author proposes utilizing a suprapubic elliptical incision together with liposuction of the abdominal wall and flanks, resulting in the total sectioning of the umbilical pedicle and plicature of the rectus abdominis. Later, in 1985, Hakme16 described a procedure in which liposuction is performed with the resection of excess skin and suprapubic muscular plication above and below the umbilicus.
Several authors have contributed to abdominoplasty, aiming to improve the surgery and correct excess skin, subcutaneous adipose tissue, flaccidity, and diastasis of the abdominal wall muscles.
However, in 1998, Avelar17 proposed a liposuction technique of the abdomen that involved a small detachment of skin and fat, leaving a much smaller scar than the classical procedure without intervention on the navel. Besides the advantage of less scarring, it is possible to attain improved treatment of abdominal and adjacent fat through liposuction. In addition, the patient recovers much faster.
The technique established by Saldanha et al.18, which has been used since 2001, is a combination of the concepts of classical abdominoplasty, Avelar's17 technique, and traditional liposuction. Its use reduces the incidence of usual complications such as enlarged scars and seroma, merging the benefits of extensive skin removal and muscle plication with a significant decrease in the panniculus through liposuction.
Despite considerable advances in lipoabdominoplasty with neoumbilicus, we noticed that the scars generated by its construction during these surgeries remain unaesthetic. Surgery is indicated when there is no excess skin, because the scar from where the navel is withdrawn remains in the middle of the hypogastrium.
In mini-abdominoplasty, which involves the detachment and reattachment of the umbilicus in the aponeurosis, the hole resulting from the section of the umbilical pedicle always requires closure with sutures and plication in the midline at least in the mesoumbilical region, making it necessary to peel it open. This maneuver may lateralize the navel in the midline even when utmost care is taken during the reinsertion, because the plication may have a slight lateral deviation.
The original navel does not always exhibit satisfactory results after mini-abdominoplasty involving the detachment of the umbilical pedicle and traction of the infraumbilical skin. This is because the navel does not allow the supraumbilical skin to be pulled and attain good accommodation.
In addition, the juxta-supraumbilical flaccidity and shape of the navel, such as a "sad belly button" (in the horizontal plane), remain when no lowering procedure is performed in mini-abdominoplasties.
Within this context, this article presents a technique in which liposuction is performed around the abdomen, flanks, waist, and back, as indicated. In addition, the suprapubic skin is resected with lowering of the navel but without pedicular detachment for better presentation of the umbilicus in the abdomen.
METHODS
A retrospective study was performed on 24 healthy female patients aged 26-55 years who underwent liposuction involving the technique developed. All operations were performed by the same surgeon between November 2007 and November 2010.
The inclusion criteria adopted for the indications of the proposed technique are as follows:
Patients with slight supraumbilical flaccidity; High umbilicus; Body mass index < 30; Abdominal ultrasonography that ruled out the possibility of umbilical or other hernia or significant muscle diastasis, since plication of the rectus abdominis is not applied because there is no open supraumbilical detachment.
Psychological evaluation is essential from the initial consultation; the aim was to inform the patient of the possibilities and limitations of the surgery as clearly and objectively as possible.
In the first consultation, the areas to be suctioned, technique indicated, scars, and type of anesthesia to be used were outlined. In addition, essential preoperative examinations such as fasting glucose, activated partial thromboplastin time, beta-hCG, complete blood count, urinalysis, and ultrasonography of the abdominal wall were performed.
The surgical procedure was contraindicated in patients who had metabolic, cardiovascular, pulmonary, or coagulation alterations, as well as infections, cancer, inflammation, or pregnancy.
The patients were referred for pre-anesthetic evaluation by the anesthetist who sedated the patient on the day of surgery.
In the second consultation, the results of the preoperative tests were presented. In addition, pre-anesthetic evaluation was performed, and the necessity of treatment before surgery and risks of anemia, infection, and other casual situations were discussed. Any further issues presented by the patient were also resolved.
During the surgical procedure, prophylactic antibiotics were routinely administered: first-generation cephalosporin (cephalothin or cefazolin) was administered at a dose of 2 g immediately after venipuncture; the same dose was repeated every 2 hours during the operation. After surgery, antibiotic therapy was continued orally (cefadroxil or cefaclor) for approximately 4 days.
Marking was performed with the patient conscious and standing for actual delineation of dermolipectomy and visualization of supraumbilical flaccidity. The anterior superior iliac crests were marked with asterisks with the aid of an overhead projector-type pen. A line 5 to 9 cm long, starting from the umbilicus and joining the iliac crests, was drawn.
The midline was marked, starting from the vulvar slit to the xiphoid process. The skin was marked between 9 and 12 cm from the umbilicus to denote the upper and lower limits, and a line located approximately 3 to 5 cm from the vulvar slit was drawn encompassing the Pfannenstiel scar, if any (Figure 1).
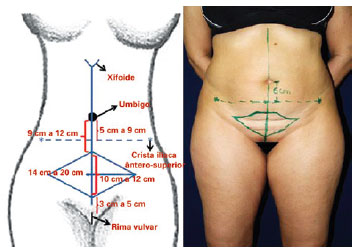
Figure 1 - Marking of the midline, beginning in the vulvar slit to the xiphoid process. Marking of the skin zone (between 9 and 12 cm), including its upper and lower limits by a line located approximately 3 to 5 cm from the vulvar slit encompassing the Pfannenstiel scar, if any.
The lateral limits of such an elliptical or trapezoid skin zone are usually marked from the abdominal midline, approximately 7 to 10 cm away from that line. Thus, the total length of the area is 14 to 20 cm latero-laterally; this zone is approximately 10 to 14 cm wide when extended.
When extended, this zone is approximately 12 × 20 cm. A suprapubic incision was made as low as possible to allow for greater traction and better positioning of the pubic mound, rising laterally under the lower abdomen skin fold or the underwear marks so that the scar is below the waistline; this marking greatly minimizes the occurrence of "ears" on the sides of the scar.
The areas of liposuction were defined according to each case, including the abdomen, flanks, hips, back, mid-thighs, etc. After marking, the patient was transferred to the surgical ward and subjected to anesthetic procedures.
The anesthesiologist routinely performed spinal anesthesia associated with sedation. Anesthesia usually consisted of spinal anesthesia with novocaine and clonidine, along with sedation with propofol, fentanyl, and dormonid.
The tumescent technique used for liposuction, wherein infiltration with vasoconstrictor solution is used (1,000 mL 0.9% saline solution + 1 mg epinephrine solution, 1: 1,000,000 IU).
Openings were made for the introduction of the cannulas: 1 in the area to be resected, 2 on each side near the iliac crests, 1 on top of the umbilicus, and 2 in the posterior dorsum for liposuction. Liposuction was then performed with the patient in the left and right lateral decubitus position, starting with the aspiration of the abdomen and then in the back, flanks, and hips. Cannulas ranging from 2 to 4 mm connected to the vibroliposuction apparatus (Microaire PAL 600) were used for this procedure.
Upon completion of this step of the surgery, total aspirated fat was quantified corresponding to the supernatant volume, and total quantity and volume of injected solution. The total volume of the injected solution ranged from 2 to 5 L; the total volume aspirated, from 3 to 7 L; and the volume of the supernatant, from 1.5 to 5 L.
After completing lipoaspiration, the actual mini-abdominoplasty was initiated. The patient was placed in the supine position, keeping the back of the table elevated at 30 degrees. New antisepsis and surgical fields were placed at this time. The markings were reinforced with methylene blue. Only the previously delineated area was resected, removing the enclosed resection area of the muscular aponeurosis (Figure 2).

Figure 2 - Resection of the skin. Appearance of the navel before attachment.
The mid-region below the umbilicus was detached with a scalpel blade no. 15 while the assistant surgeon performed careful electrohemostasis until reaching the umbilical pedicle. Then, the pedicle was skeletonized using a clampmounted gauze or a compress, keeping it attached to the aponeurosis but free from adjacent tissues (Figure 3).
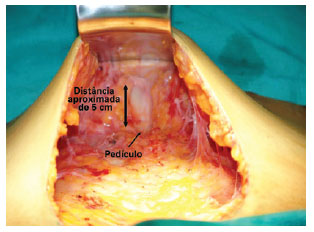
Figure 3 - Detachment of the pedicle. After liposuction, the pedicle measures up to 7 cm. It should be noted that the navel is a sac-shaped structure with a depth of approximately 2 cm and continues to the anterior abdomen with a fibrous pedicle.
The pedicle measured approximately 7 cm after liposuction. It should be noted that the navel is a sac-shaped structure with a depth of approximately 2 cm and continues to the anterior abdomen with a fibrous pedicle.
The region where the anterior portion of the umbilical pedicle would be repositioned was demarcated with methylene blue at a location equivalent to the bottom of the umbilical sac, and is then fixed 4 cm or more below its previous location in the midline of the anterior abdominal aponeurosis (i.e., linea alba); a height of 2 cm above the iliac crests (the bottom point) was always maintained (Figure 4).

Figure 4 - Marking the new fixation of the anterior portion of the pedicle. Marking using methylene blue where the anterior portion of the umbilical pedicle will be repositioned, equivalent to the bottom of the umbilical sac; it is then fixed 4 cm or more below its previous location in the midline of the anterior abdominal aponeurosis (i.e., linea alba). A height of 2 cm above the iliac crests (the previous point) is always maintained.
Fixation was performed with 3 to 4 simple 4-0 nylon sutures in the aponeurosis, which allowed the aesthetic improvement of the navel (Figures 5 and 6).
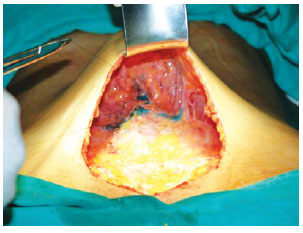
Figure 5 - Suturing of the umbilical pedicle in the aponeurosis. Fixing was usually performed with 3 to 4 simple sutures in the aponeurosis, which allows the aesthetic improvement of the navel by shaping it, including making it more or less shallow or open, as desired.
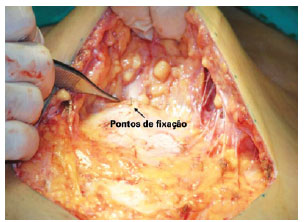
Figure 6 - Navel already attached in the lower portion, lowered by 3 to 5 cm. Fixing the navel in place previously marked with methylene blue (attachment points).
Rigorous hemostasis was performed. The abdomen was closed on 3 levels: in the deepest layer with 3-0 nylon, the subdermis with 4-0 colorless nylon, and intradermally with 4-0 monocryl. Therefore, there was no need to remove the sutures in the area of skin resection except for those at the points of liposuction, which were made with 5-0 nylon. Drains were not usually used.
Clexane® 20 mg was used routinely to prevent deep vein thrombosis. With a recommendation of early ambulation (4 hours after surgery), the patients were discharged on the same day of surgery. The surgical procedure lasted an average of 150 minutes, depending on the amount of fat and fat tissue to be removed.
The surgery was completed with occlusive dressing fitted with collagenase + chloramphenicol using a small piece of gauze inside the navel to help maintain its shape, which was changed daily for 45 days. Compression/modeling garments were also worn.
The patients were instructed regarding ambulation and mobility of the lower limbs. Drainage was performed by the physiotherapy team starting 5 days after the procedure. The patients returned 7, 15, and 30 days after surgery for wound dressing and guidance and after 4 and 6 months thereafter.
We conducted a moderate compression of the abdomen and other aspirated areas with an elastic mesh modeler, which was used by the patient for 45 days to aid tissue accommodation. Silicone or microporous adhesive tapes were used routinely for 2 months to prevent enlargement and hypertrophy of the scars.
The scar generated from this procedure was observed as a low arched line in the pubic area and laterally toward the iliac spines, hidden by a bikini or underwear.
Figures 7 to 10 illustrate some cases of this study.

Figure 7 - In A, preoperative appearance. In B, 2-month postoperative appearance.

Figure 8 - In A, Preoperative appearance. In B, 40-day postoperative appearance.

Figure 9 - In A, Preoperative appearance. In B, 4-month postoperative appearance.

Figure 10 - In A, preoperative appearance. In B, 2-month postoperative appearance.
RESULTS
The technique presented here was developed on the basis of previous procedures with the aim of providing better aesthetic results to the navel and avoiding neo-omphaloplasty. Mini-abdominoplasty was performed in patients with slight supra- and infraumbilical flaccidity, with the supraumbilical flaccidity being decisive.
The procedure aims to remove the skin below the umbilicus and treat supraumbilical flaccidity without requiring neonavel or detachment of the umbilical pedicle from the aponeuroses. It also takes into account that the detachment of the navel and reattachment in the aponeuroses after suturing of the sectioned umbilical pedicle always requires plication in the midline, at least in the mesoumbilical region, making open supraumbilical detachment necessary.
The proposed technique aims to minimize surgical time and surgical manipulation, and especially avoid supraumbilical detachments.
The mean duration of the mini-abdominoplasty was 150 minutes, which is justified by the size of the aspirated area and aspirated volume on each occasion as well as the fact that no intraoperative complications were reported.
Postoperatively, fluid replacement therapy, blood pressure control, and pulse should be maintained. Stimulation of movements with the feet on the bed, and walking as early as possible as the procedure and anesthesia allow should also be performed. Analgesia control via parenteral or oral intake and return to oral liquid intake should be pursued as soon as possible.
Regarding the degree of patient satisfaction, 95% stated their expectations were met and 100% would undergo the procedure again and refer it to others.
After 6 months, all patients presented scars that were considered aesthetically good or excellent except one who developed hypertrophy; after treatment with corticosteroids and silicone tape, the results improved and were considered good by the patient.
Intercurrences and Complications
No areas of necrosis were observed. Seroma formed in 3 patients, which was punctured in the clinic 7 days after surgery.
One patient developed hypertrophic scarring, which was treated with topical steroids. There were no cases of infection, hematoma, or wound dehiscence that required surgical intervention. No cases of deep vein thrombosis or pulmonary embolism were detected clinically.
DISCUSSION
Abdominal lipectomy was first described by Demars and Marx in 1890 19. This term was subsequently changed to abdominoplasty and refers to surgical procedures involving a resection of skin and excess subcutaneous tissue. It may be associated with several other procedures and techniques that act on muscle and aponeuroses as well as complementary procedures in subcutaneous tissue, such as liposuction.
At present, with the emergence of new techniques, liposuction can be associated with plastic surgery of the abdomen, which is confirmed in the techniques of Saldanha et al.18 and Avelar17; the latter is associated with the detachment and lowering of the umbilicus, which is at odds with previous thinking that that the procedures could not be combined because of the risk of compromising the nutrition of the abdominal skin.
The combination of abdominoplasty with liposuction is a technically viable alternative; the small increase in morbidity associated with these procedures is not a contraindication. Although there has certainly been a significant increase in the duration of the combined surgery, this has not resulted in increased infection rates.
Abdominoplasty and liposuction can be combined with ease as long as the patient's clinical conditions permit it and there is good understanding and rapport between staff and patient, clarifying the patient's possibilities, needs, and risks.
CONCLUSIONS
No clinical signs of overdose or side effects were observed in the patients evaluated. The volume of saline solution used in combination with epinephrine (1:1,000,000) was considered very safe.
The therapeutic results were assessed clinically and photographically and considered very good by both the surgeon and patients. Surgery performed with this technique was considered quite safe; there were no complications during surgery, and postoperative complications were treated appropriately.
Evaluating the patients' emotional attitude and clarifying the possibilities and limitations of this procedure increase the chance of meeting the patients' expectations. This contributes to improved self-esteem, happiness, a sense of well-being, and balance between physical and emotional health.
Liposuction associated with abdominoplasty aims to improve body contours in a specific area of the abdomen. The procedure involves the removal of excess skin below the umbilicus, significantly improving supraumbilical flaccidity, the shape of the navel, and waist definition. Excess fat around the abdomen is removed, and the umbilicus is repositioned with great aesthetic improvement of the scar. Moreover, the surgery is combined with liposuction in order to achieve even more aesthetically satisfactory results.
REFERENCES
1. Carvalho GB, Ribeiro VMN, Barbosa RCC, Coelho EM, Ferreira AC. Lipoaspiração. Residência do Hospital Geral de Fortaleza. 2003;12(2):23-4.
2. Graf R, Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;30(1):1-8.
3. Grazer FM, Klingbeil JR. Body image: a surgical prospective. St. Louis: Mosby; 1980. p. 146-9.
4. Kelly HA. Report or gynecological cases. JOMS Hopkins Med J. 1899;10:197.
5. Grazer FM, Gaudet TS, Morestin A. Abdominoplasty. In: McCarthy JG, ed. Plastic surgery. Vol. 6. Philadelphia: Saunders; 1990. p. 3929-63.
6. Morestin A. La restauration de la paroi abdominale par résection etendue des teguments et la graisse sous-cutanée et le plissements des aponévroses superficielles envisagécomme complément de la cure radicale des hernies umbilicales [Thése]. Paris; 1911.
7. Flesch-Thebesius M, Weishelmer K. Die operation des Hangebauxhes. Chirurg. 1931;3:841.
8. Thorek M. Plastic surgery of the breast and abdominal wall. Springfield: Charles C. Thomas; 1942. p. 111.
9. Gonzalez-Ulloa M. Belt lipectomy. Br J Plast Surg. 1960;13:179-86.
10. Callia WEP. Contribuição para o estudo da correção cirúrgica do abdome em pêndulo e globoso: técnica original [tese de doutoramento]. São Paulo: Faculdade de Medicina, Universidade de São Paulo; 1965.
11. Pontes R. Plástica abdominal: importância de sua associação a hérnias incisionais. Rev Bras Cir. 1965;52(2):85-91.
12. Pitanguy I, Yabar AA, Pires CEB, Matta SR. Aspectos atuais em lipectomia abdominal. Rev Bras Cir. 1974;64(5/6):147-67.
13. Psillakis J. Abdominoplasty: some ideas to improve results. Aesth Plast Surg. 1978;2:205-15.
14. Bozola R, Bozola AC. Abdominoplastias. In: Melega JM, ed. Cirurgia plástica: fundamentos e arte. Cirurgia estética. São Paulo: MEDSI; 2003.
15. Uebel CO. Mini abdominoplasty: a new approach for the body contouring. New York: Annals 9th Congress ISAPS; 1987.
16. Hakme F. Technical details in the lipoaspiration associated with liposuction. Bras Cir. 1985;75(5):331-7.
17. Avelar JM. Uma nova técnica de abdominoplastia: sistema vascular fechado de retalho subdérmico dobrado sobre si mesmo, combinado com lipoaspiração. Rev Bras Cir. 1999;88/89:3-20.
18. Saldanha OR, Pinto EBS, Matos Jr WN, Lucon RL, Magalhães F, Bello EML, et al. Lipoabdominoplastia: técnica Saldanha. Rev Soc Bras Cir Plást. 2003;18(1):42-6.
19. Storck R. Mini abdominoplastia. ACM Arq Catarin Med. 2000;29 Supl 1:250-1.
Plastic Surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery, Divinópolis, MG, Brazil.
Correspondence to:
Gustavo Gonzalez Assumpção
Avenida Getulio Vargas, 440 - Centro
Divinópolis, MG, Brazil - CEP 35500-024
E-mail: gustzalez@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 23, 2012
Article accepted: July 23, 2012
This study was performed at the Equilíbrio Clínica de Cirurgia, Divinópolis, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter