

Original Article - Year 2012 - Volume 27 -
Vertical abdominoplasty for treatment of excess abdominal skin after massive weight loss
Abdominoplastia vertical para tratamento do excesso de pele abdominal após perdas ponderais maciças
ABSTRACT
BACKGROUND: Bariatric surgeries are becoming increasingly common in the treatment of morbidly obese patients. The enormous weight loss resulting from these procedures causes excessive skin and subcutaneous tissue throughout the body, especially in the abdominal region. The objective of this study was to present the technique of vertical abdominoplasty as an alternative for resection of excess skin in ex-obese patients.
METHODS: We retrospectively evaluated the records of 40 patients who underwent vertical abdominoplasty between 2004 and 2009. The degree of patient satisfaction was assessed through a subjective scale, with scores ranging from 0 to 10.
RESULTS: Twenty-five percent of the patients had minor complications (3 seromas, 3 minor dehiscences, and 5 hypertrophic scars), which were all treated on an outpatient basis. Sixty-seven percent of the patients reported high satisfaction and considered their results as good (grades 7 or 8) or excellent (grades 9 or 10).
CONCLUSIONS: The vertical abdominoplasty technique appears to be a new option for the treatment of excess abdominal skin in ex-obese patients.
Keywords: Obesity. Bariatric surgery. Weight loss. Abdomen/surgery.
RESUMO
INTRODUÇÃO: As cirurgias bariátricas são cada vez mais frequentes no tratamento dos pacientes portadores de obesidade mórbida. A grande perda ponderal decorrente desses procedimentos causa excesso de pele e de tecido subcutâneo em todo o corpo, especialmente na região abdominal. O objetivo deste trabalho é apresentar a técnica de abdominoplastia vertical como alternativa para a ressecção do excesso de pele nesses pacientes.
MÉTODO: Foram avaliados, retrospectivamente, os prontuários de 40 pacientes submetidos ao procedimento entre 2004 e 2009. O grau de satisfação dos pacientes foi avaliado através de escala subjetiva, com notas variando de 0 a 10.
RESULTADOS: Vinte e cinco por cento dos pacientes apresentaram pequenas complicações, sendo 3 seromas, 3 pequenas deiscências e 5 cicatrizes hipertróficas, todas tratadas ambulatorialmente. Dois terços dos pacientes relataram alto grau de satisfação, considerando seus resultados bons (notas 7 ou 8) ou ótimos (notas 9 ou 10).
CONCLUSÕES: A técnica de abdominoplastia vertical aparece como uma nova opção para o tratamento do excesso de pele abdominal em pacientes ex-obesos.
Palavras-chave: Obesidade. Cirurgia bariátrica. Perda de peso. Abdome/cirurgia.
Obesity is now a pandemic causing significant health risks to a major part of the world's population. Bariatric surgeries were introduced as an alternative treatment for the morbidly obese and are becoming increasingly used. Patients undergoing these surgeries experience significant weight loss and naturally evolve to have excess skin and subcutaneous tissue throughout their body. This population is increasingly seeking the help of plastic surgeons to improve the body contour, and knowledge of surgical alternatives for the treatment of these patients is very important1.
Abdominoplasty, mammoplasty, brachioplasty, and dermolipectomy in the thigh are the most popular procedures used in our center2. The removal of excess skin and subcutaneous tissue in the abdominal region can be achieved via a low transverse incision (classical abdominoplasty), a combination of transverse and vertical incisions (anchor abdominoplasty), or, more rarely, with an incision in the mammary fold (reverse abdominoplasty)3-6.
Since 2004, some patients have been treated at our institution after massive weight loss by resection of excess tissue from the abdominal region through a unique vertical incision. Although there are reports in the literature regarding the use of these incisions for esthetic abdominoplasty7 and correction of giant hernias of the abdominal wall or tumor resections8, we found no reports on the use of this technique in the treatment of patients after bariatric surgery.
The objective of this study was to present this alternative vertical technique for the resection of excess abdominal skin after bariatric surgery and describe the results in 40 patients.
METHODS
A retrospective review of the medical records of 40 patients with a history of bariatric surgery undergoing vertical abdominoplasty between 2004 and 2009 in the Hospital of the Faculty of Medicine, University of São Paulo, was carried out. The variables analyzed were age, time between bariatric surgery and abdominoplasty, body mass index (BMI) before and after bariatric surgery, use of drains, length of stay, and postoperative complications.
Patients were contacted and questioned about postoperative pain and satisfaction with the esthetic outcome of the surgery; both of these variables were assessed on a numerical scale (0 to 10), with grades 0-4 considered as poor outcome, grades 5 and 6 as regular outcome, grades 7 and 8 as good outcome, and grades 9 and 10 as excellent outcome.
Technique Description
The vertical incision was marked by gripping the excess abdominal skin vertically (Figure 1), with the patient in a supine position. To accomplish compensation for excess skin in the craniocaudal direction, the final marking was drop shaped with a wide base encompassing all of the excessive skin in the region of the hypogastrium, which was in contrast to the classic spindle shape (Figure 2).

Figure 1 - Manual extension of excess abdominal skin for marking the vertical incision.
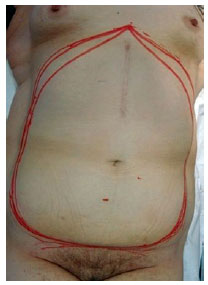
Figure 2 - Preoperative marking.
With the patient under general anesthesia, en bloc resection of the skin was performed following the preoperative marking, without additional detachments. The preaponeurotic plane was the deepest limit of the resection. The navel was separated from the surgical piece before its resection and maintained by abdominal aponeurosis (Figure 3). In all patients, abdominal aponeurosis plication in 2 planes with nonabsorbable suture was then carried out (Figure 4). This enabled not only correction of diastasis of the rectus abdominis muscles, which is always present in these patients, but also allowed reduction of the tension on the surface planes of the sutures. In the most caudal position of the scar, some wrinkling of the tissue was normal. In severe cases, compensation was accomplished with a small horizontal component.
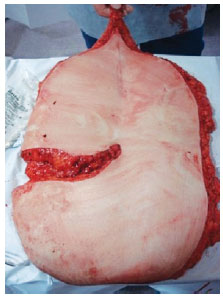
Figure 3 - Surgically excised piece.
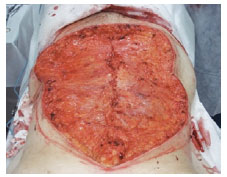
Figure 4 - After resection and plication.
Closure was performed in 3 layers by using absorbable thread. The navel was repositioned into the anatomical position, as determined by the projection of its position deep in the skin flaps. The use of drains was assessed on a case-by-case basis at the discretion of the surgeon.
All patients were instructed to use mesh compression in the abdominal region from the immediate postoperative period up to 2 months after surgery.
RESULTS
The mean age at the time of abdominoplasty was 43.6 years (range, 18 to 58 years). Most patients were women (34 women and 6 men). On average, the procedure was performed 2.8 years (range, 1 to 5 years) after gastroplasty.
All patients underwent significant weight loss after bariatric surgery, with an average loss of 39% of their initial weight (range, 25 to 48%). Mean BMI at the time of abdominoplasty was 27.4 kg/m2 (range, 22 to 32 kg/m2).
The mean hospital stay was 2.72 days (range, 1 to 4 days), and there were no serious complications such as thrombosis, systemic disorders, or death.
In 57.5% of patients, drains were used postoperatively. Minor complications were noted in 10 (25%) patients, and included 3 cases of seroma, 3 cases of minor dehiscence, and 5 cases of hypertrophic scarring. The 3 seromas occurred in patients who had their surgical sites drained. Patients with minor dehiscence were treated as outpatients with simple dressings until their injuries had healed by secondary intention. Three of these patients underwent minor revisions of their scars under local anesthesia. Figures 5 and 6 show the results obtained in 2 patients in this series.

Figure 5 - In A, preoperative appearance, frontal view. In B, postoperative appearance 6 months after vertical surgery, frontal view.
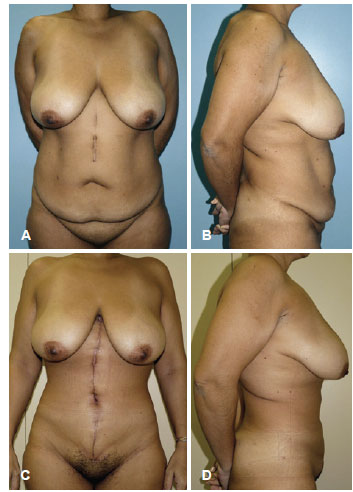
Figure 6 - In A and B, preoperative appearance, in frontal and side views, respectively. In C and D, postoperative appearance 6 months after vertical abdominoplasty, frontal and side views.
The average score on the analog pain scale was 5 points, with wide variation among patients. The average satisfaction level was 7.75 points, with 66% of patients having good or excellent assessment of outcome (score equal or above 7).
DISCUSSION
Traditionally, tummy tucks are performed via low transverse incisions in order to hide the resulting scars in the patient's underwear or swimwear, leading to better esthetic acceptance by patients. After major weight loss, especially in patients undergoing bariatric surgery, there is a lot of excess skin all over the body, particularly in the abdominal region, which is accompanied by pronounced sagging of the skin. This excess tissue is visible in both the craniocaudal direction and the lateral-lateral direction, preventing its compensation with a single horizontal scar. Thus, anchor or fleur-de-lis incisions, with their associated vertical and horizontal incisions, have become extremely popular for abdominoplasty in patients with excess abdominal skin after major weight loss. However, these incisions are subject to complications, primarily in the region of confluence of the scars, which is known as the T area.
The technique presented in the current paper results in a single vertical scar, which is less esthetically acceptable and more noticeable as compared to the transverse scar resulting from removal of excess skin in the abdominal region after drastic loss of weight. Although most bariatric surgeries are currently performed laparoscopically, many patients already had a vertical scar in the upper abdomen resulting from open bariatric surgery. In one patient in this series, the approach described allowed the complete resection of infected and chronically exposed prosthetic material (Figure 7). As compared to the anchor approach, vertical resection of excess skin did not involve the need of a horizontal component, and was associated with a lower risk of complications. Moreover, the resulting scar is difficult to disguise in the underwear and owing to the large amount of excess tissue cleared perpendicular to the lines of force of the abdominal skin, the technique tends to lead to the formation of a slightly extended and winding scar.

Figure 7 - In A and B, preoperative appearance, in frontal and side views, respectively. In C and D, postoperative appearance 6 months after vertical abdominoplasty, in frontal and side views, respectively. This patient showed chronic exposure of mesh used to correct an incisional hernia. The mesh was removed and the hernia was corrected by plication of the abdominal wall.
The complications encountered in this series were all minor and required outpatient treatment only. The seromas observed in some cases suggest that the use of drains in these patients was not effective. In fact, as there is no additional detachment and subcutaneous tissue at the edges of the wound is closed in multiple planes, the dead space resulting from the procedure is reduced and small collections in localized regions of the wound will form localized cysts, which will not be effectively drained if the drain is placed in another plane.
The difficulty in objectively evaluating the results of plastic surgery is well known, because the esthetic component of surgery is the main aim sought by patients. Although we did not have the opportunity to analyze the results with a greater degree of evidence in the present study, for example the use of a standardized scale to assess the evaluations made by independent observers9, we asked the patients to describe their satisfaction on a scale of 0 to 10 (subjective data). The degree of satisfaction was high, with 67% of the patients considering their results as good or excellent, according to subjective criteria of evaluation. Despite the low strength of evidence of the evaluation method used, our data showed that these patients were satisfied with the results of surgery even with a vertical scar visible in the abdomen. In general, we found that after drastic weight loss, patients mostly seek an improved body contour and relief from complications resulting from a large amount of excess skin, such as rashes and skin parasites. The proposed technique has allowed us to achieve these goals. Objective comparison of this technique with other treatments available for these patients will bring us additional information about its validity and directions. These studies are in progress.
CONCLUSIONS
Vertical abdominoplasty is a new alternative for the treatment of excess skin and subcutaneous tissue after massive weight loss in patients who have previously undergone bariatric surgery. Although the resulting scar is more visible than that observed in classical abdominoplasty, good results and a low risk of complications were observed in this series of 40 patients. The degree of satisfaction reported by patients highlights the vertical abdominoplasty technique as an interesting option for the esthetic treatment of the abdominal region in ex-obese patients.
REFERENCES
1. van der Beek ES, Te Riele W, Specken TF, Boerma D, van Ramshorst B. The impact of reconstructive procedures following bariatric surgery on patient well-being and quality of life. Obes Surg. 2010;20(1):36-41.
2. Orpheu SC, Coltro PS, Scopel GP, Saito FL, Ferreira MC. Body contour surgery in the massive weight loss patient: three year-experience in a secondary public hospital. Rev Assoc Med Bras. 2009;55(4):427-33.
3. Persichetti P, Simone P, Scuderi N. Anchor-line abdominoplasty: a comprehensive approach to abdominal wall reconstruction and body contouring. Plast Reconstr Surg. 2005;116(1):289-94.
4. Dellon AL. Fleur-de-lis abdominoplasty. Aesthetic Plast Surg. 1985;9(1):27-32.
5. Agha-Mohammadi S, Hurwitz DJ. Management of upper abdominal laxity after massive weight loss: reverse abdominoplasty and inframammary fold reconstruction. Aesthetic Plast Surg. 2010;34(2):226-31.
6. Costa LF, Manta AM, França AS, Cavalcante HA, Nahon M. Abdominoplastia vertical modificada em pacientes ex-obesos. Rev Soc Bras Cir Plást. 2003;18(3):71-4.
7. Fischl RA. Vertical abdominoplasty. Plast Reconstr Surg. 1973;51(2):139-43.
8. Sugarbaker PH. Vertical abdominoplasty. J Surg Oncol. 2001;78(3):217-9.
9. Salles AG, Ferreira MC, Remigio AFN, Gemperli R. Evaluation of aesthetic abdominal surgery using a new clinical scale. Aesthetic Plast Surg. 2012;36(1):49-53.
1. Plastic Surgeon, associate physician of the Plastic Surgery Department of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil.
2. Plastic Surgeon, teaching physician of the Plastic Surgery Department of the HC-FMUSP, São Paulo, SP, Brazil.
3. Resident Physician of the Plastic Surgery Department of the HC-FMUSP, São Paulo, SP, Brazil.
4. Full professor of the Plastic Surgery Department of the HC-FMUSP, São Paulo, SP, Brazil.
Correspondence to:
Bernardo Nogueira Batista
Rua Joaquim Floriano, 466 - cj. 1.708 - Itaim Bibi
São Paulo, SP, Brazil - CEP 04534-002
E-mail: bernardonb@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 7, 2011
Article accepted: August 7, 2012
This study was performed at the Plastic Surgery Department of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter