

Original Article - Year 2012 - Volume 27 -
Use of skin flaps for nasal reconstruction after neoplastic resection
Uso de retalho cutâneo para reconstrução nasal após ressecção neoplásica
ABSTRACT
BACKGROUND: Nasal reconstruction is always a challenge for the plastic surgeon. Loss of nasal mass is mainly caused by resection of skin cancers. Among the several available alternatives for covering the skin, skin flaps are the first cosmetic and functional choice. This study has 2 objectives: (1) to report the experiences of the Plastic Surgery Service of São Lucas Hospital of the Pontifical Catholic University of Rio Grande do Sul (Porto Alegre, RS, Brazil) in the reconstruction of nasal mass losses that resulted from tumor resection and (2) to describe the most commonly used skin flaps used for defect repair according to the anatomic subunit.
METHODS: This study analyzed 103 nasal skin flaps used in the reconstruction of 102 nasal mass losses that resulted from tumor resection in 96 patients who underwent surgery between December 2008 and December 2011. Mass losses were mapped according to the anatomic subunits described by Burget and Menick. Moreover, the number of times each strategy was chosen for the reconstruction of the different subunits was recorded.
RESULTS: Most of the patients were men (51%), and the average age of the analyzed group was 64.7 years. Basal cell carcinoma was the most prevalent skin cancer (85.3%), followed by squamous cell carcinoma (5.9%). The bilobed flap was commonly used for nasal alar lobule reconstruction (44%); V-Y advancement for the lateral region (72%); extended glabellar for the nasal dorsum (59.2%); bilobed for the nasal tip (46.2%); and glabellar for the nasal roof as well as in the cases mentioned above.
CONCLUSIONS: Several surgical procedures are used for nasal reconstruction following tumor resection. The most suitable strategy should be chosen according to the patient in order to maintain the contours and nasal anatomy, as described by Burget and Menick.
Keywords: Surgical flaps. Nose/surgery. Nose neoplasms. Skin neoplasms.
RESUMO
INTRODUÇÃO: A reconstrução nasal é sempre desafiadora para o cirurgião plástico. As perdas de substância nasal são causadas principalmente por ressecção de neoplasias de pele. Existem muitas alternativas para cobertura cutânea e os retalhos cutâneos constituem a melhor opção, tanto cosmética como funcional. O objetivo deste trabalho é relatar a experiência do Serviço de Cirurgia Plástica do Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (Porto Alegre, RS, Brasil) na reconstrução de perdas de substância do nariz secundárias a ressecção oncológica, descrevendo os retalhos cutâneos mais utilizados para cobertura dos defeitos segundo a subunidade anatômica.
MÉTODO: Foi realizada análise de 103 retalhos cutâneos nasais utilizados para reconstrução de 102 perdas de substância secundárias a neoplasia, em 96 pacientes operados no período de dezembro de 2008 a dezembro de 2011. As perdas de substância foram mapeadas de acordo com as subunidades anatômicas descritas por Burget & Menick, sendo registrado o número de vezes em que cada opção de reconstrução foi utilizada em cada subunidade.
RESULTADOS: A maioria dos pacientes era do sexo masculino (51%) e a média de idade do grupo estudado foi de 64,7 anos. Dentre os tumores cutâneos, o carcinoma basocelular foi o mais frequente (85,3%), seguido de carcinoma espinocelular (5,9%). Na asa nasal, o retalho mais utilizado foi o bilobado (44%); na região lateral, o retalho de avançamento em V-Y (72%); no dorso nasal, o retalho glabelar estendido (59,2%); na ponta, o retalho bilobado (46,2%); e no teto nasal, o retalho glabelar, utilizado em todos os casos.
CONCLUSÕES: São múltiplas as opções cirúrgicas para reconstrução do nariz após cirurgia oncológica, devendo-se escolher a mais adequada para cada caso, respeitando-se os contornos e a anatomia nasal, de acordo com os princípios de Burget & Menick.
Palavras-chave: Retalhos cirúrgicos. Nariz/cirurgia. Neoplasias nasais. Neoplasias cutâneas.
The nose is an anatomical subunit located in the central third of the face and is of major importance for the phenotypic characterization of an individual. The nose is formed by 3 layers: the mucosa, the osteocartilaginous framework, and the skin. Its surface is full of curves and grooves.
Mass losses commonly occur after tumor resection and trauma1-3. Cosmetic and functional reconstruction of nasal defects is a challenge for the cosmetic surgeon because several surgical procedures have been described and are available for correcting different skin defects. Burget and Menick4 revolutionized nasal reconstruction surgery by introducing the concept of aesthetic subunits of the nose. These subunits are based on differences in elasticity, color, shape, and texture of the skin, and this concept has contributed to improvements in nasal surgery.
The objective of this study is to report the experiences of the Plastic Surgery Service of São Lucas Hospital of the Pontifical Catholic University of Rio Grande do Sul (Porto Alegre, RS, Brazil) in reconstructing nasal mass losses after tumor resection and to describe the skin flaps that are commonly used for defect repair according to the anatomic subunit.
METHOD
Analysis of 103 nasal skin flaps used in the reconstruction of 102 nasal mass losses due to tumor resection was performed in 96 patients who underwent surgery between December 2008 and December 2011.
Mass losses were mapped according to the anatomic subunits described by Burget and Menick4 as follows: roof, dorsum, lateral side wall, tip, alar lobule, and columella (Figure 1).
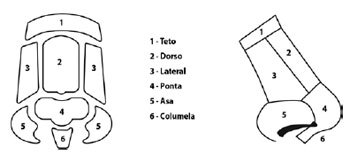
Figure 1 - Nasal subunits according to Burget and Menick4.
The number of times that each strategy was chosen for the reconstruction of the different subunits was recorded.
RESULTS
This study included 96 patients, 49 of which (51%) were men and 47 (49%) were women. The average age of the patients was 64.7 years (range, 39 to 87 years). Of the skin tumors, basal cell carcinoma was the most prevalent (85.3%), followed by squamous cell carcinoma (5.9%), actinic keratosis (3.9%), solar elastosis (2.9%), nodular hidradenoma (1%), and acanthoma (1%) (Table 1).
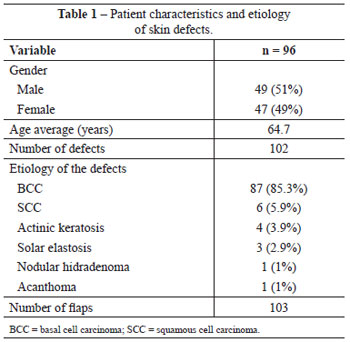
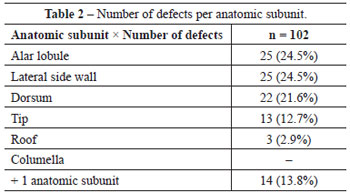
The most frequently reconstructed anatomic subunits of the nose were the lateral side wall and nasal alar lobules in 25 (24.5%) patients each, followed by the nasal dorsum in 22 (21.6%) patients, the tip in 13 (12.7%) patients, and the roof in 3 (2.9%) patients. More than 1 aesthetic subunit was involved in 14 (13.8%) patients, and these cases were defined as complex. Nasal columella tumors were not found in any of the patients (Table 2). Skin involvement was present in 91 patients, skin and cartilage in 5 patients, and skin combined with cartilage and mucosa in 6 patients.
Among the 25 nasal alar lobule mass losses, 11 (44%) were reconstructed using bilobed flaps, 7 (28%) with V-Y advancement flaps, 6 (24%) with nasolabial flaps, and 1 (4%) with a frontal flap.
Out of 25 lateral mass losses, a V-Y advancement flap was used in 18 (72%) patients (Figure 2), a bilobed flap in 4 (16%), a glabellar flap in 2 (8%), and an extended glabellar flap in 1 (4%). Of the 22 nasal dorsum mass losses, 13 (59.2%) were reconstructed using extended glabellar flaps (Figure 3), 4 (18.2%) using bilobed flaps, 3 (13.6%) using rhomboid flaps, 1 (4.5%) using a V-Y advancement flap, and 1 (4.5%) using a frontal flap.

Figure 2 - V-Y advancement flap for repair of a defect in the left lateral subunit. In A, detail of the lesion. In B, appearance after confection of the flap.

Figure 3 - Extended glabellar flap for repair of a defect in the nasal dorsum. In A, detail of the lesion. In B, appearance after confection of the flap.
A bilobed flap (Figure 4) was used for the reconstruction of the nasal tip in 6 (46.2%) patients, a frontal flap in 3 (23.1%), an extended glabellar flap in 4 (30.7%) and a glabellar flap in 3 (100%) (Figure 5 and Table 3).

Figure 4 - Bilobed flap for repair of a defect in the nasal tip. In A, detail of the lesion. In B, appearance after confection of the flap.

Figure 5 - Glabellar flap for repair of a defect in the nasal roof. In A, detail of the lesion. In B, appearance after confection of the flap.
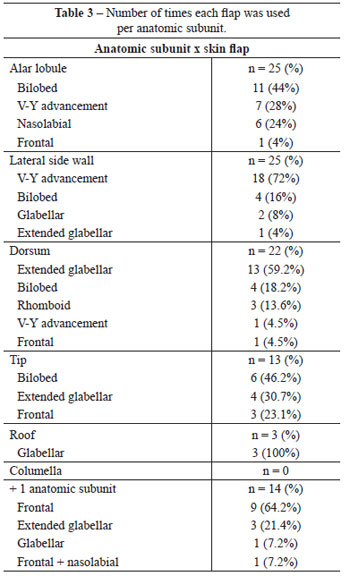
Of the 14 mass losses classified as complex, 9 (64.2%) were reconstructed using a frontal flap (Figure 6), 3 (21.4%) using an extended glabellar flap, 1 (7.2%) using a glabellar flap, and 1 (7.2%) using a combination of frontal and glabellar flaps (Table 3).
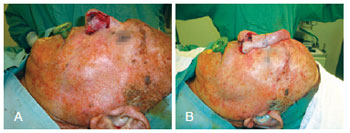
Figure 6 - Paramedian frontal flap to repair complex defects involving the alar lobule, dorsum, and left nasal lateral wall. In A, detail of the lesion. In B, appearance of the rotated flap.
DISCUSSION
Although skin flaps used for nasal reconstruction present high versatility in terms of their application, some flaps may be adapted according to the necessity of each patient3. Skin flaps are preferred to skin grafts for reconstructing mass losses because of their higher similarity to the color and the texture of the skin5,6. Moreover, removal of skin from other locations is not necessary with the use of skin flaps, thus precluding a second surgical wound and avoiding the extensive care required by skin grafts.
Skin cancers develop mainly in men and particularly affected the nose7-12. The average age of the patients included in this study (64.7 years) is in agreement with the literature because most individuals presenting with skin cancer are over 60 years of age, with a higher prevalence in the 7th decade of life13.
Among facial skin cancers, 30% to 35% develop in the nose14-16. According to the literature, skin cancers are etiologically divided as basal cell carcinomas (70%) and squamous cell carcinomas (25%)13. In this study, most of the nasal tumors were basal cell carcinomas (85.3%) followed by squamous cell carcinomas (5.9%).
Overall, 103 skin flaps were used for the correction of 102 mass losses. In 1 of these patients, 2 flaps were required to cover the skin adequately.
This study adopted the principles of aesthetic subunits for the reconstruction of nasal cutaneous defects introduced by Burget and Menick4. When more than 50% of the aesthetic subunits were simultaneously involved, it became necessary to reconstruct the entire subunit.
Distinct skin flaps are currently used for the reconstruction of the nasal alar lobule. Many authors prefer the nasolabial or V-Y advancement flap as a first option1-3. In this study, the bilobed transposition flap (44%) was most commonly used, followed by V-Y advancement (28%) and nasolabial (24%) flaps. All flaps described herein have been shown to be safe and to provide satisfactory aesthetic results. The advantage of the bilobed flap, which was the most frequently used flap in our patients, is that it can be used in a simple surgery during a single procedure. Moreover, in contrast to nasolabial flaps, the functional and cosmetic outcomes of this flap are satisfactory, these flaps are and well accepted by patients.
In this study, satisfactory post-operative results were obtained in 72% of patients who underwent nasal reconstruction of the lateral walls with V-Y advancement flaps. Although the incision typically crosses the nasofacial groove, an important anatomic structure of the face, most of the patients reported satisfaction with the final aesthetic result. Uchinuma et al.17 reported several advantages of using V-Y advancement flaps for defect repairs of the nasal lateral wall. To reach this conclusion, these authors analyzed the nasal morphology, including color, skin texture, and scars of local donors.
Concerning the nasal dorsum, satisfactory aesthetic and functional results were obtained in more than 50% of the procedures performed using extended advancement glabellar skin flaps. The patients were satisfied with their final appearance despite the extent of the incision caused by these flaps. In the literature, the most highly recommended flaps for the reconstruction of the nasal dorsum are glabellar or extended glabellar flaps. These types of flaps are reportedly preferred by Guo et al.3, who used an algorithm for the treatment of nasal defects with local skin flaps, and by Woodard et al.18. The bilobed flap was used in a small number of patients (18.2%) in this study, which is similar to the work of Chu and Dobratz19, who mainly described the large nasal tissue laxity of small cutaneous defects.
In the series of patients reported herein, our first option for the reconstruction of the nasal tip was bilobed flaps, followed by extended glabellar flaps. Guo et al.3 reported excellent results from bilobed flaps, with minimal distortion of this anatomic subunit. These flaps were also recommended by Steiger20, who showed excellent results from their use. The extended glabellar flap differs from the previous bilobed flaps, which lead to larger scars and a decreased distance between the eyebrows.
In the study by Collar et al.21, the bilobed flap was recommended for reconstruction of the nasal tip in lesions of up to 2 cm caused by cutaneous mass loss. The same authors suggested the use of paramedian frontal skin flaps for cancers affecting the nasal tip with an extension longer than 2 cm and no cartilage involvement. In this study, the bilobed flap was used to repair defects of up to 1.8 cm in the nasal tip. Satisfactory cosmetic and functional outcomes were obtained without postoperative complications. Paramedian frontal skin flaps were used to treat losses of larger mass, whereas frontal flaps were used to reconstruct losses affecting more than 1 aesthetic subunit and defects involving cartilage and/or mucosa. In this study, 10 of the 15 frontal flaps were applied to repair defects involving more than 1 aesthetic subunit, thus confirming their utility for the reconstruction of extensive and complex lesions. Repairing mass loss in addition to reconstructing the entire aesthetic subunit was a concept used to improve the aesthetic outcomes.
In conclusion, when mass losses affected the nasal roof, glabellar flaps were commonly used for the subsequent pronounced local skin sagging, as they provided excellent donor areas for these skin defects.
CONCLUSIONS
In this study, we described the various flaps used for the reconstruction of mass losses affecting different nasal subunits. The plastic surgeon should be aware of the different skin flaps described because the incidence of nasal skin cancers is continuously increasing. This study and other algorithms in the literature may help surgeons recommend appropriate treatment for nasal reconstruction without compromising the respiratory function and for providing satisfactory aesthetic results in the repair of each nasal subunit. Nasal contour and anatomy should always be considered when the reconstruction is planned and executed.
REFERENCES
1. Parrett BM, Pribaz JJ. An algorithm for treatment of nasal defects. Clin Plast Surg. 2009;36(3):407-20.
2. Yoon T, Benito-Ruiz J, García-Díez E, Serra-Renom JM. Our algorithm for nasal reconstruction. J Plast Reconstr Aesthet Surg. 2006;59(3):239-47.
3. Guo L, Pribaz JR, Pribaz JJ. Nasal reconstruction with local flaps: a simple algorithm for management of small defects. Plast Reconstr Surg. 2008;122(5):130e-9e.
4. Burget GC, Menick FJ. The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985;76(2):239-47.
5. Jacobs MA, Christenson LJ, Weaver AL, Appert DL, Phillips PK, Roenigk RK, et al. Clinical outcome of cutaneous flaps versus fullthickness skin grafts after Mohs surgery on the nose. Dermatol Surg. 2010;36(1):23-30.
6. Hollier HJ, Stucker FJ. Local flaps for nasal reconstruction. Facial Plast Surg. 1994;10(4):337-48.
7. Smeets NW, Kuijpers DI, Nelemans P, Ostertag JU, Verhaegh ME, Krekels GA, et al. Moh's micrographic surgery for treatment of basal cell carcinoma of the face: results of a retrospective study and review of the literature. Br J Dermatol. 2004;151(1):141-7.
8. Strom SS, Yamamura Y. Epidemiology of nonmelanoma skin cancer. Clin Plast Surg. 1997;24(4):627-36.
9. Kumar P, Orton CI, McWilliam LJ, Watson S. Incidence of incomplete excision in surgically treated basal cell carcinoma: a retrospective clinical audit. Br J Plast Surg. 2000;53(7):563-6.
10. Mureau MA, Moolenburgh SE, Levendag PC, Hofer SO. Aesthetic and functional outcome following nasal reconstruction. Plast Reconstr Surg. 2007;120(5):1217-27.
11. Telfer NR, Colver GB, Morton CA; British Association of Dermatologists. Guidelines for the management of basal cell carcinoma. Br J Dermatol. 2008;159(1):35-48.
12. Tan PY, Ek E, Su S, Giorlando F, Dieu T. Incomplete excision of squamous cell carcinoma of the skin: a prospective observational study. Plast Reconstr Surg. 2007;120(4):910-6.
13. Santos ABO, Loureiro V, Araújo Filho VJF, Ferraz AR. Estudo epidemiológico de 230 casos de carcinoma basocelular agressivos em cabeça e pescoço. Rev Bras Cir Cabeça Pescoço. 2007;36(4):230-3.
14. Griffiths RW. Audit of histologically incompletely excised basal cell carcinomas: recommendations for management by re-excision. Br J Plast Surg. 1999;52(1):24-8.
15. Petit JY, Avril MF, Margulis A, Chassagne D, Gerbaulet A, Duvillard P, et al. Evaluation of cosmetic results of a randomized trial comparing surgery and radiotherapy in the treatment of basal cell carcinoma of the face. Plast Reconstr Surg. 2000;105(7):2544-51.
16. Kimyai-Asadi A, Alam M, Goldberg LH, Peterson SR, Silapunt S, Jih MH. Efficacy of narrow-margin excision of well-demarcated primary facial basal cell carcinomas. J Am Acad Dermatol. 2005;53(3):464-8.
17. Uchinuma E, Matsui K, Shimakura Y, Murashita K, Shioya N. Evaluation of the median forehead flap and the nasolabial flap in nasal reconstruction. Aesthetic Plast Surg. 1997;21(2):86-9.
18. Woodard CR, Park SS. Reconstruction of nasal defects 1.5 cm or smaller. Arch Facial Plast Surg. 2011;13(2):97-102.
19. Chu MW, Dobratz EJ. Reconstruction of the dorsal and sidewall defects. Facial Plast Surg Clin North Am. 2011;19(1):13-24.
20. Steiger JD. Bilobed flaps in nasal reconstruction. Facial Plast Surg Clin North Am. 2011;19(1):107-11.
21. Collar RM, Ward PD, Baker SR. Reconstructive perspectives of cutaneous defects involving the nasal tip: a retrospective review. Arch Facial Plast Surg. 2011;13(2):91-6.
1. Aspiring member in training of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, resident physician at the Plastic Surgery Service of Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (São Lucas Hospital of the Pontifical Catholic University of Rio Grande do Sul) - HSL-PUCRS, Porto Alegre, RS, Brazil.
2. Associate member of SBCP, plastic surgeon at the Plastic Surgery Service of HSL-PUCRS, Porto Alegre, RS, Brazil.
3. Full member of SBCP, regent of the Plastic Surgery Service at HSL-PUCRS, Porto Alegre, RS, Brazil.
4. Full member of SBCP, preceptor of the Plastic Surgery Service at HSL-PUCRS, Porto Alegre, RS, Brazil.
Correspondence to:
Francisco Felipe Laitano
Rua Farnese, 199/501 - Bela Vista
Porto Alegre, RS, Brazil - CEP 90450-180
E-mail: fflpoa@hotmail.com
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 13, 2011
Article accepted: March 25, 2012
This study was performed at the Plastic Surgery Service of Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (São Lucas Hospital of the Pontifical Catholic University of Rio Grande do Sul), Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter