

Original Article - Year 2012 - Volume 27 -
Olecranon bone graft for nasal dorsal augmentation
Enxerto ósseo de olécrano para aumento do dorso nasal
ABSTRACT
BACKGROUND: Rhinoplasty surgery, performed for the treatment of "saddle-back" nose, has significantly improved in the last decades due to better management of grafts and implants. However, the choice of these materials is controversial and remains a subject of discussion. Scar contracture forces in nasal deformities prevent any type of reconstruction that is not rigid or semi-rigid. Therefore, the bone graft is an appropriate choice because it is stable, available, and reliable with regard to aesthetic outcomes. The olecranon bone graft is easily harvested and has a single cortical thickness, which is essential for resisting bone resorption and for providing long-lasting cosmetic results. The aim of this study is to discuss the advantages of the olecranon bone graft in rhinoplasty and to demonstrate our experience with this procedure.
METHODS: In this descriptive and retrospective study, we reviewed the medical records of patients who underwent olecranon bone grafting for nasal dorsal augmentation between January 2000 and January 2010 and were consequently followed-up for an equivalent period, at the Plastic Surgery Service of Hospital Daher Lago Sul (Daher Lago Sul Hospital, Brasília, DF, Brazil). Possible graft resorption was monitored by anthropometric measurements of the nose with photographic documentation and graft radiological control.
RESULTS: Satisfactory aesthetic results were achieved for the 9 patients who underwent surgery. According to the examinations performed to monitor possible graft resorption, projection loss or signs of bone resorption were not observed for up to 6 years after surgery.
CONCLUSIONS: The olecranon bone graft proved to be a suitable choice for primary or secondary rhinoplasty to treat "saddle-back" nose, with no long-term resorption or morbidity of the donor area observed up to this point. Moreover, the olecranon bone graft provides satisfactory, predictable, and long-lasting aesthetic results.
Keywords: Rhinoplasty. Nose/surgery. Bone transplantation. Transplantation, autologous.
RESUMO
INTRODUÇÃO: O planejamento cirúrgico nas rinoplastias para tratamento do "dorso em sela" apresentou grande avanço nas últimas décadas, em decorrência do melhor manejo de enxertos e implantes. Porém, a escolha desses materiais é tema de controvérsia e debates. As forças da cicatriz no nariz com deformidades tendem a subjugar qualquer tipo de reconstrução que não seja rígida ou semirrígida. Assim, o enxerto ósseo é uma boa opção, pois é estável, apresentando boa disponibilidade e confiabilidade nos resultados estéticos. O enxerto ósseo de olécrano é de fácil coleta, tem uma única espessura do córtex, característica importante para resistir à reabsorção, além de proporcionar resultado estético estável. Este trabalho tem como objetivo discutir as vantagens da utilização do enxerto ósseo de olécrano em rinoplastias e demonstrar a experiência com esse tipo de procedimento.
MÉTODO: Estudo descritivo e retrospectivo, sendo realizada revisão dos prontuários de pacientes submetidos a enxerto ósseo de olécrano para aumento de dorso nasal, no período de janeiro de 2000 a janeiro de 2010, com acompanhamento por igual período, no Serviço de Cirurgia Plástica do Hospital Daher Lago Sul (Brasília, DF, Brasil). O controle de possível reabsorção do enxerto foi realizado com medidas antropométricas do nariz em documentação fotográfica, além de controle radiológico do enxerto.
RESULTADOS: Foram operados 9 pacientes, sendo obtidos bons resultados estéticos. Em nenhum dos métodos para controle de possível reabsorção do enxerto ficou evidenciada alguma perda de projeção ou sinais de reabsorção óssea no acompanhamento com até 6 anos de pós-operatório.
CONCLUSÕES: O enxerto de olécrano demonstrou ser uma boa opção para rinoplastias primárias ou secundárias, no tratamento do "dorso em sela", não tendo sido demonstrada reabsorção a longo prazo ou morbidade da área doadora, com bons resultados estéticos, previsíveis e duradouros.
Palavras-chave: Rinoplastia. Nariz/cirurgia. Transplante ósseo. Transplante autólogo.
Rhinoplasty surgery, performed for the treatment of "saddle-back" nose and for aesthetic or reconstructive purposes, has significantly improved during the last few decades because of the better management of grafts and implants. However, the choice of these materials remains controversial and is a subject of discussion. Currently, several grafts and implants have been described for this procedure and these are classified according to their origin: autologous, homologous, or synthetic1,2.
Autografts include cartilage, bone, fascia, and dermis from the same individual, whereas homografts are derived from tissue donated by individuals of the same species. Homografts include irradiated cartilage and acellular dermis, which are not used in our daily practice. Synthetic implants are alloplastic products (biocompatible polymers), of which silicone is commonly used in Asia for nasal augmentation3. Autologous grafts have higher biocompatibility and a lower risk of infection and extrusion when compared to homograft or alloplastic implants. However, it should be noted that several issues are associated with these grafts including morbidity of the donor area, graft availability, and the possibility of graft resorption.
In major nasal deformities or secondary rhinoplasty, the forces of scar contractures prevent any type of reconstruction that is not rigid or semi-rigid. The reconstruction strategy should aim to confer nasal tip and dorsum stability until the contraction diminishes. Therefore, the bone graft is a suitable choice because it is stable, available, and reliably produces satisfactory aesthetic results1,3-10.
The aim of this study is to discuss the benefits of the olecranon bone graft in rhinoplasty and to demonstrate our experience with this procedure.
METHOD
In this descriptive and retrospective study, we reviewed the medical records of patients who underwent olecranon bone graft for nasal dorsal augmentation between January 2000 and January 2010 and were consequently followed-up for an equivalent period.
The indications for bone graft in dorsal nasal augmentation include "saddle-back" nose, inflammatory conditions, burn sequelae, tumor resection, Binder's syndrome, primary aesthetic rhinoplasty in afro-descendants, and secondary rhinoplasty in patients with excessive surgical removal of osteocartilaginous structures1-12.
Surgical Procedure for Graft Removal
The non-dominant forearm was chosen for removal of the olecranon bone graft. The proximal third of the posterior face was infiltrated followed by a longitudinal incision and dissection of the planes. The cortex of the olecranon was measured according to the nasal defect for repair and the graft was removed with a bone saw or a simple chisel (Figure 1).
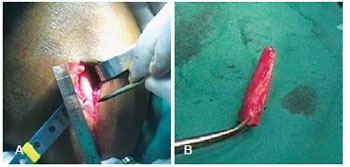
Figure 1 - In A, donor area in the forearm. In B, bone graft.
Upon removal, the olecranon was placed in a container with saline solution and the donor area was covered with bone wax. Synthesis was carried out by planes, with absorbable sutures and of skin with 4.0 nylon intradermal threads. Finally, the limb was covered with a crepe bandage. A tourniquet was not necessary. The graft was transferred into the recipient area with external anchoring with micropore tape for 21 days; rigid fixation was not used.
Possible graft resorption was monitored by anthropometric measurements of the nose with photographic documentation and graft radiological control. Frontal, oblique, lateral, and nasal base photographs were taken 3, 6, 12, and 24 months after surgery and the images were compared. The height of the nasal tip and dorsum and the length of the dorsum were measured. Graft radiographs were obtained postoperatively at 6, 12, and 24 months and the height of the nasal dorsum, graft length, and possible signs of bone resorption were assessed.
RESULTS
The olecranon bone graft was used in 9 rhinoplasties: 6 were performed for aesthetic purposes in afro-descendants and 3 were performed for "saddle-back" nose reconstruction. All 5 surgeries performed in women were for aesthetic purposes (Figure 2), whereas 4 of the surgeries performed in men, one of them was for aesthetic purposes (Figure 3), and the other 3 were performed for nasal reconstruction (Figure 4). The age of the patients at the time of the surgery varied from 21 to 43 years, with an average age of 27 years.

Figure 2 - In A and C, rhinoplasty preoperative aspect: frontal and left profile, respectively. In B and D, rhinoplasty postoperative aspect after micropore tape removal: frontal and left profile, respectively
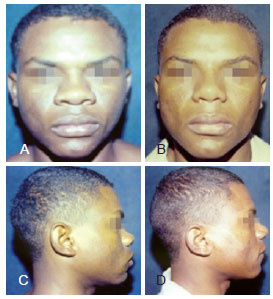
Figure 3 - In A and C, rhinoplasty preoperative aspect: frontal and right profile, respectively. In B and D, postoperative aspect 4 years after rhinoplasty: frontal and right profile, respectively.
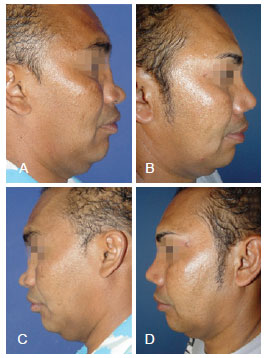
Figure 4 - In A and C, rhinoplasty preoperative aspect: right and left profile, respectively. In B and D, postoperative aspect 2 years after rhinoplasty: right and left profile, respectively.
Open rhinoplasty was performed in 8 patients and the closed rhinoplasty procedure was used in 1 patient, the first of our series. The postoperative follow-up varied between 12 months and 6 years, with an average of 24 months.
According to the exams performed to monitor possible graft resorption (Figure 5), projection loss or signs of bone resorption did not occur up to 6 years after surgery. Secondary rhinoplasties were not necessary in this series of patients. Graft displacement or hypertrophic scars/synechiae did not occur and respiratory complaints were not reported.
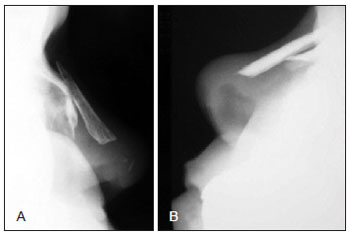
Figure 5 - In A and B, radiological controls 2 years after surgery; no signs of graft resorption were observed.
All patients reported temporary paresthesia in the forearm scar (donor area), with a complete recovery within 1 year. None of the patients presented with a hypertrophic scar or keloids in that region (Figure 6). All patients reported mild pain in the area where the bone graft was removed, with complete recovery after 2 months. No cases of persistent pain or sequelae in the donor forearm were observed.

Figure 6 - Aesthetic and barely perceptible scar in the donor area.
DISCUSSION
In a literature review, Foda13 reported that irregularities in the nasal dorsum and "saddle-back" nose represent 54% and 44%, respectively, of all complaints leading to secondary rhinoplasty. In these cases, septal cartilage is usually considered the best material for nasal deformity repair because it is easy to harvest and has properties that are similar to the original cartilaginous framework of the nose. Moreover, it confers adequate structural support1. However, the limitation of this choice is the amount of mass that potentially must be removed. Consequently, the second option for the surgeon is the auricular cartilage because it is proven to be flexible and resistant. In addition, a variety of different forms can be harvested and rendered available. Auricular cartilage is the first choice for the reconstruction of the external nasal valve because low donor site morbidity has been observed so far. Although the modeling of this graft is an advantage, it can be deformed easily as it is more fragile, less rigid, and less able to confer support than septal cartilage when it is damaged.
On the other hand, costal cartilage is an abundant source of material that provides proper resistance and support and demonstrates efficient long-term viability and minimal reabsorption. Possible disadvantages include morbidity in the donor area (pneumothorax, scar-induced chest wall deformities, persistent pain, paresthesia, infection, and dehiscence) and unpredictable shape maintenance1.
A common complication associated with cartilage grafts is inadequate placement. Other complications include bone resorption, extrusion, and deformity1,4,11,13.
Another alternative for nasal reconstruction is the acellular dermis. However, this alternative is not permitted by the National Agency of Health Surveillance. Furthermore, this material should not be used as a supporting graft when a deformity larger than 3 mm is observed in the dorsal profile of the nose2.
The main complications observed in synthetic implants are extrusion and infection, which lead to unacceptable scars and are difficult to repair with minor surgery, particularly when the extrusion is through the skin of the nasal tip2,3. Severe nose shortening may also occur due to recurrent infections and nasal capsular contractures around the silicone prosthesis.
Synthetic materials such as high-density porous polyethylene (Medpor®, Porex®), which were developed in the 1970s, are also important. Although these materials are expensive, their micropores facilitate better insertion of the implant and decrease the rates of extrusion and infection compared to other synthetic materials1.
Different bone graft donor areas such as the iliac crest, skullcap, mastoid, ribs, and olecranon have been used for nasal reconstruction and dorsal augmentation. These grafts confer excellent structural support, are abundantly available, and provide reliable aesthetic results. Regardless of the source of the bone graft, the following concepts should be taken into consideration for better implantation of these grafts: the concept of graft augmentation, preparation of the nasal dorsum for insertion of the bone graft into the recipient area, and immobilization1,3-10. In this study, immobilization was performed only with external micropore tape in order to avoid complications due to fixing screws. Gurley et al.14 reported that almost two-thirds of the fixing screws were removed in patients who underwent nasal dorsal augmentation with the iliac bone graft because of skin erosion, palpability, or easy visibility.
Bone graft removal from the skullcap is well tolerated, with minimal or no postoperative discomfort compared to the significant morbidity that is commonly associated with iliac crest resections and usually lasts 2 or 3 weeks. However, injuries to the central nervous system and hematoma formation might occur, although these appear to be rare1.
The olecranon bone graft is our first choice because it is easy to harvest and leads to minimal morbidity of the donor area. The insertion of the olecranon bone graft in the donor area is performed with the spongy part adhered to the nasal bone, thus allowing graft fixation. This procedure ensures long-lasting results without long-term resorptions. Moreover, the use of the olecranon bone graft is not associated with disadvantages commonly associated with other grafts such as neurological injuries or walking-induced pain. The olecranon bone graft presents a single cortex thickness (2 mm to 5 mm), which is essential for avoiding resorption and providing long-lasting esthetic results1,3,12.
In this study, possible graft resorption was monitored by anthropometric measurements and radiological control according to studies in the literature describing cephalometry on iliac bone grafts. The distance between the following 3 points was analyzed for each image: the height of the tip and the lengths of the upper and lower grafts14,15.
Open rhinoplasty, which was used in most of the cases described herein, is becoming the preferred method because it provides better structural handling of the nose than closed rhinoplasty.
CONCLUSIONS
The olecranon bone graft proved to be a good option for primary or secondary rhinoplasty for the treatment of "saddle-back" nose. Long-term resorption or morbidity of the donor area has not been observed so far. This procedure ensures satisfactory, predictable, and long-lasting aesthetic results.
REFERENCES
1. Sajjadian A, Rubinstein R, Naghshineh N. Current status of grafts and implants in rhinoplasty: part I. Autologous grafts. Plast Reconstr Surg. 2010;125(2):40e-9e.
2. Sajjadian A, Rubinstein R, Naghshineh N. Current status of grafts and implants in rhinoplasty: part II. Homologous grafts and allogenic implants. Plast Reconstr Surg. 2010;125(3):99e-109e.
3. Hodgkinson DJ. The Eurasian nose: aesthetic principles and techniques for augmentation of Asian nose with autogenous grafting. Aesthetic Plast Surg. 2007;31(1):2831.
4. Baek RM, Eun SC, Heo CY, Min KH. Rhinoplasty using rib chondroosseous graft in Asian patients. J Craniofac Surg. 2010;21(4):1122-5.
5. Sadooghi M, Kouhi A. Mastoid bone as a new graft material in rhinoplasty. Am J Rhinol Allergy. 2009;23(6):e42-6.
6. Shipchandler TZ, Chung BJ, Alam DS. Saddle nose deformity reconstruction with a split calvarial bone L-shaped strut. Arch Facial Plast Surg. 2008;10(5):305-11.
7. Chou TD, Lee WT, Chen SL, Lee CH, Chen SG, Chen TM, et al. Split calvarial bone graft for chemical burn-associated nasal augmentation. Burns. 2004;30(4):380-5.
8. Neu BR. Segmental bone and cartilage reconstruction of major nasal dorsal defects. Plast Reconstr Surg. 2000;106(1):160-70.
9. Posnick JC, Seagle MB, Armstrong D. Nasal reconstruction with full-thickness cranial bone grafts and rigid internal skeleton fixation through a coronal incision. Plast Reconstr Surg. 1990;86(5):894-904.
10. Goh RC, Chen YR. Surgical management of Binders syndrome: lessons learned. Aesthetic Plast Surg. 2010;34(6):722-30.
11. Bottini DJ, Gentile P, Donfrancesco A, Fiumara L, Cervelli V. Augmentation rhinoplasty with autologous grafts. Aesthetic Plast Surg. 2008;32(1):136-42.
12. Hodgkinson DJ. The olecranon bone graft for nasal augmentation. Aesthetic Plast Surg. 1992;16(2):129-32.
13. Foda HM. Rhinoplasty for the multiply revised nose. Am J Otolaryngol. 2005;26(1):28-34.
14. Gurley JM, Pilgram T, Perlyn CA, Marsh JL. Long-term outcome of autogenous rib graft nasal reconstruction. Plast Reconstr Surg. 2001;108(7):1895-907.
15. Sarukawa S, Sugawara Y, Harii K. Cephalometric long-term follow-up of nasal augmentation using iliac bone graft. J Craniomaxillofac Surg. 2004;32(4):233-5.
1. Plastic surgeon, full member of Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, regent of the Plastic Surgery Service of the Hospital das Forças Armadas (Armed Forces Hospital), Brasília, DF, Brazil.
2. Resident physician at the Plastic Surgery Service of Hospital Daher Lago Sul (Daher Lago Sul Hospital), aspiring member in training of the SBCP, Brasília, DF, Brazil.
3. Plastic surgeon, full member of SBCP, preceptor of the Plastic Surgery Service of the Hospital das Forças Armadas (Armed Forces Hospital), Brasília, DF, Brazil.
4. Plastic surgeon at the Hospital Regional da Ceilândia (Ceilândia Regional Hospital), full member of SBCP, Brasília, DF, Brazil.
5. Surgeon at the Hospital Regional do Gama (Gama Regional Hospital), specialist member of SBCP, Brasília, DF, Brazil.
Correspondence to:
Ognev Meireles Cosac
Condomínio Villages Alvorada cj. 17 casa 10 - Lago Sul
Brasília, DF, Brazil - CEP 71680-351
E-mail: ognev@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 23, 2011
Article accepted: February 6, 2012
This study was performed at the Plastic Surgery Service of Hospital Daher Lago Sul (Daher Lago Sul Hospital), Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter