

Original Article - Year 2012 - Volume 27 -
Profession-related postural changes in surgeons
Alterações posturais em cirurgiões provocadas pela atividade profissional
ABSTRACT
BACKGROUND: Any deviation from the standard posture is considered a postural alteration; although this is not necessarily considered a disease, it may substantially affect the quality of life of surgeons. The aim of this study was to evaluate backbone alignment and posture in surgeons and physicians in order to identify and quantify the positioning of body segments and investigate possible postural alterations.
METHODS: Thirty subjects participated in the study group (CI) and corresponded to the following inclusion criteria: physician, aged 30-60 years, with at least 2 years of surgical practice and performing 4 weekly surgeries lasting 2 h each. The comparative group (CL) included 32 clinical physicians, in the same age range as the CI group. The control group (CO) included 33 non-physicians in the same age range as the CL and CI groups, who satisfied the following exclusion criteria: chronic muscle-skeletal pain or acute intense pain, diagnosis of or sequelae from orthopedic, rheumatologic, or respiratory disease, or prosthetic use.
RESULTS: We observed a high incidence of postural changes in the CI group, including varus thrust, hyperextension, lumbar hyperlordosis, and more foot support in the heel, and other misalignments. The results indicate that the activities of surgeons may be considered as a risk for the musculoskeletal system. Because the specialty of plastic surgery is particularly surgical, the risk is even higher in these surgeons.
CONCLUSIONS: Surgical activity provokes progressive postural changes in surgeons and may reduce useful time in the profession and hinder the quality of life.
Keywords: Posture. Physicians. Workload.
RESUMO
INTRODUÇÃO: Qualquer desvio da postura padrão é considerado alteração postural, o que não é necessariamente classificado como doença, embora afete consideravelmente a qualidade de vida dos profissionais cirurgiões. O objetivo deste estudo foi avaliar o alinhamento e o controle posturais de médicos cirurgiões e não-cirurgiões, a fim de identificar e quantificar o posicionamento dos segmentos corporais e averiguar comparativamente possíveis alterações posturais.
MÉTODO: Participaram do estudo 30 sujeitos no grupo teste (CI), que atenderam aos seguintes critérios de inclusão: ser médico, idade entre 30 anos e 60 anos, com, no mínimo, 2 anos de prática cirúrgica e 4 cirurgias semanais com duração de 2 horas cada uma. O grupo comparativo (CL) constituiu-se de 32 sujeitos, médicos clínicos, com idade similar ao do grupo CI. O grupo controle (CO) constituiu-se de 33 sujeitos não-médicos, com a mesma faixa etária dos grupos CL e CI, que atendiam aos seguintes critérios de exclusão: presença de dor musculoesquelética crônica ou dor aguda intensa; diagnóstico ou sequela de doença ortopédica, reumatológica ou respiratória; ou utilização de prótese.
RESULTADOS: Observou-se alta incidência de alterações posturais no grupo CI, como joelho varo, hiperextensão, hiperlordose lombar e pé com maior apoio em calcâneo, além de outros desalinhamentos. Os resultados indicam que as atividades dos cirurgiões podem ser consideradas de risco para o sistema musculoesquelético. Por ser eminentemente cirúrgica, a especialidade de cirurgia plástica é de risco ainda maior.
CONCLUSÕES: A atividade cirúrgica provoca alterações posturais progressivas nos cirurgiões, podendo reduzir a vida útil na profissão e prejudicar a qualidade de vida.
Palavras-chave: Postura. Médicos. Carga de trabalho.
Postural alignment is a standard reference used internationally for normal posture and any asymmetry between the body segments is considered a postural alteration1,2. Man has always attempted to make the objects in his environment more suitable to his needs by minimizing the effort required to use them3. It was in this context that ergonomics originated; ergonomics studies the interaction between humans and their work environment, aiming at achieving safety, efficiency, and better quality of life4.
With physical and postural focus, Kendall et al.5 proposed the model of perfectly aligned posture. In the side view, this refers to the alignment of body segments of the anterior and posterior sides, divided by the frontal plane. In the anterior and posterior views, segment alignment is established by right and left symmetry divided by a sagittal plane (Figure 1).

Figure 1 - Postural analysis of the control group (CO), in posterior (A), anterior (B) and right lateral (C) views.
The study of postural alignment is justified by the fact that mechanical stress has clinical consequences and affects connective tissue in muscles and joints. Bad body alignment during surgical procedures may alter the distribution of load and pressure in the joints, thereby contributing to joint degeneration and inappropriate muscle tension6,7.
Many variables are involved in postural evaluation and qualitative analysis, mostly performed by observation, has not been very reproducible, making it necessary to quantify these variables8. Some studies have shown that ergonomics may contribute significantly to the analysis of important work situations in hospitals and may help surgeons better execute activities considered to involve extreme responsibility, including tasks and skills that are exhausting for osteo-muscular, physiological, and psychological functions, because of the long time periods spent practicing this activity9. While performing surgery, it is difficult for surgeons to maintain an erect posture because it involves the alignment of and control over several body segments6,9. Remaining upright while standing demands swings and body movements for the maintenance of balance, with stimuli coming from the vestibular, somatosensorial, and visual systems, which requires complex interaction between the neural and musculoskeletal systems, including biomechanical relationships between body segments9. Added to this is the psychological stress of the surgeon during long surgeries, hypercontracting specific muscle chains, and the need to bend forward to effectuate the surgery. Rotating right or left (for right-or left-handed surgeons) to place the arms and hands in a better position also occurs in an effort to improve technical ability. Danis et al.10 have shown a strong correlation between people with alterations in stability and postural deviations.
Few studies have performed quantitative evaluation of postural alignment with attention to body segments during all visits. Therefore, we aimed at observing and evaluating alignment and postural control in physicians and surgeons in order to identify and quantify the positioning of the body segments and comparatively investigate possible posture alterations.
METHOD
This is a descriptive, explorative, and cross-sectional study, in which 30 subjects participated in the test group (CI), corresponding to the following inclusion criteria: a physician, aged 30-60 years, with at least 2 years of surgical practice and 4 weekly surgeries lasting 2 h each, who signed the informed consent form. The comparative group (CL) included 32 clinical physicians, in the same age range as the CI group. The control group (CO) included 33 non-physicians in the same age range as the CL and CI groups, who satisfied the following exclusion criteria: chronic muscleskeletal pain or acute intense pain, diagnosis of or sequelae from orthopedic, rheumatologic, or respiratory disease, or prosthetic use.
The data was collected in a surgical center and in the Hospital de Base (São José do Rio Preto, SP, Brazil). A digital camera (Sony Cyber-shot, 7.2 mega pixels) was used for taking the pictures, and an anamnesis protocol was designed for this study, including questions for subject identification, sample characterization, and presence or absence of pain. Data collection was carried out individually in a single previously appointed session. Initially, every subject was informed of the aims of the study, was asked to complete the anamnesis questionnaire, and measurements of height and weight as well as were photos taken, with the subject wearing a swimsuit. The subjects were photographed from anterior, posterior, left side, and right side views, and then localization and demarcation of anatomical points were performed. Systematic observation11 was performed, not involving the establishment of previous criteria to guide the registration of the phenomenon to be observed for postural analysis of the subjects. To standardize data collection, a protocol was assembled to register and analyze postures and kinetic description. Anatomical points were demarcated in the regions of the head, trunk, upper limbs, and lower limbs.
In the anterior view, in standard posture, the criteria were as follows:
hallux aligned with the first metatarsus; hind foot aligned with the center of the foot; preserved foot arches; straight ankles at the same distance as the medial side of the knees; straight tibias, no arches; knees not touching each other and the distance between them should be the same distance as that between the medial malleoli of the tibias; patellae (rotulas) at the same height and pointing forward; pelvis at the same height at both sides, measured by the height of the anterior superior iliac spine; straight trunk, with no rotations or bends; shoulders at same height as the clavicles; symmetrical clavicular creases; straight head and neck, no rotations or bends.
In the posterior view, the evaluation was based on an imaginary line starting at a mid-point between the heels, extending upwards between the lower limbs and passing through the medial line of the pelvis, backbone, and head and using the following criteria:
symmetrical right and left halves, both in skeletal and muscular structure; back of the foot with symmetrical support, not too supported medially or laterally; heel vertically aligned with Achilles tendon; medial malleoli equal in height; popliteal creases and gluteal creases of equal height; pelvis of equal height on both sides, with posterior superior iliac spines leveled horizontally; straight backbone, no lateral deviations; symmetrical Thales triangles, on both sides; scapulas at the same distance from the backbone, flattened against the thorax; inferior angle of the scapulas leveled horizontally; shoulders at same height; straight head and neck, without lateral rotations or bends.
In the lateral view, alignment was based on a reference line that, in ideal posture, passed slightly anterior to the lateral malleolus of the fibula, slightly anterior to the center of the knee joint, slightly posterior to the hip joint, roughly through the middle of the trunk, through the shoulder joint (as long as the arms hung normally aligned with the thorax), through the cervical vertebrae, and through the earlobe12.
The variables were summarized in simple and relative (percentage) frequencies.
RESULTS
In all of the 3 groups, we observed a predominance of the male gender (100%), dominant right-handedness (95.5%), and a mean body mass index (BMI) of 24.3 ± 4.3, with 65% of the subjects having normal weight. The average age in the groups was 38.7 ± 8.4 years, mean height was 1.72 m, and mean weight was 76.53 kg.
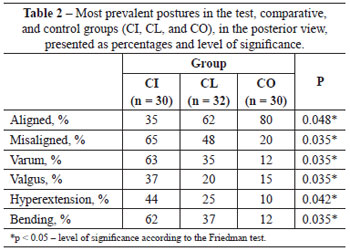
In the anterior view (Figure 2A), individuals of the CI group showed: significantly more misalignment of the feet with abducted hind foot (left and right); high medial longitudinal arch (left and right); left genu varum and right genu valgum; misaligned anterior superior iliac spines (the right spine being higher); asymmetric thorax; shoulder joint with left medial rotation and right lateral rotation; elbows with increased right bending; and head hanging laterally to the left (Table 1).
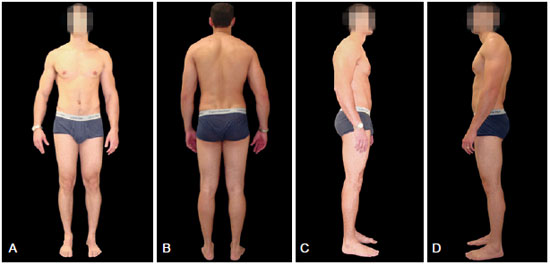
Figure 2 - Postural analysis of the study group (CI), in posterior (A), anterior (B), right lateral (C) and left lateral (D) views.
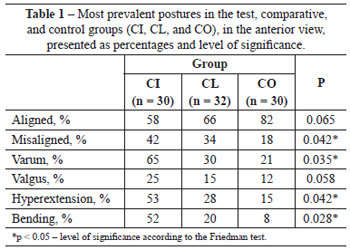
In the posterior view (Figure 2B), individuals from the CI group showed significantly more alterations, including: misaligned heels; left varum and right valgum; misaligned back of the feet; left and right genu valgum; misaligned posterior superior iliac spines, with the right spine being higher; backbone of the thorax convex to the left; cervical backbone convex to the left; shoulders higher on the left; and head hanging laterally to the right (Table 2).
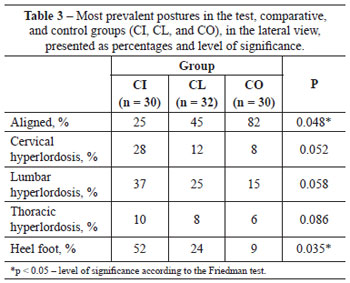
In the lateral view (Figures 2C and 2D), individuals of the CI group showed significantly more postural alterations than the other groups, including: feet with heel support; left hyperextension of the knee; flexed right; pelvis with anteversion of the iliac crest; trunk with rotated scapula and right and left pelvis; lumbar backbone with increased lordosis; thoracic backbone with increase in kyphosis and winged scapula on the left; cervical backbone with increased lordosis; shoulders with right medial rotation; protruding head (Table 3).
Asymmetry in the shoulders and abnormal alignment of the scapulas, as a result of lateral bending, were prevalent in the CI group.
Postural changes grouped by misalignments were more prevalent in the CI group. Lumbar hyperlordosis and genu varum were also prevalent in this group.
DISCUSSION
The results of the current study concerning postural aspects indicate that surgeons are at risk of damage to the musculoskeletal system. These data corroborate previous studies in other professionals12-14, indicating that physical load upon surgeons during elective procedures, depending on the length of the surgery, causes deformities in the course of time.
Generally, surgeons do not realize the position they adopt during their activity and feel tired, but few present with complaints related to posture; this finding contradicts that in some studies15,16.
The analysis of the results of the present study shows that the postures adopted by surgeons during the course of surgery force the surgeon to place their body weight on 1 leg, overloading one-half of the body and causing joint alterations in the thigh and femur in the long run, which corroborates other studies17,18.
The specialty of plastic surgery is eminently surgical and the surgeon sometimes spends more than 4 h daily in surgery, thereby increasing the possibility of acquiring serious postural defects, with consequences for physical health and professional longevity.
The small sample in the current study limited the understanding of some relationships that could possibly elucidate the postural changes and musculoskeletal lesions related to work in surgeons. It is important to highlight that several ergonomic improvements could avoid such alterations. Among the proposed methods, one with proven efficacy is Global Postural Reeducation (GPR), which considers the muscular and skeletal systems as a whole and treats individuals with static body work (isometric contraction) and dynamic body work (isotonic contraction). The aim of this treatment is to improve tone, function and muscle strength, proprioception and perception, joint alignments, coordination, balance, and walking.
The results of the current study serve as a precaution for surgeons and suggest the need for prevention of the described alterations, which may compromise quality of life and useful time in the profession.
CONCLUSIONS
Surgical activity causes progressive postural changes in surgeons, and may reduce useful time in the profession and damage quality of life.
REFERENCES
1. Gil Coury HJC, Porcatti IA, Alem MER, Oishi J. Influence of gender on work-related musculoskeletal disorders in repetitive tasks. Int J Ind Ergon. 2002;29(1):33-9.
2. Junqueira L. Anatomia palpatória: tronco, pescoço, ombro e membros superiores. Rio de Janeiro: Guanabara Koogan; 2004.
3. Santos A. Diagnóstico clínico postural: um guia prático. São Paulo: Summus; 2001.
4. Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2005;30(19):2153-63.
5. Kendall FP, McCreary EK, Provance PG. Postura: alinhamento e equilíbrio muscular. In: Kendall FP, McCreary EK, Provance PG, eds. Músculos: provas e funções. 4ª ed. São Paulo: Manole; 1995. p. 69-118.
6. Campos F, Silva A, Anhesim GA. Alterações posturais e abordagem fisioterapêutica em crianças e adolescentes obesos. In: Fisberg M, ed. Atualização em obesidade na infância e adolescência. São Paulo: Atheneu; 2004. p. 131-41.
7. Medina-Rodríguez F, Andrade-Padilla MA, Rivera-Ibarra DB, Gaña-Eretza B. Educative posture estimation of the doctors with and without educational formation. Rev Med Inst Mex Seguro Soc. 2009;47(6):677-82.
8. Castien RF, van der Windt DA, Dekker J, Mutsaers B, Grooten A. Effectiveness of manual therapy compared to usual care by the general practitioner for chronic tension-type headache: design of a randomised clinical trial. BMC Musculoskelet Disord. 2009;10:21.
9. Szeto GP, Ho P, Ting AC, Poon JT, Tsang RC, Cheng SW. A study of surgeons' postural muscle activity during open, laparoscopic, and endovascular surgery. Surg Endosc. 2010;24(7):1712-21.
10. Danis CG, Krebs DE, Gill-Body KM, Sahrmann S. Relationship between standing posture and stability. Phys Ther. 1998;78(5):502-17.
11. Szeto GP, Ho P, Ting AC, Poon JT, Cheng SW, Tsang RC. Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil. 2009;19(2):175-84.
12. Ribeiro CZP, Akashi PMH, Sacco ICN, Pedrinelli A. Relação entre alterações posturais e lesões do aparelho locomotor em atletas de futebol de salão. Rev Bras Med Esporte. 2003;9(2):91-7.
13. Gentzler M, Stader S. Posture stress on firefighters and emergency medical technicians (EMTs) associated with repetitive reaching, bending, lifting, and pulling tasks. Work. 2010;37(3):227-39.
14. Ngan K, Drebit S, Siow S, Yu S, Keen D, Alamgir H. Risks and causes of musculoskeletal injuries among health care workers. Occup Med.2010;60(5):389-94.
15. Takala EP, Pehkonen I, Forsman M, Hansson GA, Mathiassen SE, Neumann WP, et al. Systematic evaluation of observational methods assessing biomechanical exposures at work. Scand J Work Environ Health. 2010;36(1):3-24.
16. Rempel D, Star D, Barr A, Blanco MM, Janowitz I. Field evaluation of a modified intervention for overhead drilling. J Occup Environ Hyg. 2010;7(4):194-202.
17. Stock SR, Fernandes R, Delisle A, Vézina N. Reproducibility and validity of workers' self-reports of physical work demands. Scand J Work Environ Health. 2005;31(6):409-37.
18. Gori L, Firenzuoli F. Posturology. Methodological problems and scientific evidence. Recenti Prog Med. 2005;96(2):89-91.
1. Physiotherapist in the department of Neurological Sciences of the Faculdade de Medicina de São José do Rio Preto (Faculty of Medicine of São José do Rio Preto) - FAMERP, São José do Rio Preto, SP, Brazil.
2. Professor Doctor in the department of Neurological Sciences of the FAMERP, São José do Rio Preto, SP, Brazil.
3. Professor Doctor in Plastic Surgery, head of the Plastic Surgery Unit of the Hospital de Base (Base Hospital), São José do Rio Preto, SP, Brazil.
Correspondence to:
Antonio Roberto Bozola
Av. Brigadeiro Faria Lima, 5416 - São Pedro
São José do Rio Preto, SP, Brazil - CEP 15090-000
E-mail: ceplastica@hotmail.com
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 30, 2012
Article accepted: March 11, 2012
Study carried out at the Faculdade de Medicina de São José do Rio Preto (Faculty of Medicine of São José do Rio Preto) - FAMERP, São José do Rio Preto, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter