

Original Article - Year 2012 - Volume 27 -
Mastopexy associated with submuscular or subglandular silicone implants: indications and complications
Mastopexia associada a implante de silicone submuscular ou subglandular: sistematização das escolhas e dificuldades
ABSTRACT
BACKGROUND: Throughout history, the breasts are considered important to the femininity and self-esteem of women. In augmentation mammoplasty, organ function must be preserved. Indications for the best tissue plane for coverage of silicone implants and association with mastopexy can be challenging. The aim of this study was to evaluate a series of cases of mastopexy associated with silicone implants.
METHODS: A retrospective descriptive study was performed in patients who underwent mastopexy at the Plastic Surgery Unit of the Hospital Daher Lago Sul (Brasília, DF, Brazil). From July 2008 to July 2011, 243 patients with a mean age of 31.4 years underwent surgery. In 149 patients, the subglandular technique was used and in 94 patients, the submuscular technique was used. Implant volume ranged from 150 mL to 400 mL. RESULTS: There were 174 cases of combined procedures. Four patients who underwent surgery using the subglandular technique developed capsular contracture (grade II). We followed up 7 cases of pseudoptosis with the submuscular technique and 14 cases of mammary ptosis with the subglandular technique. Eight patients experienced a mobile implant resulting from muscle activity. The reoperation rate was 6.58%.
CONCLUSIONS: Treatment of mammary ptosis associated with augmentation mammoplasty demands a complex combination of techniques and careful preoperative analysis in order to define the best techniques to be used; this procedure lowers the need for surgical revisions and allows harmonious, stable, and long-lasting results.
Keywords: Mammaplasty. Breast/surgery. Breast implantation.
RESUMO
INTRODUÇÃO: Ao longo dos tempos tem sido reportado o papel fundamental das mamas na feminilidade. Na mamoplastia de aumento deve-se buscar preservar a funcionalidade do órgão.As indicações do melhor plano tecidual de cobertura e a associação com a mastopexia podem tornar-se um grande desafio. O objetivo deste trabalho é avaliar uma série de casos de mastopexia associada a implantes.
MÉTODO: Estudo descritivo retrospectivo de pacientes submetidas a mamoplastia de aumento e mastopexia no Serviço de Cirurgia Plástica do Hospital Daher Lago Sul (Brasília, DF, Brasil). No período de julho de 2008 a julho de 2011, 243 pacientes foram operadas, com média de idade de 31,4 anos, sendo 149 operadas pela técnica subglandular e 94, pela submuscular. Os volumes dos implantes variaram de 150 ml a 400 ml.
RESULTADOS: Houve 174 casos de procedimentos combinados. Quatro pacientes submetidas à técnica subglandular desenvolveram contratura capsular (grau II). Foram observados 7 casos de pseudoptose pela técnica submuscular e 14 de ptose mamária pela técnica subglandular. Oito pacientes apresentaram mobilidade do implante pela ação do músculo. A taxa de reoperação total foi de 6,58%.
CONCLUSÕES: O tratamento da ptose mamária associado a mamoplastia de aumento exige combinações técnicas complexas e cuidadosa análise pré-operatória, para definição das melhores técnicas a serem utilizadas, diminuindo a necessidade de revisões cirúrgicas e permitindo a obtenção de resultados harmônicos, duradouros e estáveis.
Palavras-chave: Mamoplastia. Mama/cirurgia. Implante mamário.
Throughout history, breasts are considered fundamentally important for femininity and the self-esteem of women. This important role is reinforced by images exploring the theme of femininity, for example, in works by artists such as Frida Kahlo (Figure 1)1-15.
Figure 1 - My nurse and I (1937), by Frida Kahlo. Oil on canvas. Collection Foundation Dolores Olmedo (Mexico).
Where aesthetic surgery of the breast is concerned, augmentation mammoplasty is the most commonly performed procedure in Brazil, according to data from the DataFolha and the Brazilian Society of Plastic Surgery2. This surgi cal procedure aims to give the breasts a better shape, but it must also preserve the function of these organs, due to their importance in breastfeeding. Factors such as chronic pain, capsular contracture, and excessive pressure of the implant over the parenchyma can cause problems with breastfeeding3.
In daily surgical practice, inserting a silicone implant, particularly in the subglandular plane, appears to be a simple procedure, even for surgeons in training. However, the indications for the best tissue plane to use for coverage of the implant and for association with mastopexy can easily become challenging, eventually requiring secondary procedures4,5. When choosing the best surgical technique, the surgeon must aim to achieve the most natural and long-lasting results. The technique of mammary augmentation with subpectoral implants, associated with mastopexy or not, is one of the options available to the surgeon.
The submuscular implant may be placed in 3 different planes: completely submuscular, including the large pectoral muscle, external obliques, anterior serratus, and rectus abdominal; completely subpectoral, in which the implant lies beneath the pectoral muscle and is covered by pectoral fascia or by the adipose layer in the lower segment; and partly subpectoral, in which a part of the muscle will serve as coverage for the upper pole of the breast6,7.
Significant weight loss, pregnancy, prolonged breastfeeding, and involution of the mammary tissue after menopause are common causes of ptosis, which can be associated with hypomasty, leading to the desire for a combination of prostheses and mastopexy8.
The aim of this study was to evaluate a series of cases of mastopexy associated with mammary implants, in order to discuss complications associated with mammary implants, and the indications and complication rates among patients undergoing surgeries using the subglandular or submuscular techniques. Moreover, we discuss indications and strategies applicable to mastopexy with submuscular prostheses.
METHOD
This retrospective descriptive study reviewed the medical records of patients who underwent augmentation mammoplasty associated with mastopexy in the Plastic Surgery Unit of the Hospital Daher Lago Sul (Brasília, DF, Brazil). From July 2008 to July 2011, 243 patients underwent surgery: 149 using the subglandular technique and 94 using the submuscular technique. The mean age of the patients at the time of the surgery was 31.4 years, ranging from 17 to 63 years. All patients were preoperatively investigated using mammary ultrasonography and mammography, cardiology, and histopathological examination of the product of mammary resection.
General anesthesia was administered to 202 patients and patients epidural with morphine to 41. Implant volumes ranged from 150 mL to 400 mL.
The degree of satisfaction of both the surgeon and the patient with the final result was classified as good, limited, or bad, according to the technique used. Photographic records were also taken, and complication and reoperation rates were analyzed.
Description of the Technique
General anesthesia and/or an epidural with morphine for postoperative analgesia were usually used at our institution.
All patients underwent preoperative marking and either racket incision or classic Pitanguy technique, depending on the degree of ptosis and amount of excessive skin (Figure 2).

Figure 2 - Markings are made depending on the amount of excessive skin and degree of ptosis.
The criteria to indicate placement of implants in the submuscular plane were as follows: thin skin with a lot of stretch marks, patients with previous bariatric surgery, scarce mammary glands and adipose tissue, capsular contractures, or limited results with the subglandular technique and subsequent patient request.
Access to the retromammary area was achieved according to the Pitanguy technique, with vertical bipartition of the breast. In the cases of submuscular implants, a subpectoral zone was prepared with an oblique line in the direction of the fibers of the large pectoral muscle in the retroareolar area acting as an opening, over the 4th or 5th costal arch. Detachment of the subpectoral zone was performed by direct visualization and by using optic fiber and electric cauterization.
The key points of this technique are the complete separation of the medial insertion of the pectoral muscle at the sternal margin up to the 4th intercostal space and preservation of the prolongation of the fascial/adipose tissue, which maintains the connection between the dissected muscles and the thorax. With these maneuvers, mobility of the implant with activity of the pectoral muscle and possible upward dislocation is avoided. In addition, good coverage of the lower pole is allowed, since the muscles do not lose their connection to the ribs and sternum (Figures 3 and 4).
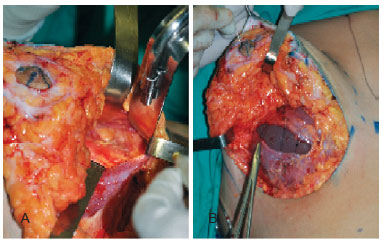
Figure 3 - In A, section of the medial insertion of the pectoral muscle up to the 4th costal arch. In B, implant surrounded by muscle.
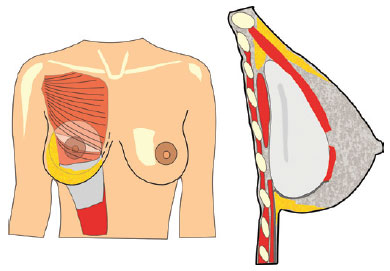
Figure 4 -Schematic representation of the placement and coverage of the implant. The dotted line indicates the level of muscle section.
A vacuum tube drain was placed in the submuscular area, with an exit hole in the axillary region. Round, textured, high-profile implants were used in most patients, while polyurethane was used in some of the cases. The area was closed by partially bringing together the margins of the large pectoral muscle by using nylon 3.0. At this point, the area was hermetically closed; however, in most cases, it is difficult to avoid compression of the prosthesis and laceration of the fibers of the large pectoral muscle. Therefore, the intention, instead, is to maintain the margins of the muscles in the position shown in Figure 5, until the process of wound healing allows the connection to be made definitively, and the implants remain surrounded by a pocket that will sustain them in the indicated position.
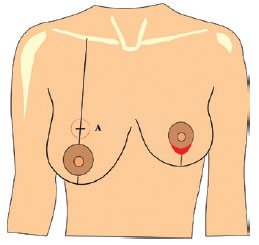
Figure 5 - Schematic representation of the difficulty of closure of the areola (in red), if the volume of the implant is inadequate. A = Pitanguy's point.
After inserting the submuscular prosthesis and joining together the separated margins of the pectoral muscle, assembly of the breast was performed in order to obtain a good cleavage. In the case of larger breasts, in which the prosthesis was aggregated to improve the cleavage, careful resection of the lower quadrants was performed, since otherwise excess tissue would result in pseudoptosis and undesirable results. After such resections, the medial and lateral pillars of the gland were assembled with nylon 3-0 to finish coverage of the implant not achieved using the pectoral muscle.
Elevation of the areolar-papillary complexes was performed using the upper (Pitanguy) or medial (Silveira Neto) pedunculus, depending on the demands of each case. The subcutaneous layer was closed using simple sutures of nylon 4-0, the deep subdermal layer was closed with nylon 5-0, and the intradermal layer was closed with a continuous suture of nylon 4-0.
RESULTS
The average duration of hospital stay was 24 h, and patients who underwent combined surgeries were discharged within 48 h. There were 174 cases of combined procedures: the most common being liposuction, followed by abdominoplasty.
One patient who underwent the subglandular technique had an anesthetic transoperative complication, when infusion of muscle relaxant in the cellular subcutaneous tissue after loss of venous access went unnoticed. The patient was transferred to the intensive therapy unit as a consequence of erratic absorption of the medication.
Three patients evolved with expansive hematoma in the immediate postoperative period, with reoperation being needed for drainage. Of these patients, 2 underwent the submuscular technique and 1 the subglandular technique. Two patients who underwent the surgery with the subglandular technique suffered from infection and extrusion of the prosthesis, which was treated with removal of the implant, antibiotic administration, and reoperation within 4-6 months, without complications. Four patients who underwent the subglandular technique developed capsular contracture (Baker's grade II), and 2 underwent reoperation in the submuscular plane. All the 7 cases of surgery with the submuscular technique showed pseudoptosis, with the breast sliding over the implant and the patient complaining that the prosthesis was too high. Four of these cases were not severe and 3 required reoperation. Fourteen patients who underwent surgery using the subglandular technique developed mammary ptosis; 5 of these underwent reoperation, with 2 changing to the submuscular plane. Eight patients who underwent the surgery using the submuscular technique complained of implant mobility with activity of the pectoral muscle (Figure 6). One of these patients underwent reoperation by request, and a double plane technique was used the second time.

Figure 6 - Mobility of the implant with activity of the pectoral muscle.
The reoperation rate was 6.58%. No cases of prosthesis dislocation were observed.
During outpatient follow-up on postoperative days 3, 7, 14, 30, 90, 180, and 360, there were 19 cases of seroma, which resolved by spontaneous drainage or reabsorption without the need for puncture. Two patients had stretch marks on the breasts, which were partially cleared by chemical exfoliation. There was 1 case of partial necrosis of the areolar-papillary complex, where the technique of Silveira Neto had been used, and was treated with pigmentation. In 1 patient, there was persistent paresthesia in the areolas after 6 months of follow-up. Seven cases of partial dehiscence were observed, without exposure of the implants. Of these, 2 were treated with re-synthesis and 5 with a second intention wound healing. Twenty-seven patients evolved with scar hypertrophy, which was treated using silicone tape and/or triamcinolone infiltration.
Figures 7 to 10 show the degree of satisfaction of the surgeon and the patients, according to the technique employed.
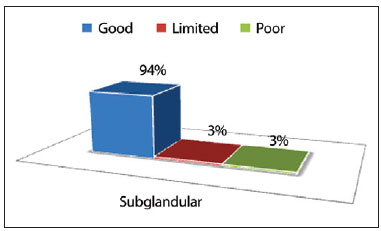
Figure 7 - Degree of satisfaction of the surgeon, by using the subglandular technique.
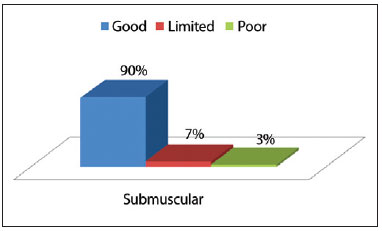
Figure 8 - Degree of satisfaction of the surgeon, by using the submuscular technique.
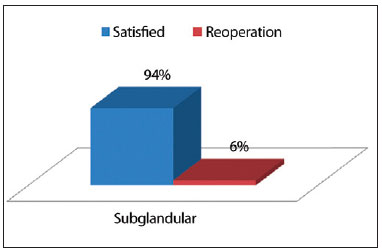
Figure 9 - Degree of satisfaction of the patient, by using the subglandular technique.
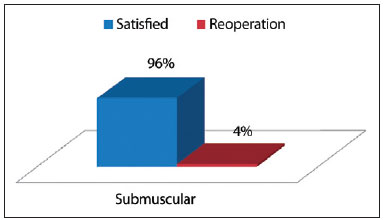
Figure 10 - Degree of satisfaction of the patient, by using the submuscular technique.
DISCUSSION
The options for breast surgery faced by plastic surgeons daily are as follows:
augmentation mammoplasty with subglandular implants; augmentation mammoplasty with submuscular implants; mastopexy associated with augmentation mammoplasty with subglandular implants; and mastopexy associated with augmentation mammoplasty with submuscular implants.
At our unit, augmentation mammoplasties and hypomasties are corrected with subglandular or subfascial implants, leading to a more natural look. In serious hypomasties, where there is not much gland, skin, and subcutaneous tissue, subpectoral implants are indicated, based on our experience in mammary reconstructions with little coverage tissue. When mastopexy associated with silicone implants is indicated, we use subglandular implants, whenever possible, believing that a more natural appearance is achieved when the implant is smaller than the existent mammary gland.
Difficulties
If the implant is large and voluminous and the tissue is fragile and thin, there may be dislocation of the implant with deterioration of the predefined shape, falling, and lateral dislocation, amongst other complications (Figure 11).

Figure 11 - A patient with large implants showing fall and lateral dislocation (subglandular technique).
Submuscular implants associated with mastopexy are reserved for patients with little dermoglandular tissue that would not support the newly created mammary cone. The subpectoral implant fixes the implant in a defined position in the anterior thoracic wall, without dislocation. In this way, a new skin and dermoglandular tissue "bra" is created over the muscle fascia pocket, with a stable shape and volume (Figure 12). Although this appears to be a logical option, there are several complications that must be considered and prevented.
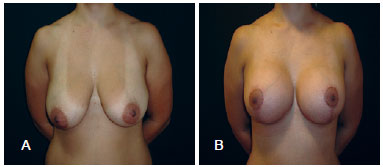
Figure 12 - In A, preoperative appearance of a patient with large ptotic breasts. In B, postoperative appearance after mastopexy associated with submuscular silicone implants, showing shape maintenance and the absence of dislocations.
1. The gland may slide over the implant (which will remain stable and surrounded by the capsule behind the pectoral muscle), making the breasts hang on the volume of the silicone. This happens when the gland is very large and heavy (Figure 13). To avoid this situation, the glandular tissue must be emptied, similarly to adenomastectomy, and the volume of the new breast will effectively be the volume of the implant.
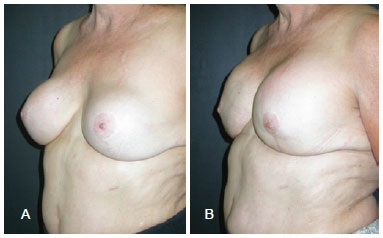
Figure 13 - In A, preoperative appearance of a patient with large and heavy breasts. In B, postoperative appearance after mastopexy with limited parenchyma resection, showing sliding of the parenchyma over the prosthesis in the submuscular plane.
2. Bad positioning of the areola must be avoided by marking it in a higher position, while respecting the marking principles of Pitanguy's point "A." Anatomical distance between the clavicle and point "A" must be maintained. If this measurement is too long or the mammary cone is not proportional, there will be a tendency for falling into the subglandular implants or ptosis of the mammary parenchyma over the implant (pseudoptosis) (Figure 14).
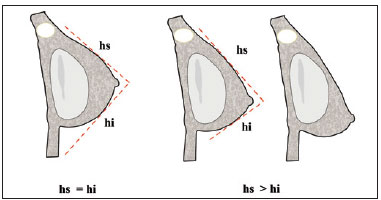
Figure 14 - Schematic representation of the correct placement of the areola, in which hs = hi and sliding of point A next to the parenchyma causes hs > hi. hi = inferior length of the new mammary cone; hs = superior length of the new mammary cone.
3. Difficulties in assembly of the breast and synthesis of the tissues can occur, since closure of the original area of the areola is a limiting factor to the volume of the implant that can be used. This must be previously evaluated by the surgeon and discussed with the patient. Non-observance of this rule will make closure of the original area of the transposed areola difficult, leading to artificial results (retractable belts in the middle of the breast and dehiscence)(Figure 5).
It is known that flat implants, subglandular implants, and the presence of bacteria over the implant (subclinical infections) are associated with a larger incidence of capsular contracture, but there is doubt as to whether submuscular implants have lower rates of capsular contracture, since better tissue coverage would hide this complication6,9-13. The submuscular plane may be associated with more postoperative pain, more hematomas, and mobilization or dislocation of the implants with muscle activity9,14. These possible complications may be circumvented with better postoperative analgesia, routine use of vacuum drains, and appropriate detachment of the large pectoral muscles.
Thin patients who lack coverage in the upper pole of the breasts, those who might have breastfed for long periods, those with thin skin of bad quality and a lot of stretch marks, patients of older age, ex-obese patients who have undergone large weight losses and lipodystrophies, and those who present with prostheses with capsular contracture and spontaneously request the technique are best indicated for the submuscular technique6-8,15.
In ex-obese patients and in those with lipo-substituted breasts, amputation of the lower segment of the breast is indicated to avoid possible early ptosis with the "double breast" effect. Patients with familial or previous history of breast cancer, histological risk factors, and mutations of the BRCA 14 genes and those with pronounced ptosis are indicated for mastology16; in these patients, we perform an amplified resection of the mammary tissue (subcutaneous adenomastectomy) and avoid the sliding of the remaining mammary tissue over the prosthesis, thereby resulting in a final aesthetic result. The size and shape of the mammary implant is usually accepted by the patients and ensures more durable results.
CONCLUSIONS
Treatment of mammary ptosis associated with augmentation mammoplasty demands complex technical combinations and careful preoperative analysis to define the best techniques to be used, which decreases the need for surgical revision and allows stable, long-lasting, and harmonious results.
REFERENCES
1. Disponível em:
2. Pesquisa Datafolha encomendada pela Sociedade Brasileira de Cirurgia Plástica. Disponível em:
3. Michalopoulos K. The effects of breast augmentation surgery on future ability to lactate. Breast J. 2007;13(1):62-7.
4. Spear SL, Low M, Ducic I. Revision augmentation mastopexy: indications, operations, and outcomes. Ann Plast Surg. 2003;51(6):540-6.
5. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67.
6. Hendricks H. Complete submuscular breast augmentation: 650 cases managed using an alternative surgical technique. Aesthetic Plast Surg. 2007;31(2):147-53.
7. Tebbetts JB. Dual plane breast augmentation: optimizing implant-softtissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118(7 Suppl):81S-102S.
8. De Benito J, Sánchez K. Key points in mastopexy. Aesthetic Plast Surg. 2010;34(6):711-5.
9. Henriksen TF, Fryzek JP, Hölmich LR, McLaughlin JK, Kjøller K, Høyer AP, et al. Surgical intervention and capsular contracture after breast augmentation: a prospective study of risk factors.Ann Plast Surg. 2005;54(4):343-51.
10. Embrey M, Adams EE, Cunningham B, Peters W, Young VL, Carlo GL. A review of the literature on the etiology of capsular contracture and a pilot study to determine the outcome of capsular contracture interventions. Aesthetic Plast Surg. 1999;23(3):197-206.
11. Del Pozo JL, Tran NV, Petty PM, Johnson CH, Walsh MF, Bite U, et al. Pilot study of association of bacteria on breast implants with capsular contracture. J Clin Microbiol. 2009;47(5):1333-7.
12. Biggs TM,Yarish RS. Augmentation mammaplasty: retropectoral versus retromammary implantation. Clin Plast Surg. 1988;15(4):549-55.
13. Collis N, Coleman D, Foo IT, Sharpe DT. Ten-year review of a prospective randomized controlled trial of textured versus smooth subglandular silicone gel breast implants. Plast Reconstr Surg. 2000;106(4):786-91.
14. Lesavoy MA, Trussler AP, Dickinson BP. Difficulties with subpectoral augmentation mammaplasty and its correction: the role of subglandular site change in revision aesthetic breast surgery. Plast Reconstr Surg. 2010;125(1):363-71.
15. Spear SL, Carter ME, Ganz JC. The correction of capsular contracture by conversion to "dual-plane" positioning: technique and outcomes. Plast Reconstr Surg. 2003;112(2):456-66.
16. Hoover DJ, Paragi PR, Santoro E, Schafer S, Chamberlain RS. Prophylactic mastectomy in high risk patients: a practice-based review of the indications. Do we follow guidelines? Breast Dis. 2010;31(1):19-27.
1. Head of the Plastic Surgery Unit of the Hospital Daher Lago Sul, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society for Plastic Surgery) - SBCP, Brasília, DF, Brazil.
2. Preceptor of the Plastic Surgery Unit of the Hospital Daher Lago Sul, full member of the SBCP, Brasília, DF, Brazil.
3. Resident of the Plastic Surgery Unit of the Hospital Daher Lago Sul, aspiring member of the SBCP, Brasília, DF, Brazil.
Correspondence to:
José Carlos Daher
SHIS QI 8 cj. 8 - casa 19 - Lago Sul
Brasília, DF, Brazil - CEP 71600-500
E-mail: daher@hospitaldaher.com.br
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 31, 2012
Article accepted: June 7, 2012
Work carried out at the Plastic Surgery Unit of the Hospital Daher Lago Sul, Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter